7.1 Anterior Uvea Flashcards
What are epicapsular stars? (Definition and appearance)
Remnants of embryonic pupil membrane.
Appear as brown pigment flecks on anterior lens surface
Clinical significance of epicapsular stars?
No clinical significance.
Very common, don’t affect vision.
BUT do not confuse with pigment dispersion syndrome
What are persistent pupil membranes? (Definition and appearance)
Remnants of embryonic pupil membrane.
Appear as fine avascular threads that emanate from collarette (may also attach to pupil margin or lens)
Clinical significance of persistent pupil membrane?
No clinical signifance unless has an effect on vision (based on size of defect). Very common
Iris coloboma (definition, appearance)
Incomplete closure of optic cup.
Can affect iris, choroid/retina, eyelids.
ALWAYS inferior nasal
Iris coloboma (condition type, Tx)
Rare, congenital, *non-progressive* condition.
Can affect vision if retina/optic nerve involved.
Tx: cosmetic contact lens (cosmetic and can reduce glare)
Chediak-Higashi, Hermansky-Pudiak
Systemic rare AR diseases associated with albinism.
Ocular albinism (features)
Little/no pigment in iris or fundus.
Characteristic iris transillumination
Low vision: foveal hypoplasia, nystagmus, abnormal nerve crossings at chiasm
Anaridia (definition, frequency, features)
Congenital bilateral absence of iris, genetic mutation.
Very rare
Retinal (macular) hypoplasia (VA ~6/60)
Nystagmus
Cataract
Progressive corneal opacity
Anaridia (associations, potential complications)
Wilm’s tumour (kidney)
High glaucoma risk
Heterochromia iridum vs heterochromia iridis
Different iris colours between the 2 eyes vs different iris colours on the SAME eye
Heterochromia iridum (associations)
Possible associations: Horner’s syndrome, iris inflammation (Fuch iridocyclitis)
A heterochromia iridis Dx requires you rule out _____
A pigmented iris tumour
Pigment dispersion syndrome (definition, associations)
Bilateral, pigment shedding from iris pigment epithelium (into anterior segment/chamber)
Associated w pigmentary glaucoma
Pigment dispersion syndrome (pathogenesis)
- “reverse pupil block” leads to IOP increase (aqueous not flowing easily thru pupil and force iris to bow backwards against zonules)
- Posterior pigment layer rubs against lens zonules (2ndary to posterior iris bowing mid periphery)
Pigment dispersion syndrome (signs)
CAIGL
Cornea: endothelium pigment deposition, Krukenberg spindle
AC: deep, floating melanin granules
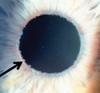
Iris: transillumination!, pigment dusting, pupillary ruff loss, pigment epithelial atrophy
Gonioscopy: mid-peripheral iris concavity, wide open angle, trabecular hyperpigmentation
Lens: occasional Scheie line (line/annular ring of pigment)
Pigment dispersion syndrome (management)
Monitor IOP
Pseudoexfoliation syndrome (definition/etiology)
abnormal basement membrane of epithelial cells produce fibrillary extracellular materials that is deposited throughout anterior segment
- Involved epithelial cells from trab. meshwork, equatorial lens capsule, iris, CB
- Deposition sites: anterior lens capsule, zonules, CB, iris, trabeculum, anterior vitreous, conjunctiva
Pseudoexfoliation syndrome (associations)
Relatively common cause of open-angle glaucoma (syndrome more common in women but the glaucoma risk greater for men)
Pseudoexfoliation syndrome (signs)
CAIGL
Cornea (endothelium): cellular debris, pigment deposits, diffuse Krukenerg spindle
AC: mild aqueous flare (maybe)
Iris: pupil margin cellular debris, sphincter atrophy (moth eaten transillumination defect)
Gonioscopy: trab hyperpigmentation, cellular debris is trabeculum, Sampaolesi line (pigment on/anterior to Schwalbe line)
Lens: central disk debris, peripheral band debris (clear mid-periphery)
Diseases with transillumination defects
Mid-periphery - pigment dispersion syndrome
Moth-eaten/sphincter atrophy - pseudoexfoliation
Entire iris lights up - ocular albinism
You should dilate a suspected pseudoexfoliation syndrome patient because…
It allows you to see if there is debris on the lens with a central disk and peripheral band (created by pupil movements)
Iridocorneal endotheliopathy variations
“ICE” syndrome
- Essential iris atrophy
- Iris nevus (Cogan-Reese) syndrome
- Chandler syndrome
Iridocorneal endotheliopathy (what it is/associations)
Abnormal corneal endothelial layer which has the capacity to migrate across the angle onto the surface of the iris
Corneal decompensation (bc compromised endothelium)
Glaucoma (synechial angle closure) -> 50% of Px develop it -corneal endothelial cells migrate to iris which blocks aqueous outflow and creates synechiae/adhesions b/w cornea and iris