17 - Benign and Malignant Skin Tumours Flashcards
How can skin cancers for classified?
- Melanotic (malignant melanoma)
- Non-melanotic (BCC and SCC)
What is an Actinic Keratosis and what does it look like?
Premalignant scaly spot found on sundamaged skin e.g face, hands, back, arms
Can regress or can progress to SSC
Often looks crumbly with yellow-white crust (keratotic) if solitary or erythematous if multiple

What are some differential diagnoses for Acitinic Keratoses?
- BCC
- Bowen’s
- Psoriasis
- Seborrhoeic keratosis
IF IN DOUBT BIOPSY!
What is the epidemiology of Actinic Keratoses?
- Fair skin with history of sunburn
- History of long hours spent outdoors for work or recreation (e.g lived abroad)
- Immunocompromised

What is the simple way to tell the difference between an acitinic keratoses and seborrheic keratoses?
AK usually are flat or slightly raised that cannot be moved but SK can move and look like they are stuck on like a sticker
Also SK can be tan coloured

AK is a precursor for SSC. What advice can you give to patients if they have AKs to prevent the progression?

- Avoid sun/wear sunscreen
- Wear hats and clothes that cover the skin
- Advise patient to monitor skin and educate them that it can predispose to skin cancer.

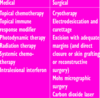
How are actinic keratoses treated?
Solitary/Keratotic/Thick Crust Lesions:
- Cryotherapy
- Shaving/Curettage
- Surgical excision, pathology and stitches
Field/Flat Red Lesions:
- 5-Fluorouracil cream
- Imiquimod cream is an immune response modifier
- Diclofenac cream
- Photodynamic therapy

How does photodynamic therapy work?
Light sensitive medicine is applied then light is applied to the area and this produces free radicals and causes cell death

What is Bowen’s Disease and what does it look like?
SCC in-situ
Pink scaly plaques
Flat edges NOT rolled like BCC

What are some risk factors for developing Bowen’s disease?
- Sun exposure
- Immunosuppressants
- Immunosuppression e.g lymphoma
- Radiation
- Arsenic
- HPV

How is Bowen’s disease diagnosed?
- Dermascopy: will show red irregular scaly plaque with crops of rounded and coiled blood vessels
- Biopsy: will show full thickness dysplasia

How is Bowen’s disease treated?
It can turn to SCC but unlikely. If it does go to SCC then likely to metastasise
- Observe
- Cryotherapy with liquid nitrogen
- Curretage
- 5Fluorouracil
- Imiquimod (off-licence)
- Photodynamic therapy

HOW CAN YOU TELL THE DIFFERENCE BETWEEN AK, BOWEN’S AND SCC?
will come back to
What is the prevalence of different skin cancers?
Most common to least:
- BCC
- SCC
- MM
How does an SCC (cancer of keratinocytes) present?
- Firm irregularly defined nodule that may persistently ulcerate and crust
- Usually on sun-exposed areas
- Often grow quickly and tender to touch
- Invasive and has the potential to metastasise

What are the risk factors for developing an SCC?
- Excessive UV exposure e.g occupation, lived abroad
- Pre-malignant skin e.g AK
- Chronic inflammation e.g leg ulcer, cutaneous lupus, HPV
- Immunosuppresion
- FHx
- Skin type 1
- Xeroderma pigmentosa

Which types of SCC are more likely to metastasise?

- Lip
- Ear
- Non sun-exposed site
- >2cm diameter or >2mm thick
- Host immunosuppression
How is SCC investigated and diagnosed?
- Dermascopy
- Biopsy or excision then biopsy
- Consider lymph node biopsy and MRI if think it has metastasised

How is SCC treated?
- Complete surgical excision with margins of normal tissue around the outside. May need flap to close
- Moh’s micrographic surgery for ill-defined, large, or recurrent tumours
- Radiotherapy if large and non resectable tumour
What is the pathophysiology of SCC?
- UV light causes mutation in p53 tumour suppressor gene
- Ageing, smoking, immunosuppressants (e.g Azathioprine), HPV also induce mutations in tumour suppressor genes
- Allows keratinocytes to mutate and reproduce without being killed

What is the prognosis of BCC? (Rodent Ulcer)
- Most common skin cancer
- Very slow growing
- Rarely metastasises
- Often recurrent
- Increased risk of developing other skin cancers

What are some risk factors for BCC?
- UV exposure
- History of severe/frequent sunburn in childhood
- Skin type 1
- Increasing age
- Male
- Immunosuppressed
- Previous history of skin cancer
- FHx (Genetic Predisposition)

What is the pathophysiology of BCC?
- Mutations in the PCTH tumour suppressor gene, can be triggered by UV radiation
- Can also inherit gene defects e.g P53, RAS
What are the different presentations of BCC?
Nodular (most common)

- Small skin coloured or pink nodule with surface telangiectasia and pearly rolled edge.
- May have necrotic or ulcerated centre (rodent ulcer)
- TURP
Superficial
- Scaly irregular plaque with microerosions on younger patients
- Morphoeic
- Basosquamous



















