17 - HTN, CKD, Hyperlipidaemia Flashcards
(46 cards)
What is the definition of CKD and what is the diagnostic criteria?
Reduction in kidney function or structural damage (or both) present for more than 3 months, with associated health implications
Markers of kidney damage: proteinuria (urinary albumin:creatinine ratio [ACR] greater than 3 mg/mmol), urine sediment abnormalities, electrolyte imbalance, abnormalities detected by histology, structural abnormalities detected by imaging, and a history of kidney transplantation, and/or
Persistent reduction in renal function with eGFR <60ml/min

What are the different classifications of CKD?
Classified based on the underlying cause, GFR, and proteinuria category
Given a G score and an A score

What are some risk factors for developing CKD?
- Hypertension
- Diabetes
- CVD
- AKI
- Nephrotoxic drugs e.g ACEi, bisphosphonates, calcineurin inhibitors, NSAIDs, diuretics, Lithium
- Obstructive uropathy
- Smoking
- Afro-caribbean/Asian
- Family history e.g auto dominant polycystic kidney disease
- Aged over 60
- Kidney transplant
- Obesity
- SLE, Vasculitis, Myeloma

What are some complications of CKD?

- AKI
- Hypertension
- CVD
- Renal anaemia
- Renal mineral and bone disorder
- End-stage renal disease (ESRD)
- Increased all-cause mortality
- Electrolyte imbalances
- Malnutrition
- Infertility, libido loss, impotence, amenorrhea

What are some of the signs and symptoms of CKD that may present to a GP?
Symptoms
- Often asymptomatic or generic/vague
- Lethargy, itch, breathlessness, cramps (often worse at night), sleep disturbance, bone pain, loss of appetite, vomiting, weight loss, taste disturbance (often present with end-stage disease).
- Polyuria (tubular concentrating ability is impaired), oliguria, nocturia, anuria
Signs
- Uraemic breath odour, pallor due to renal anaemia, cachexia, cognitive impairment, dehydration or hypovolaemia (risk of AKI)
- Tachypnoea (may be due to fluid overload, anaemia, or co-morbid ischaemic heart disease), hypertension (may be primary or secondary to CKD itself)
- Palpable bilateral flank masses with possible hepatomegaly (suggests polycystic kidney disease with possible liver cysts).
- Palpable distended bladder (suggests obstructive uropathy).
- Peripheral oedema (may be due to renal sodium retention, hypoalbuminaemia, or co-morbid heart failure).
- Peripheral neuropathy (may present with paraesthesia, sleep disturbance, and restless legs syndrome)
- Frothy urine (proteinuria)

What are some investigations you may do if you suspect a patient has CKD?

- Blood tests for serum creatinine and eGFR and advise not to eat meat for 12 hours before: if less than 60 repeat in 2 weeks and again in 3 months if still less than 60 and no evidence of sudden deterioration
- Early morning urine sample for ACR: if less than 3mg/mmol no action, if above then indicates proteinuria so repeat in 3 months. Can be falsely raised during menstruation, UTI, strenuous exercise and upright posture
- Urine dipstick for haematuria: if 1+ arrange MSU to check for UTI. If isolated persistent haematuria (2 out of 3 dipsticks positive) and no decline in eGFR or proteinuria think about urological cancer
- Check BMI, HbA1c, Lipid profile, BP to assess for CVD risk factors.
- Consider renal US if suspect stones, obstruction, FHx of polycystic kidney disease
- If repeated in 3 months and still the same ACR and eGFR can classify what type of CKD it is to determine the risk of disease progression. (raised serum creatinine by 20% but normal eGFR can indicate CKD)

How should CKD be monitored in primary care to look for disease progression?
- Monitor renal function by looking at eGFR and urine ACR. If decline by 25% and a category or drop by 15ml/min in 12 months this is accelerated progression
- FBC to exclude renal anaemia
- Serum calcium, phosphate, vitamin D, and parathyroid hormone tests to exclude renal metabolic and bone disorder
Which CKD patients should be referred to a nephrology specialist?
- Uncontrolled HTN when has not responded to 4 different drugs
- Complications include renal anaemia as may need EPO, decline in nutrition status, phosphate or other mineral disorders, persistent metabolic acidosis
- Suspect renal artery stenosis if decline in eGFR by 25% within 3 months of starting RAAS antagonist, refractory HTN, pulmonary oedema, renal artery bruit

What lifestyle advice can be given to a patient with CKD?
- Provide sources of info and support e.g patient info, NHS, Kidney Care UK, Think Kidneys
- Healthy lifestyle and diet as CKD can raise lipids and cholesterol e.g alcohol, low protein diet if advised by specialist, smoking, exercise
- Tell patient to avoid NSAIDs, protein supplements and herbal remedies
- Advise on risk of AKI

How are patients with CKD managed in primary care apart from the monitoring for disease progression?

- Assess for and manage risk factors and co-morbidities of CKD and CVS e.g nephrotoxic drugs, disease progression
- Assess for hypertension and give low cost RAAS antagonist if HTN as antiproteinuric(lisinopril or lorsartan). If ACR less than 70mg/mmol aim for 140/90, if more than or diabetic aim for 130/80
- Prescribe statin but be aware raised risks of myopathy and rhabdomyolysis with lower kidney function. Do not prescribe if eGFR<30
- Ensure offered flu and pneumovax

What is the pathophysiology behind CKD?
- Renal damage (e.g by diabetes or HTN)
- Reduced filtration (oxi stress, glomerulosclerosis, loss of nephrons)
- Increased glomerular pressure so glomerular hypertrophy
- Increased glomerular permeability (inflammartion, fibrosis, scarring)
- Overall loss of kidney function

What are the sick day rules for CKD?
When patient has acute illness (N+V for 12 hours or fever, shaking, shaking) stop any ACEi, ARBs, NSAIDs, diuretics, metformin
This is done to prevent an AKI or any drugs building up in the system due to impaired renal function. Need to inform patient of this risk of AKI on Dx
Mneumonic is DAMN

How do you treat a patient with CKD plus the following:
- metabolic acidosis (due to build up of urea)
- anaemia
- secondary hyperparathyroidism
- Oral sodium bicarbonate
- Iron and EPO injections
- Kidney needed for Vit D synthesis, without PTH increases. Phosphate binding agent, active Vitamin D
How often do CKD patients need monitoring of their FBC, eGFR, ACR, phosphate, PTH, calcium, serum creatinine?
- Every 6-12 months
- If stage 4 every 3-6 months and PTH every 6-12 months
- If stage 5 FBC for anaemia monthly, every 1-3 months check calcium and phosphorous etc, every 3-6 months check PTH
Check lipids anually in all CKD patients
What are the target values for blood pressure?
- Stage 1 >140/90 or >135/85 HBPM
- Stage 2 >160/100 or >150/95 HBPM
- Stage 3 >180/120

What is the definition of hypertension?
Persistently raised arterial blood pressure
Stage 1: >140/90
Stage 2: >160/100
Stage 3: >180/120
Malignant hypertension when over 180/120 with retinal haemorraghe and/or papilloedema

How do you manage blood pressure that is over target in general terms?
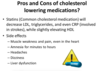
MEMORISE IMAGE
- Lifestyle advice includes stopping smoking, cutting down caffeine, cutting down alcohol, low dietary salt intake, healthy diet, regular exercise
- Consider drug treatment in under 60s if Stage 1 HTN and QRISK>10%, in all over 80s with Stage 1 HTN, and referral for all those under 40 with Stage 1 HTN
- Treat all patients with stage 2 regardless of age
- Treat severe hypertension promptly

What antihypertensive drug do you use when patients are over target?
- ACD rule!!!
- Add spironolactone, beta blockers and alpha blockers if necessary
- Give drugs if stage 1 with Q risk >10% or stage 2

What are some of the risk factors for developing hypertension?
- Increasing age
- Male
- Ethnicity (AfroCaribbean)
- Family history
- Social deprivation
- Smoking
- Alcohol
- Obesity
- Lack of physical exercise
- Emotional stress

What are the complications of hypertension?
Single biggest risk factor for CVD (strokes and heart attacks)

What are the causes of hypertension?
- Primary: no identifiable cause
- Secondary: other causes e.g renal artery stenosis, phaeochromocytoma, use of certain drugs, diabetic nephropathy, polycystic kidney disease, renal cell carcinoma, coarctation of the aorta, Cushing’s, acromegaly, hypothyroidism, primary hyperaldosteronism

When do you need to refer someone presenting with hypertension for a same day referral?
- Clinical blood pressure over 180/20 with signs of retinal haemorraghe or papilloedema
- Suspected phaeochromocytoma e.g labile/postural hypertension, headache, palpitations, pallor, abdominal pain, diaphoresis

How is hypertension officially diagnosed?
- Measure BP in both arms with appropriate cuff size. If difference between the two is >15mmHg repeat the measurements.
- If over 140/90 repeat. If still above offer ABPM/HBPM
- Check pulse before taking readings as if irregular will not be accurate so need manual reading

What investigations are done if somebody has a new diagnosis of hypertension?
Assess for target organ damage and cardiovascular risk
- Test for haematuria
- Measure ACR, HbA1c, eGFR, electrolytes, creatinine
- Examine the fundi
- Arrange ECG to look for left ventricular hypertrophy
- Measure serum cholesterol and HDL
- Look at QRISK score