Acute myocardial infarction/ACS Flashcards
What is acute coronary syndrome?
umbrella term covering a number of acute presentations of ischaemic heart disease, including:
- ST elevation myocardial infarction (STEMI)
- Non-ST elevation myocardial infarction (NSTEMI)
- Unstable angina
What is meant by ischaemic heart disease?
synonymous with coronary heart disease; gradual build up of fatty plaques within walls of coronary arteries
What are the 2 main problems associated with fatty plaques deposited in the walls of the coronary arteries in ischaemic heart disease?
- Gradual narrowing: less blood + therefore oxygen to myocardium at times of increased demand → angina
- Risk of sudden plaque rupture: plaques in endothelium may rupture causing sudden occlusion of the artery → no blood/oxygen reaching the area of myocardium
What is angina?
chest pain due to insufficient oxygen reaching the myocardium during exertion
What are 3 unmodifiable risk factors for ischaemic heart disease?
- Increasing age
- Male gender
- Family history
What are 5 modifiable risk factors for ischaemic heart disease?
- Smoking
- Diabetes mellitus
- Hypertension
- Hypercholesterolaemia
- Obesity
What are 6 stages to the pathophysiology of ischaemic heart disease?
- Initial endothelial dysfunction triggered by factors e.g. smoking, HTN, hyperglycaemia
- Results in changes to endothelium: pro-inflammatory, pro-oxidant, proliferative and reduced nitric oxide bioavailability
- Fatty infiltration of subendothelial space by low-density lipoprotein (LDL) particles
- Monocytes migrate from blood and idfferentiate into macrophages: phagocytose oxidised LDL, turning into large ‘foam cells’. As they die can propagate inflammatory process
- Smooth muscle proliferation and migration from tunica media into intima results in formation of fibrous capsule covering fatty plaque

What can result if the plaque within a coronary artery ruptures?
can cause complete occlusion of coronary artery which may result in myocardial infarction

What are 5 key symptoms of acute coronary syndrome?
- Chest pain
- Dyspnoea
- Sweating
- Nausea and vomiting
- Palpitations
How is the chest pain of ACS typically described?
- central/left-sided
- may radiate to jaw or left arm
- often described as ‘heavy’ or ‘constricting’, ‘like an elephant on my chest’
- but can be wide variety of types of chest pain
What are 2 examples of groups of patients who may not experience any chest pain in ACS?
- Diabetics
- Elderly patients
What may observations (vital signs) show in a patient with ACS?
pulse, BP, temperature and oxygen sats often normal or only mildly altered e.g. tachycardia
What may be seen on examination in patients with ACS?
- if complication has developed e.g. cardiac failure - signs of this
- pale, clammy
What are the 2 most important investigations when assessing a patient with chest pain?
- ECG
- Cardiac markers e.g. troponin
What are the 5 broad groups of territories affected by ACS and the corresponding ECG leads and arteries?
- Anterior: V1-V4: left anterior descending artery
- Inferior: II, III, aVL: right coronary artery
- Anterolateral: V4-6, I, aVL: left anterior descending or left circumflex
- Lateral: I, aVL ± V5-6: left cicumflex artery
- Posterior: tall R waves, V1-2: left circumflex, right coronary
(also new LBBB anywhere)

How do the LAD, right coronary and left circumflex arteries relate to each other?
left coronary artery and right coronary artery arise from the ascending aorta
left coronary artery splits into left anterior descending and left circumflex

What are the 3 aims of treatment of ACS?
- Prevent worsening of presentation (further occlusion of coronary vessel)
- Revascularise the vessel if occluded (patients with STEMI)
- Treat pain
What is the commonly taught mnemonic for the treatment of ACS generally?
MONA:
Morphine IV (±anti-emetic) - only if severe pain
Oxygen (if sats <94)
Nitrates
Aspirin (300mg, often given pre-hospital)
For patients who have presented with STEMI, what are 3 additional aspects of the management as well as MONA?
- Second antiplatelet drug shoudl be given in addition to aspirin - options include clopidogrel, prasugrel and ticagrelor
- PCI (percutaneous coronary intervention)
- Before PCI introduced, thrombolysis with clot-busting drug was used to break down the thrombus
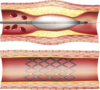
What does PCI involve?
catheter inserted into either radial or femoral artery; blocked arteries opened up using a balloon (angioplasty) folowing whcih a stent may be deployed ot prevent the artery occluding again in the future
If a patient presents with NSTEMI (no ST elevation on ECG) what are 2 steps that can be taken to determine further management (in addition to MONA)?
- Risk stratification tool such as GRACE can be used to decide upon further management
- If considered high-risk or clinically unstable, coronary angiography performed during admission
- if lower risk, patient can have coronary angiogram at later date
What are 5 types of medications that patients are prescribed lifelong following ACS to reduce risk of a further event?
- Aspirin
- Second antiplatelet if appropriate (e.g. clopidogrel)
- Beta-blocker
- ACE-inhibitor
- Statin
What is the name of the system used to stratify risk post-myocardial infarction?
GRACE (Global Registry of Acute Coronary Events) score
What are 9 poor prognostic factors in acute coronary syndrome according to the GRACE score?
- Age
- Development (or history) or heart failure
- Peripheral vascular disease
- Reduced systolic blood pressure
- Killip class
- Initial serum creatinine concentration
- Elevated initial cardiac markers
- Cardiac arrest on admission
- ST segment deviation (elevation or depression)
What is Killip class and what are the 4 categories?
system sed to stratify risk post-myocardial infarction
- I: no clinical signs of heart failure (6% 30-day mortality)
- II: lung crackles, S3 (17%)
- III: frank pulmonary oedema (38%)
- IV: cardiogenic shock (81%)
What is the definition of ST-elevation?
ST-segment elevation and elevated biomarkers of myocardial damage
What are the criteria for NSTEMI?
ECG changes but no ST-segment elevation, + elevated biomarkers of myocardial damage
What are the 2 groups into which to categories patients with ACS for management?
- STEMI
- NSTEMI/unstable angina
When should IV morphine be given in ACS and what may be a disadvantage of it?
only if patient is in severe pain
previously given routinely but evidence suggests this may be associated with adverse outcomes
In which patients should nitrates be used to manage ACS with caution?
hypotensive patients (can worsen)
Following the MONA treatment what is the next step to determine what further treatment is indicated for ACS?
determine if patient meets ECG criteria for STEMI (interpret in context of clinical history)
What are the ECG/clinical criteria for a STEMI diagnosis?
- clinical symptoms consistent with ACS (>20 minutes duration) with persistent (>20min) ECG features in 2 or more contiguous leads of:
- 2.5 mm (≥ 2.5 small squares) ST elevation in leads V2-3 in men <40 years, or ≥ 2.0 mm (i.e ≥ 2 small squares) ST elevation in leads V2-3 in men over 40 years
- 1.5 mm ST elevation in V2-3 in women
- 1mm ST elevation in other leads
- new LBBB (LBBB should be considered new unless evidence otherwise)
What are 3 factors which determine whether ST elevation is considered significant?
- Gender: in V2-3, 2-2.5 needed in males, 1.5 in females
- Age: in V2-3, 2mm needed in male >40, 2.5mm needed in male <40
- Leads: 1mm only needed in leads other than V2-3
When should LBBB be considered new?
always consider new (and therefore evidence of STEMI) unless evidence otherwise
What is the easy way to remember ECG evidence of LBBB?
Look at V1 and V6: W in V1, M in V6 (WiLLiaM)
What are 5 ECG signs of LBBB?
- QRS duration> 120ms
- Dominant S wave in V1 (creating W)
- Broad monophasic R wave in lateral leads (I, aVL, V5-6)
- Absence of Q waves in lateral leads
- Prolonged R wave peak time > 60ms in leads V5-6

What is the key determinant of what the initial management of STEMI involves?
is PCI possible within 120 mins

If PCI is available within 120 mins, what is the management of STEMI? Includes 3 drugs given
- give prasugrel
- radial access preferred
- give unfractionated herparin + bailout glycoprotein IIb/IIIa inhibitor (e.g. abciximab)
- drug-eluting stents should be used in preference
What are 3 examples of glycoprotein IIb/IIIa inhibitors?
- abciximab
- Tirofibn
- Eptifibatide
What is the management of STEMI if PCI is not possible within 120 minutes? 3 aspects
- Fibrinolysis with alteplase/streptokinase
- Given antithrombin at the same time
- following procedure give ticagrelor (antiplatelet)
What are 2 examples of fibrinolytic drugs?
- Alteplase
- Tenecteplase
What are 3 assumptions made by the broad STEMI maangement plan?
- Patient presents within 12 hours of symptom onset
- Patient is not a high bleeding risk
- Patient is not on oral anticoagulants
How should STEMI management by modified for patients presenting after 12 hours of symptom onset?
consider PCI if ongoing myocardial ischaemia or cardiogenic shock
How should STEMI management by modified for patients with high bleeding risk?
consider swapping prasugrel for ticagrelor/swapping ticagrelor ofor clopidogrel
How should STEMI management by modified for patients taking oral anticoagulants?
swap prasugrel for clopidogrel
What are the 2 criteira which usually must be met for STEMI to be managed with PCI?
- presentation is within 12 hours of onset of symptoms
- PCI can be delivered within 120 minutes of time when fibrinolysis could have been given
When should you consider PCI to manage STEMI beyond 12 hours of symptom onset?
if there is still evidence of ongoing ischaemia
What type of stent is used for PCI and why?
drug-eluting stents are now used. Previously ‘bare-metal’ stents were sometimes used but have higher rates of restenosis
Which vessel is preferred as the route for delivery of PCI?
radial access
When is fibrinolysis used to treat STEMI?
offered within 12 hours of onset of symptoms if primary PCI cannot be delivered within 120 minutes of time when fibrinolysis could have been given
e.g. patient presenting to small DGH without facilities for PCI and they can’t be transferred to larger hospital with PCI within 120 minutes
What should be done if a patient’s ECG 90 minutes after fibrinolysis fails to show resolution of ST elevation?
they require transfer for PCI
What type of antiplatelet therapy is given to patients prior to PCI and what does this consist of?
- dual antiplatelet therapy - aspirin + another drug
- if not taking oral anticoagulent: aspirin + prasugrel
- if taking oral anticoagulent: aspirin + clopidogrel
When is clopidogrel given rather than prasugrel as dual antiplatelet therapy before PCI?
if patient is taking an oral anticoagulant
What is the drug therapy given during PCI and how does it change for radial vs. femoral access?
- radial access: unfractionated heparin + bailout glycoprotein IIb/IIIa inhibitor (GPI)
- femoral acess: bivalirudin + bailout GPI
What are 2 additional procedures during PCI to consider?
- Thrombus aspiration (not mechanical thrombus extraction)
- Complete revascularisation: for patients with multivessel coronary artery disease without cardiogenic shock
What drug must patients be given in addition to fibrinolytic drugs if undergoing fibrinolysis?
antithrombin drug
What drug should be given following fibrinolysis?
ticagrelor
What investigation should be performed following fibrinolysis and what should be done based on the result?
ECG 60-90 minutes afterwards; if persistent MI, PCI should be considered
What is bivalirudin?
reversible direct thrombin inhibitor used as an anticoagulant in management of ACS (during PCI via femoral access)
What is the mechanism of action of thienopyridine antiplatelets (clopidogrel, prasugrel, ticagrelor, ticlopidine)?
antagonist of the P2Y12 adenosine diphosphate (ADP) receptor, inhibiting the activation of platelets
What drug might clopidogrel interactive with and what is the effect?
PPIs may make it less effective (particularly omeprazole and esomeprazole)
What is the approach to management of NSTEMI/unstable angina (algorithm)?
- Give aspirin 300mg and fondaparinux if no immediate PCI planned
- esptimate 6-month mortality e.g. with GRACE
- if low risk: conservative management
- if intermediate/high risk: coronary angiography with follow on PCI if necessary
What 2 things do you give immediately in NSTEMI/unstable angina once identified?
aspirin 300mg
fondaparinux if no immediate PCI planned
What is the management of NSTEMI/unstable angina if 6-month mortality is low (from e.g. GRACE score)?
conservative management: give ticagrelor
What is the management of NSTEMI/unstable angina if the 6-month mortality (e.g. from GRACE) is intermediate or high? 3 aspects
- (coronary angiography ± follow on) PCI:
- offer immediately if clinically unstable, otherwise offer within 72 hours
- drug-eluting stents used in preference
- give prasugrel or ticagrelor
- give unfractionate heparin
When should PCI be offered in intermediate-high risk 6-month mortality NSTEMI/UA?
offer immediately if clinically unstable, otherwise within 72 hours
How does the management of NSTEMI/unstable angina hange if the patient is a high bleeding risk? 2 things
- consider swapping fondaparinux for an alternatiev antithrombin/dose
- swappng prasugrel for ticagrelor/ swapping ticagrelor for clopidogrel
How does the management of NSTEMI/unstable angina change if a patient is taking oral anticoagulants?
swap prasugrel/ticagrelor for clopidogrel
When should unfractionated heparin be given instead of fondaparinux for patients with NSTEMI/unstable angina? 2 situations
- If immediate angiography planned
- If patients’ creatinine is >265 micromol / L
In NSTEMI/unstable angina, what decision does the GRACE score help us to decide?
- helps decide whether patient has coronary angiography with follow-on PCI if necessary or conservative management
What determines whether patients with intermediate-high risk NSTEMI/UA are offered coronary angiography with follow on PCI if necessary immediately or within 72h?
patients who are clinically unstable (e.g. hypotensive) are offered immediate coronary angiography with follow-on PCI if necessary
the rest with GRACE score intermediate/high/highest offered coronary angiography with follow on PCI if necessary within 72 hours
In addition to patients with NSTEMI/UA scoring intermediate-high on the GRACE score, when else should coronary angiography be considered for NSTEMI/UA patients?
if ischaemia is subsequently experienced after admission
What are 2 drugs which are given additional to PCI in NSTEMI/UA?
- unfractionated heparin (regardless of whether patient has already had fondaparinux)
- prior to PCA: dual antiplatelet therapy: aspirin + prasugrel/ ticagrelor/ clopidogrel
What determines what dual antiplatelet therapy a patient with NSTEMI/UA should be given prior to PCI?
- if not taking an oral anticoagulant: prasugrel or ticagrelor
- if taking an oral anticoagulant: clopidogrel
What is the conservative management for patients with NSTEMI/UA?
dual antiplatelet therapy: aspirin + ticagrelor or clopidogrel
What determines the dual antiplatelet therapy for patients with NSTEMI/UA undergoing conservative management?
if no at high risk of bleeding: ticagrelor
if at high risk of bleeding: clopidogrel
What are the 4 drugs which are given as secondary prevention of MI following an MI?
- Dual antiplatelet therapy (aspirin + second antiplatelet agent)
- ACE inhibitor
- Beta-blocker
- Statin
How much exercise is recommended as secondary prevention of MI?
20-30 minutes a day until patients are slightly breathless
How long after uncomplicated MI can sexual activity resume?
4 weeks (reassure that sex doesn’t increase likelihood of further MI)
How long following an MI can PDE5 inhibitors (e.g. sildenafil) be used following MI?
6 months
When shouhld PDE5 inhibitors be avoided?
in patients prescribed either nitrates or nicorandil
After how long can the second antiplatelet as part of dual antiplatelet therapy for ACS management be stopped?
12 months (but this period can be altered if high risk of bleeding or high risk of further ischaemic events)
What treatment should be initiated for patients who have had an acute MI and have symptoms and/or signs of heart failure and left ventricular systolic dysfunction?
aldosterone antagonist licensed for post-MI treatment (e.g. eplerenone)
When should eplerenone be initiated post MI if indicated?
within 3-14 days of MI, preferably after ACE inhibitor therapy
What is the recommendation for management of hyperglycaemia during acute coronary syndromes?
dose-adjusted insulin infusion with regular monitoring of blood glucose levels to glucose below 11.0 mmol/L
(intensive insulin therapy (IV infusion of insulin and glucose with or without potassium) not recommeded routinely)


