Anato Flashcards
What are the 7 layers of the anterior abdominal wall?
- Skin
- Superficial fascia
- Fatty superficial layer (Camper’s fascia)
- Deep membranous layer (Scarpa’s fascia)
- Deep fascia
- Anterolateral wall muscles
- Transversalis fascia
- Extraperitoneal fatty tissue
- Peritoneum

External oblique muscle?
Fibbers orientation: Hands in pocket (sexternal)
Origin: Ribs 5-12
Insertion: Iliac crest, pubic crest, linea alba and xyphoid process –> forms inguinal ligament
Function: Anterior and lateral flexion of vertebral column

Internal oblique muscle?
Fibbers orientation: Hands on tits (seinterne)
Origin: Iliac crest and lateral part of inguinal ligaments
Insertion: Ribs 9-12 and linea alba
Function: Anterior and lateral flexion of vertebral column

Tranversus abdominis muscle?
Fibbers orientation: Horizontally
Origin: Iliac crest and lateral/upper part of inguinal ligament
Insertion: Linea alba and public crest
Function: Anterior and lateral flexion of vertebral columm

Rectus abdominis muscle?
Fibbers orientation: vertically
Origin: Pubic symphysis and crest
Insertion: Costal margin and xyphoid procress –> becomes pyramidalis muscle
Function: Anterior flexion of the vertebral column

What is the arcuate line?
Is the lower edge of posterior sheath of rectus abdominis. The transversalis fascia is directly posterior to rectus abdominis muscle below the arcute line while before the arcuate line, the rectus was between the anterior and posterior fascias of the internal oblique (IO).

Arterial supply of the anterior abdominal wall?
- Superior epigastric a. –> from internal thoracic a.
- Deep circumflex iliac a. –> from external iliac a.
- Inferior epigastric a. –> from external iliac a.
- Superficial epigastric a. –> from femoral a.

Venous drainage of the anterior abdominal wall?
Deep
- Superior epigastric v. –> to internal thoracic v.
- Deep circumflex iliac v. –> to external iliac v.
- Superficial circumflex iliac v. –> to femoral v.
- Inferior epigastric v. –> to external iliac v.
Superficial
- Thoraco-epigastric v. –> to axillary v.
- Superficial epigastric v. –> to femoral v.
Two important nerves of the pubic region?
- Iliohypogastric nerve: pierces the aponeurosis of the external abdominal oblique muscle 3-5 cm above the superficial inguinal ring
- Ilioinguinal nerve: emerges from the superficial inguinal ring and passes on the surface of the spermatic cord (or round ligament).

Layers of the inguinal canal?
From superficial to deep:
- Skin
- Dartos
- External spermadic fascia (from external oblique muscle)
- Cremaster muscle (from internal oblique muscle)
- Internal spermadic fascia (from traversalis fascia)
- Tunica vaginalis parietal
- Tunica vaginalis visceral

Ligaments of the inguinal canal?
- Cooper’s ligament: extension of the lacunar ligament that runs on the pectineal line of the pubic bone.
- Conjoint tendon: derived from fusion of the aponeuroses of the transversus abdominis and internal oblique muscles. On each side, it inserts into the pubic crest in continuity with the pectineal line. It forms the medial reinforcement to the posterior wall of the inguinal canal.
- Lacunar ligament: as the inguinal ligament reaches the pubic tubercle, it reflects backward and lateralward to attach to the pectineal line for about 1.25 cm. This posterior projection of the inguinal ligament is called the lacunar ligament.

What is the difference between a direct and indirect hernia?
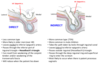
Inguinal Triangle Hesselbach’s Triangle?
- Medial border = Lateral margin of the rectus abdominis muscle/sheath
- Superolateral border = Inferior epigastric vessels
- Inferior border = Inguinal ligament (Poupart’s ligament)

Name those lines
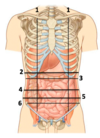
- Midclavicular (or midinguinal) line
- Transpyloric plane
- Subcostal plane
- Transumbilical plane
- Intertubercular plane
- Interspinous plane
Name these

Name the content of the 4 quadrants
Right upper quadrant
Liver and Gallbladder
Left upper quadrant
Stomach and spleen
Right lower quadrant
Cecum, appendix, ascending colon & small bowel
Left lower quadrant
Descending and sigmoid colon & Small bowel
Name the 9 abnominal regions

Intraperitoneal Organs?
- Liver
- Stomach (ST)
- Spleen
- Duodenum (1st and 4th parts)
- Small intestines (SI)
- Cecum
- Appendix
- Transverse colon (TC)
- Sigmoid colon
- Rectum (upper 1/3)
- Fallopian tubes/ovaries
Retroperitoneal Organs?
Primarily retroperitoneal:
- Adrenal glands, kidneys, ureter, bladder
- Aorta, inferior vena cava
Secondarily retroperitoneal organs:
- Head and neck of the pancreas (but not the tail)
- Second and third portions of the duodenum (but not the first or fourth)
- Ascending and descending portions of the colon (but not the transverse or sigmoid)
Name the different Mesentaries and Omenta
- Lesser omentum - stabilizes the position of the stomach and provides an access route for blood vessels and other structures entering or leaving the liver.
- Greater omentum - hangs like an apron from the lateral and inferior borders of the stomach.
- Mesentery proper - a thick mesenterial sheet that provides stability to the small intestine, but permits some independent movement.
- Transverse mesocolon - supports the transverse colon, extending from pancreas on the posterior wall to the transverse colon.
- Sigmoid mesocolon - supports the sigmoid colon.

What are the lesser sac ligaments?
Gastrocolic ligament (GC) - a portion of the greater omentum (GO) that stretches from the greater curvature of the stomach to the transverse colon. It forms part of the anterior wall of the lesser sac.
Lesser omentum (LO) (two parts):
1) Hepatogastric ligament (HG) - connects the liver to the lesser curvature of the stomach.
2) Hepatoduodenal ligament (HD) - connects the liver (porta hepatis) to the duodenum. It contains the proper hepatic artery, hepatic portal vein, common bile duct (portal triad).
Ligaments of the liver?
- The falciform ligament (falciform in Latin = “sickle-shaped”) is a ligament that attaches the liver to the anterior body wall. It is a broad and thin antero-posterior peritoneal fold.
- The ligamentum teres is a remnant of the umbilical vein of the fetus.
- Triangular ligament

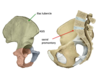
Identify these structures

The external sphincter of the stomach comes from where?
The right crus of the diaphragm. Function: sphincter that prevents stomach contents from refluxing up the esophagus when intra-abdominal pressure rises during inspiration



















