8.1 Pupils Flashcards
What is an efferent pupil defect? Any key features?
Motor defect; lesion to system carrying signal from CNS to iris
Key feature: anisocoria
What is an afferent pupil defect? Key features?
Lesions in the initial signalling pathway (usually retina or optic nerve)
Key features: abnormal signalling reflexes, no anisocoria
Mydriasis mechanism? (including neurotransmitters and receptors)
Mydriasis = dilation
Excite sympathetic system, inhibit parasympathetic
Norepinephrine acts on α-adrenergic receptors and stromal elastic expansion
Miosis mechanism? (including neurotransmitters, receptors)
Miosis = constriction
Excite parasympathetic, inhibit sympathetic
Acetylcholine acts on muscarinic receptors
Equal pupil sizes in light and dark indicates ….
Normal light reflex, normal pupils
Unequal pupil size
In light: OD is 5mm, OS is 6mm
In dark: OD is 7mm, OS is 8mm
Normal light reflex, physiological anisocoria
Disparity is the same in light and dark conditions and is less than 2mm (could still be physiological anisocoria if >2mm but very uncommon)
Light on right eye: OD 5mm, OS 5mm
Light on left eye: OD: 3mm, OS 3mm
No light perception in right eye
Absolute afferent pupil defect (OD affected in this case)
Swinging flashlight test
Light on right eye: OD: 3mm, OS 3mm
Light on left eye: OD: 4mm, OS 4mm
Relative afferent pupil defect (OS affected in this case)
Abnormal light reflex, no light perception
absolute APD
Abnormal light reflex, light perception is fine
Relative APD
Abnormal light reflex, bilateral, near reflex normal
Argyll Robertson pupil (efferent defect)
Abnormal light reflex, bilateral, near reflex abnormal
Drug induced pupil issue likely, efferent
Abnormal light reflex, anisocoria, no ptosis, near defect
Adie’s tonic pupil (efferent)
Abnormal light reflex, anisocoria, no ptosis, intermittent near defect
Tourney phenomenon (efferent)
abnormal light reflex, anisocoria, no ptosis, no near defect, no trauma or drugs
Hutchinson’s pupil (efferent)
abnormal light reflex, anisocoria, no ptosis, no near defect, trauma
Iris sphincter damage (efferent)
abnormal light reflex, anisocoria, no ptosis, no near defect, drugs
Pharmacological pupil (efferent)
abnormal light reflex, anisocoria, ptosis, + (XOT - down and out eye position)
3rd nerve palsy (efferent defect)
abnormal light reflex, anisocoria, ptosis, anhydrosis
horner syndrome (efferent defect)
Pupils are equal in size in _____ pupillary defects
afferent
Ocular associations of afferent pupil defects
reduced VA, colour vision defects, central visual field defects, abnormal VEP (visual evoked potential)
Minor causes of afferent pupil defect ?
Very mild: amblyopia, vitreous hemorrhage
Mild: macular degeneration, BRVO/BRAO, retinal detachment, other retinal disease
(BRVO/BRAO = branch retinal vein/artery occlusion)
Major causes of afferent pupil defects
(think nerves and blood)
- Optic nerve disease: ischemic optic neuropathy (ION), optic neuritis, optic atrophy, tumour, glaucoma)
- Ischemic CRVO/CRAO (central retinal vein/artery occlusion)
- RAPD: optic chiasm and tract lesions (infarcts, demyelination)
Absolute afferent pupil defect (type of lesion, alternative name)
Complete optic nerve lesion
aka amaurotic pupil
Absolute afferent pupil defect (signs)
Pupils equal in size
Involved eye is blind (no light perception)
Normal eye stimulated with light = normal light response in both eyes (constriction). Affected eye stimulated = no response/change
Normal near reflex
relative afferent pupil defect (what it is)
RAPD = objective sign of asymmetric lesion in anterior visual pathway
relative afferent pupil defect (cause)
incomplete optic nerve lesion or severe retinal disease (usu. optic nerve conduction defect)
NEVER due to a dense cataract
relative afferent pupil defect (signs)
Like an absolute afferent pupil defect but not as severe
Swinging flashlight test: both eyes constrict when light shone in normal eye. both eyes dilate when light shone in affected eye. Affected eye’s consensual response > direct response so affected eye responds as if the light is dimmer; termed pupillary escape
What is the near reflex?
Pupils constrict with convergence, dilate with divergence
What is the light-near dissociation?
normal near reflex but abnormal or sluggish light reflexes
If _____ reflex is normal, the ____ reflex will be normal (but the converse is not true)
light, near
Argyll Robertson pupil (causes, association)
neurosyphilis (tertiary syphilis)
Ocular assocations: interstitial keratitis
Systemic associations: (+) syphilis serology
Argyll Robertson pupil (signs)
Small irregular pupils that show light-near dissociation
Usually bilateral but may be asymmetrical
Poor reaction to light (constriction and dilation
Poor dilation with mydriatic
Normal constriction with convergence
pharmacological pupil defects (reflex responses, type)
abnormal light response
abnormal near response
(efferent defect)
pharmacological pupil can be ______ or _______
unilateral or bilateral
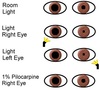
right pharmacological pupil
pharmacological pupil, unilateral, miosis -> what drug will cause this?
pilocarpine
What drug(s) will cause pharmacological pupil, unilateral, mydriasis?
Mydriacyl, tropicamide, cyclogyl, cyclopentalate
What drugs will cause bilateral pharmacological pupils, miosis?
Systemic drugs (8): caffeine, chloryl hydrate, chlorpromazine, histamine, MAO inhibitors, morphine, nicotine, opiates
What causes bilateral pharmacological pupil, mydriasis?
Systemic drugs: amphetamines, antihistamines, cocaine, benedryl, LSD, marijuana, tricyclic antidepressants
What is anisocoria?
Unequal pupil size; abnormal pupil may be smaller or larger
Anisocoria suggests …
Efferent (motor) defect but need to look at eyelid position and EOM

