22- Transfusion Medicine Flashcards
REVIEW!
What are the 4 Blood groups?
What RBCs can each recieve and what plasma?
Group O- Group O blood and Group O, A, B, AB plasma
Group A- Group A, O blood, and Group A, AB plasma
Group B- Group B, O blood, Group B, AB plasma
Group AB- Group A, B, AB, O blood, and group AB plasma

When do we prophylactically give platelelet transfusions?
Marrow failure
before surgery
What are the guidelines for giving platelets to marrow failure patients?
<10K transfusion indicated
<20K may be indicated (ie sepsis, mucosisitis, bleeding history)
What are the guidelines for giving platelets before surgery?
<50K General surgery, IR procedures
<100K CNS, Eye, high-risk surgery
Any platelet count: platelet inhibitor drugs; platelet dysfunction
When do we therapeutically give platelets transfusions?
active bleeding AND
- platelet count <50K
- platelet function defect- platelet inhibitor meds, congenital platelet disorder
Which patients SHOULD get RBC transfusion?
-
Symptomatic/perioperative anemia
- single unit transfusions with H&H/symptom rechecks
- decisions should be guided by combination of symptoms, vital signs, and lab values
-
Patients who are actively bleeding
- Hgb trigger to begin transfusion is based on rapidity of bleeding and ability to “stop the bleed”
What is the safest bet for RBC transfusion Hgb cut off
RESTRICTIVE transfusionstrategy (Hgb 7-8 g/dL) is safe
the literature supports this
When is it reccomended that you use restrictive RBC strategy?
- Restrictive
- Hgb<7 for stable pts in hospital
- Hgb<8 for pts undergoing ortho, cardiac surgery or pre-existing CVD
In what pts is there no reccomendation for transfusion threshold?
ACS/MI, heme/onc w bleeding risk, chronic transfusion dependent anemia
**I guess this mean for these pts just use your best judgement
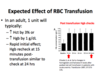
What is the expected effect of 1 unit of RBC transfusion?
increase Hct by 3%
increase Hgb by 1 g/dL
rapid initial effect; Hbg recheck at 15 minutes post-transfusion should be similar to check 24 hrs (otherwise there may be a destructive process)
What are the universal steps if you suspect a transfusion reaction?
STOP THE TRANSFUSION
Keep the IV patent (new tubing and .9NS)
Obtain vital signs, assess patient
provide supportive care
What will the nurse do if a transfusion reaction is suspected?
verify all patient and product information
notify provider and transfusion services
follow provider orders (meds, labs, etc)
send blood bag and any paperwork to lab
document reaction in patient’s medical record
What 4 conditions could be assciated w fever during a transfusion?
FNHTR
Hemolysis
Septic Reaction
Patient’s Underlying Disease
What condition is associated with rash/itching during transfusion?
Allergic reaction
What transfusion reactions are associated with dyspnea?
TRALI (most deadly)
TACO
Anaphylaxis

What causes Acute Hemolytic Transfusion Reaction?
Accelerted clearance of transfused red cells due to red cell incompatibility between donor and recipient
Anti-A or Anti-B, Anti-Kell, Anti-Jk(a), Anti-Fy(a)
What are the signs ans symptoms of Acute Hemolytic Transfusion Reaction?
Fever, chills, nausea and impending doom
hypotension
back pain, chest pain, or pain at infusion site
hemoglobinemia, hemoglobinuria
coagulopathy
renal failure

How do you treat Acute Hemolytic Reaction?
- Stop transfusion
- IV fluids to maintain blood pressure and urine output
- supportive care
- monitor vitals
- monitor labs Hgb, renal function
- administer platelets, FFP, and/or cryoprecipitate as needed for DIC
What is the most common transfusion reaction that presents with a fever?
Febrile Non-Hemolytic Transfusion Reaction (1-3%)- honestly what a relief
What does the frequency of Febrile non-hemolytic transfusion reaction vary with?
type of blood product and WBC content
age of blood product
recipient characteristics
What signs and symptoms are associated with Febrile Non-hemolytic Transfusion Reaction and when do they occur?
during or up to 4 hrs post transfusion
Fever (at least 1C or 2 F elevation so >38C/100.4F)
usually associated with chills and/or rigors
no other cause is identifiable
What is the etiology of FNHTR
interaction of leukocyte antibody (in recipient) with leukocytes/fragments in product
passive transfer of biologic response modifiers that accumulate in product during storage
activates cytokines (I-1B, IL-6, TNFa)
triggers fever and chills
How do you manage suspected FNHTR?
antipyretic initially
if significant rigors 25-50mg Demerol IV
often see resolution of fever and chills within 30 minutes of dicontinuation of unit
Leukoreduction (LR) has reduced the incidence of FNHTR (reduced 50% in Red cells and 80% in platelets)


