17 - Hemolytic anemias intro Flashcards
(19 cards)
What are the 3 classifications of anemia?
- blood loss
- accelerated destruction
- decreased production
What are 3 classes of inherited hemolytic anemias?
Also called intrinsic:
- RBC membrane disorders
- RBC enzyme deficiencies
- Hemoglobinopathies
What are 5 classes of acquired hemolytic anemias?
Also called extrinsic:
- autoimmune (Ab mediated) hemolysis
- mechanical trauma
- infections
- chemical/toxic injury
- splenic sequestration
What are the 2 types of pathology behind hemolysis?
- Extravascular
- most common
- spleen >> liver, bone marrow
- macrophage mediated (usually Ab mediated)
- Intravascular
- less common
- within the vessels
- usually complement mediated or from mechanical destruction
- combination of the 2 also possible
What are some extravascular disorders?
- RBC membrane disorders
- RBC enzyme disorders
- sickle cell anemia
- thalassemias
- autoimmune hemolysis (antibody or complement)
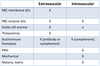
What are some intravascular disorders?
- RBC enzyme disorders
- sickle cell anemia
- autoimmune hemolysis (complement)
- PNH
- mechanical
- malaria, toxins

What are some consequences of hemolytic anemias?
- red cell destruction (shortened RBC lifespan)
- anemia
- elevated EPO
- compensatory increase in erythropoiesis
- reticulocytosis
- bone marrow hyperplasia
- hemoglobin degradation products secondary to hemolysis
- hemosiderosis (accumulation of iron in the spleen, liver, and bone marrow)
- hyperbilirubinemia, pigmented gallstones
What are 4 blood tests you should get to evaluate hemolysis?
- CBC
- normocytic (to macrocytic) anemia
- reticulocytosis
- peripheral blood smear
- biochemistry tests (look for LDH, AST, potassium, hyperbilirubinemia, hemoglobinemia)
- DAT (direct antiglobulin test)

What cellular contents can be detected in the blood and indicate hemolysis?
LDH (lactate dehydrogenase), AST (aspartate aminotransferase), potassium
What is hemoglobinemia?
Free Hb in plasma
**more pronounced in intravascular hemolysis (detected by decreased haptoglobin in plasma)
What are these images showing?

- bite cells
- shistocytes
- sickle cells
- spherocytes

What are 3 urine tests you should get to evaluate hemolysis?
- hemoglobinuria
- usually from intravascular processes
- blood by dipstick but absence of RBCs when you run a urinalysis
- increased urobilinogen (dipstick)
- breakdown product of biliverdin, formed in the gut
- hemosiderinuria
- usually from intravascular processes
- iron storage deposits in renal epithelium

Describe erythroid precursors
You know they’re erythroid when they have perfectly round nuclei!
**she mentioned it would be good to know this for the exam!!

What are 2 common symptoms of all patients with hemolytic anemia despite differing underlying etiology?
Anemia and hyperbilirubinemia (other characteristic symptoms are needed to determine underlying pathology)
What is a normal hemoglobin level? What could affect how a patient reacts to decreased levels of Hb?
- normal= 12-16 g/dL
- young patients with chronic hemolytic conditions (e.g. sickle cell) can often tolerate extreme anemia with minimal symptoms because they are used to a lower baseline
What are some symptoms of decreased Hb?

What are some symptoms of hyperbilirubinemia?

What are 2 rare complications of hemolytic anemia?
- pigment induced kidney injury
- heme pigment can cause tubular obstruction, direct cellular injury, and vasoconstriction
- results in decreased medullary blood flow
- urinalysis shows hemoglobinuria without RBCs
- folate deficiency due to increased utilization (giving folate won’t correct this because it keeps being used up… need to address the underlying hemolysis)
What are 4 clinical features of hemolytic anemia that point towards a specific underlying disease process?
- splenomegaly/hepatomegaly
- related to extra-medullary hematopoiesis
- seen in thalassemias, PK deficiency, hereditary spherocytosis
- skeletal changes (convex bones; abnormal facies)
- related to expansion of marrow esp. in beta thalassemia major
- asplenia
- e.g. in sickle cell anemia
- microangiopathic hemolytic anemia
- TTP, HUS, DIC, malignant HTN, HELLP syndrome (idk what she means by this list but it’s the last slide of the lecture if you want to look it up…)


