BIO uW: Digestion & musculoskeleton Flashcards
Long bone structure
Epiphyses
diaphysis
metaphysis
- Epiphyses (rounded ends covered by articular cartilage)
- Diaphysis (shaft containing the medullary cavity filled with yellow bone marrow)
- Metaphysis (where the diaphysis and epiphyses meet).

Red & yellow bone marrow

Skeletal system functions

Example of osteoarthritis & osteoporosis

Cellular bone composition
Compact bone
Cartilage
- Compact bone is organized into concentric rings of bone matrix called lamellae. The entire unit of concentrically arranged lamellae surrounding a central haversian canal is known as an osteon, or a haversian system.
- Within each osteon, lacunae (spaces containing osteocytes) connect to one another via microscopic channels called canaliculi, which allow osteocyte waste exchange and nutrient delivery.
- Chondrocytes make up the cellular component of cartilage, NOT BONE

Cartilage
- Cartilage is a firm but flexible connective tissue that lacks blood vessels and nerves.
- Chondrocytes (cartilage cells) secrete chondrin, which is the specialized extracellular matrix that makes up cartilage.
- The most common type of cartilage is hyaline cartilage, which plays a role in bone development and lines the ends of articulating bones.
- ribs, nose, trachea & larynx

Tendons & ligaments
- Ligaments and tendons are important connective tissue structures at joints.
- Tendons tautly anchor muscle to bone. Tendons are strong, fibrous bands of connective tissue that transmit a force generated by contracting muscle to the bone, permitting locomotion (movement).
- Ligaments are strong bundles of connective fibers that connect bones to other bones and stabilize and hold structures together.
Reporter Genes
Gene Regulation
- A reporter gene allows researchers to study the regulation or expression of other genes.
- The luciferase gene is a commonly used reporter gene whose protein product catalyzes a reaction that results in bioluminescence, which allows easy expression quantification of the target gene.

Coding & noncoding RNA

Which organ synthesizes a compound that facilitates the mechanical digestion of lipids?
- LIVER
- Bile is synthesized in the liver, stored in the gallbladder, and released into the duodenum to aid lipid digestion.
- Bile salts, a key component of bile, mechanically digest lipid globules by physically breaking them down into smaller droplets in a process known as emulsification.
- Subsequently, pancreatic lipase chemically digests emulsified lipids.

What is bile composed of?
- bile salts, bile pigments (eg, bilirubin), and cholesterol
Emulsification
- Emulsification is an example of mechanical digestion, which physically breaks down food particles into smaller pieces.
- (Additional examples of mechanical digestion include chewing in the mouth and churning in the stomach due to peristaltic waves.)
Bile Salts
- act as detergents to solubilize fats during digestion and possess both a hydrophobic region that associates with the surface of lipids and a hydrophilic region that associates with water. Consequently, bile salts break down large lipid globules into smaller droplets (micelles) in a process known as emulsification.
gallbladder
stores bile
salivary glands
lingual lipases
salivary amylase
- are exocrine glands in the mouth that secrete saliva, a lubricating fluid that contains the enzymes lipase and amylase
- Lingual lipase facilitates the chemical, not mechanical, digestion of lipids.
- In contrast, salivary amylase hydrolyzes (chemically digests) the polysaccharide starch into the disaccharide maltose.
Exocrine glands

Neutralization of chyme in the small intestines

acidic enviroment of the stomach
- The acidic pH of the stomach is maintained by gastric juice, which is primarily composed of hydrochloric acid (HCl).
- This acidic environment is required for protein digestion and to kill harmful bacteria.
- When gastric juice mixed with food (chyme) enters the duodenum, it is neutralized by bicarbonate ions (from the pancreas) and bile (released from storage in the gallbladder).

Large intestines structures & functions

Gastric bypass

Stomach cells
- The cells in the stomach secrete the following: gastrin (from G cells) signals parietal cells to secrete HCl (from parietal cells); pepsinogen (from chief cells) cleaves polypeptides when activated by HCl; and mucus (from mucous cells) and bicarbonate (from epithelial cells) protect the stomach lining against autodigestion by gastric juice.

Peritonium
- is composed of two membranes that line the abdomen: the parietal layer, which lines the abdominal wall, & visceral layer, which covers the abdomindal organs
- the peritoneal cavity: is a potential space between the partietal & visceral laters of the peritonium

Body contains 4 types of tissues

subtypes of connective tissue
- bone: which makes up the skeletal system and provides structural support and physical protection for internal organs as well as a framework for mobility. Bone comprises osteoblasts (matrix-secreting cells that build bone), osteoclasts (bone-degrading cells), and osteocytes (mature bone cells)
- blood: which transports gases, cells (ie, erythrocytes, leukocytes), nutrients, wastes, and other materials (eg, hormones) throughout the body via blood vessels. Although mature erythrocytes have no nucleus, gene expression profiles can still be obtained from leukocytes
- adipose tissue: which is responsible for the storage of fats as well as providing cushioning for organs and insulation to prevent heat loss

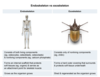
Endoskeleton vs exoskeleton
- The vertebrate endoskeleton is composed of both bone and cartilage and provides an internal scaffold that facilitates mobility while protecting and supporting internal organs.
- In contrast to vertebrates, many invertebrate animals possess an external skeleton (exoskeleton), which is a rigid outer covering that serves to protect the soft tissues underneath.
ligament
connects two bones

Joints
- are structures of the musculoskeletal system where bones articulate (ie, interact) and can range in mobility from freely moveable to immoveable.
- Within moveable joints, strong connective tissue structures called tendons attach muscle to bone whereas ligaments attach bone to bone.
Functions of the GI tract

Sacroplasmic reticulum
Muscle relaxtion & contraction
- The sarcoplasmic reticulum (SR) is a muscle fiber organelle that tightly regulates intracellular calcium (Ca2+) concentration.
- The release of calcium from the SR promotes muscle fiber contraction whereas the transport of calcium into the SR promotes and maintains muscle fiber relaxation.

Muscle fibers & sarcromeres

Cellular respiration & fermentation
Aerobic (O2) respiration

Cellular respiration & fermentation
Anaerobic (no O2) respiration

myoglobin & hemoglobin
- iron facilitates oxygen binding proteins myoglobin & hemoglobin
- Myoglobin stores oxygen within muscle fibers, and hemoglobin is an oxygen carrier molecule found in red blood cells that allows oxygen to be transported throughout the body.

muscle fibers primarily generate ATP through:
- glucose metabolism
Division of the nervous system

ACH breakdown & synthesis

Neuromuscular junction function
- the basic function of the NMJ is to convert a motor neuron action potential into a muscle fiber action potential
- Acetylcholine (ACh) degradation within the neuromuscular junction is one process by which muscle fiber contraction is terminated.
- However, decreased ACh degradation would allow more ACh molecules to remain in the synapse and prolong stimulation of nAChR and subsequent muscle contraction.

Relationship among experimental variables

transverse tubule
- Electrical depolarization caused by action potential propagation leads to the contraction of skeletal muscle fibers.
- As extensions of the plasma membrane that penetrate deep into muscle fibers, transverse (T) tubules are specialized muscle fiber structures that facilitate action potential propagation throughout individual muscle fibers
- (in neurons, action potential propagation occurs along the axon. the analogous structure in skeletal muscle fibers that enables action potential propagation is the transverse tubule)

a decrease in what will result in lowered blood pressure?
- Angiotensin II, antidiuretic hormone, and aldosterone all regulate blood pressure.
- Angiotensin II of the RAS pathway, aldosterone, and ADH are hormones that cause blood pressure to increase. Accordingly, a decrease in RAS activation, ADH secretion, or aldosterone production would cause BP to fall.
- The effect of these hormones on blood pressure can be explained wholly or in part by the modulation of water and salt reabsorption in the kidneys
- each explained in a seperate card

Blood pressure
- the force blood exerts on blood vessel walls, decreases when blood vessels dilate (become wider) or when blood volumedecreases. Hormones such as angiotensin II, aldosterone, and antidiuretic hormone (ADH; vasopressin) regulate BP by modulating the kidney’s reabsorption of water and salts.
- image shows regulating blood pressure by the kidney

RAS: renin-angiotensin system
- is a multi-organ molecular cascade activated when BP (or blood volume) falls.
- A drop in BP causes the juxtaglomerular cells in the kidneys to release renin, an enzyme that cleaves the plasma protein angiotensinogen to form angiotensin I.
- Angiotensin-converting enzyme (ACE) then cleaves angiotensin I to form angiotensin II.
- Angiotensin II ultimately raises BP by inducing both the release of aldosterone from the adrenal cortex (increasing BP by increasing blood volume through water retention) and the constriction of arterioles (increasing BP without changing blood volume)
ALDOSTERONE
- is released in response to RAS activation or to an increased serum level of K+.
- Aldosterone acts on the distal tubules and collecting ducts of nephrons to promote the reabsorption of Na+ and the secretion of K+.
- Increased reabsorption of Na+increases the osmolarity, or solute concentration, of the renal interstitial fluid.
- Elevated osmolarity promotes water reabsorption, which ultimately causes blood volume and BP to increase
ADH
- is released by the posterior pituitary when BP falls or when blood osmolarity rises.
- ADH promotes water reabsorption by increasing the permeability of the distal tubule and collecting duct to water.
- ADH also induces vasoconstriction, the narrowing of blood vessels.
- Both of these effects increase BP
Urine Storage**
- Urine flows from the kidney to the bladder through the ureter. Once the bladder is full, urine exits the body via the urethra through the process of urination. Urination is controlled by the detrusor muscle (smooth muscle lining of the bladder), the internal urethral sphincter, and the external urethral sphincter.
- The detrusor and IUS are under involuntary control; the EUS is under voluntary control.
- During urination, activity within stretch receptors in the bladder leads to:
- Contraction of the detrusor muscle, which pushes urine out of the bladder and into the urethra.
- Relaxation of the IUS, which opens the urethra and allows urine to pass.
- Nerve damage that impairs the contraction of the detrusor muscle of the bladder would impair emptying of the bladder and lead to urinary retention.
- when contracted IUS & EUS block urine flow through the urethra (inability to contract these muscles will facilitate urine flow)

Pressures of the glomerulus of the nephron
Hydrostatic pressure and osmotic pressure are two opposing forces that regulate fluid movement between capillaries and the tissues that surround them.
- Hydrostatic pressure is the force exerted by a liquid on the walls of its container. Accordingly, the hydrostatic pressure of blood, or blood pressure (BP), is the force exerted by blood on the vessel walls. This pressure pushes fluid through capillary wall pores and into the interstitial fluid (the extracellular fluid surrounding cells of a tissue). The kidneys regulate BP by increasing water reabsorption (thereby increasing blood volume and, consequently, BP) when BP is low and by decreasing water reabsorption when BP is high.
- Osmotic pressure causes a solution to take in water by osmosis, the passive movement of water molecules from an area of low to an area of high solute concentration. Osmotic pressure increases as solute concentration (osmolarity) increases. When blood osmolarity is high, the kidneys respond by increasing water reabsorption and decreasing solute reabsorption. Conversely, when blood osmolarity is low, the kidneys react by decreasing water reabsorption and increasing solute reabsorption.

If sodium/glucose transporter is blocked in proximal tubule (such as administration of a SGLT inhibitor), what will happen?
—–>prevents glucose reabsorption, increasing solute concentration within the tubule and consequently increasing the osmotic pressure of the tubular filtrate. As a result, water is drawn back into the renal tubule, increasing urine output.
reabsorption & secretion of substances along the nephron

proximal tubule:
In this segment, important nutrients (eg, amino acids, vitamins, salts, glucose, water) are reabsorbed from the nephron and incorporated back into the blood through the peritubular capillaries that surround the tubule. Waste products not filtered by Bowman’s capsule are actively secreted from the peritubular capillaries into the nephron.
loop of henle
- This segment is a hairpin structure composed of two limbs:
- The descending limb extends down into the relatively salty medulla (inner portion of the kidney) and is permeable to water, allowing the passive reabsorption of water via osmosis
- The ascending limb transports filtrate out of the medulla and back to the cortex (outer portion of the kidney). This limb is permeable to salt but impermeable to water; this leads to active reabsorption of ions only, which concentrates the medullary interstitial fluid (maintains its saltiness) and prevents its dilution.

Distal tubule:
Antidiuretic hormone (ADH; vasopressin) and aldosterone promote the reabsorption of water in this segment of the tubule. Additional waste products are secreted into the nephron from the peritubular capillaries.
Collecting duct
- ADH and aldosterone act on the collecting duct in the same way they act on the distal tubule. The now-concentrated urine is emptied into the ureters for excretion.
Bone remodeling
-
Bone remodeling is a continuous process in which osteoclasts (bone-resorbing cells) break down old bone and osteoblasts (bone-depositing cells) secrete new bone matrix. This process functions to maintain the strength and integrity of bone over time.
- Osteoblasts promote the precipitation of calcium and phosphate from the bloodstream and their transfer and incorporation into the bone matrix. In contrast, osteoclasts secrete acids that break down the mineral components of bone, releasing calcium and phosphate into the bloodstream.

Another form of bone remodeling

transcription factors
have nuclear localization sequences that facilitate their entry into the nucleus, where they regulate the expression of target genes

Effect of PTH on bone

- To regulate calcium homeostasis, parathyroid hormone (PTH) and calcitonin act antagonistically to each other.
- PTH is secreted in response to low blood calcium levels and stimulates bone resorption by osteoclasts, causing an increase in blood calcium.

Calcitonin

Muscle types

Sliding filament model of muscle contraction
- When ATP bound to a myosin head hydrolyzes, the myosin head shifts back and attaches to the actin filament.
- Dissociation of ADP and Pi leads to a power stroke, which shortens the sarcomere.
- A new ATP molecule binds to the myosin head, causing it to dissociate from the actin filament.
- The action of many myosin heads cycling through this process leads to muscle contraction.

3 types of muscle fibers
- Their contractile speed (fast or slow): Contractile speed is determined largely by the catalytic speed of the myosin ATPase and the activity of the associated motor neuron at the neuromuscular junction.
- Their primary means of producing ATP (oxidative or glycolytic): To generate ATP, oxidative fibers use aerobic respiration, but glycolytic fibers use anaerobic glycolysis.
-
Summary:
- Skeletal muscle fibers can be classified as type 1 (slow oxidative), 2A (fast oxidative-glycolytic), or 2X (fast glycolytic).
- The speed of contraction (slow or fast) is determined by the catalytic speed of the myosin ATPase and the activity of the fiber’s associated motor neuron.
- Oxidative fibers are fatigue resistant and synthesize ATP through aerobic respiration (oxygen-requiring pathways).
- Glycolytic fibers are easily fatigable and generate ATP through anaerobic glycolysis (in the absence of oxygen)

Oxygen Debt (excess post-exercise oxygen consumption EPOC)
- Oxygen intake remains elevated after exercise due to the increased demand in muscle cells for oxygen to replenish ATP, creatine phosphate, and glycogen stores and restock myoglobin with oxygen.
- The amount of additional oxygen consumed is called the excess post-exercise oxygen consumption, or oxygen debt.

Transcription factors
- Transcription factors are translated in the cytoplasm but act in the nucleus to control gene expression.
- They contain a nuclear localization sequence that allows nuclear import proteins to direct them back to the nucleus to alter gene transcription.
ELISA
- Enzyme-linked immunosorbent assay (ELISA) can detect and quantify proteins.
- Initially, a primary antibody (linked to a “reporter” enzyme) is added, which binds the antigen (protein). The samples are washed to remove unbound proteins, and the reporter enzyme substrate is added.
- The enzyme-substrate reaction creates a product that results in a quantifiable/detectable signal.

Countercurrent muliplication in the loop of henle

activity of mitochondrial enzyme in nonoxidative & oxidative muscle fibers
- Oxidative muscle fibers use aerobic respiration for ATP synthesis, requiring large amounts of oxygen supplied by high levels of myoglobin and extensive capillary networks.
- In contrast, nonoxidative fibers generate ATP through anaerobic glycolysis and require less oxygen than oxidative fibers.

- Dehydration caused by frequent loose stools is often observed in patients with certain diseases of the gastrointestinal (GI) tract. Given this, which of the following treatments would be most effective in treating this symptom?
- Answer: use of drugs that decrease the luminal secretion of chloride ions from intestinal epithelial cells

Sarcromere lenght influences contractile force



