11 - Ophthalmology Conditions 1 Flashcards
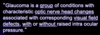
What is the worldwide leading cause of irreversible blindness?
Glaucoma
Collection of disorders resulting in progressive optic neuropathy. Can have raised IOP but doesn’t need to be raised for a diagnosis
What is the pathophysiology of acute angle closure glaucoma?
EMERGENCY!
Angle of the anterior chamber narrows acutely so rise in IOP >30mmHg, this leads to optic nerve damage.
This is due to the iris bulging forward blocking off the trabecular meshwork so aqueous humour cannot drain. Increased pressure on iris then blocks it off further
Primary angle closure: Anatomical predisposition
Secondary angle closure: Due to pathological processes e.g traumatic haemorraghe pushing the posterior chamber forwards

What are some of the risk factors of acute angle closure glaucoma?

- Increasing age
- Female
- Chinese
- FHx
- Shallow anterior chamber (Hyperopia/Short sighted)
- Medications: TCA, anticholinergics (as parasympathetics constrict pupil). Adrenergics

How will somebody with acute angle closure glaucoma present and what will you find on examination?
Presentation (Systemically unwell)
- Severely painful red eye
- Blurred vision
- Halos around lights
- Headache, Nausea, Vomiting (often mistaken for gastroenteritis until you look in their eye)
Examination
- Red eye
- Fixed dilated pupil
- Corneal haze
- Teary
- Decreased visual acuity
- Firm eye on palpation

What investigations are done if you suspect acute angle closure glaucoma?
- Tonometry
- Gonioscopy: look at anterior chamber and drainage system
- Slit lamp/Opthalmoscopy: optic disc cupping
- OCT?

How do you manage acute angle closure glaucoma?
Initial (Triad)
- Lie on back, avoid dark room as will dilate pupil and make worse
- Timolol (B-blocker to reduce aqueous humour production)
- Pilocarpine drops (muscarinic that causes miosis so pupil constriction opening angle up)
- Acetazolamide 500mg IV (carbonic anhydrase inhibitor that reduced aqueous humour production)
- Analgesia and Antiemetic
Definitive
- Bilateral Peripheral Laser Iridotomy once IOP lowered. Remove piece of iris so always drainage between anterior and posterior chamber. Often do other eye too as at risk of angle closure

Apart from the triad of pilocarpine (4% for darker eyes, 2% for lighter), azetazolamid and timolol for acute angle closure glaucoma, what are some other medications that can be used?
- Hyperosmotic agents: e.g glycerol or mannitol increase the osmotic gradient between blood and fluid in eye
- Brimonidine: sympathomimetic that reduces the production of aqueous fluid and increase uveoscleral outflow
What is the prognosis with acute angle closure glaucoma?
- If not treated can lead to visual loss
- Can occur to contralateral eye so make sure definitive treatment is done on both eyes
- CRAO

There is no formal screening test for glaucoma, however what patients are recommended to have regular reviews by optometrists?
Elderly: over 60 every 2 years, over 70 every year, free on NHS
FHx of Glaucoma: over 40 with first degree relative that has/had glaucoma then every year have eye test, free on NHS
Black African: over 40 should have test ever year, not free on NHS
Important to screen as asymptomatic until visual fields are affected and by this point it is too far!!!

What tests are performed to screen for and diagnose open angle glaucoma?

- Tonometry (Non-Contact or Goldmann Application is gold standard): increased pressure
- Fundoscopy: optic disc cupping (>0.5)
- Visual fields
- Can also measure corneal thickness and do gonioscopy to look at drainage of humour

What is the pathophysiology of open-angle glaucoma?
Increased resistance in trabecular meshwork so more difficult for aqueous humour to flow through so builds up in the eye and increases the pressure slowly over time

Why is there cupping in chronic glaucoma?

Normal optic cup is <0.5 the size of the optic disc.
When there is an increased pressure in the eye this puts pressure on the cup making it wider and deeper so >0.5 the size of the optic disc
Loss of disc makes the cup look larger

What are some risk factors of chronic open angle glaucoma?
- Increasing age
- FHx
- Myopia (short sighted)
- Black ethnicity
- ?Diabetes
- ?HTN

How does chronic simple (open-angle) glaucoma present?

- Asymptomatic at start and only picked up on screening
- Tunnel vision as gradual loss of peripheral vision
- Fluctuating pain
- Headaches
- Blurred vision
- Halos around lights especially at night

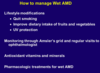
How are patients with open angle glaucoma managed?

Treatment starts when IOP is 24 or more. Aim is to reduce IOP to slow progression but cannot reverse
1st Line:
- Topical prostaglandin analogue (Latanoprast): increase uveoscleral outflow
2nd Line:
- Topical beta-blocker (Timolol): reduce production of aqeuous humour
- Topical carbonic anhydrase inhibitor (Dorzalamide): “
- Topical sympathomimetic (Brimonidine):” and increases uvoscleral outflow
3rd Line:
- Trabeculotomy or Laser Trabeculoplasty: path from sclera to conjuctiva by bleb

What are some complications of a trabeculotomy?
- Early failure
- Hypotony
- Bleb leakage
- Infection
What are the side effects of the following topical drugs used in treatment of open angle glaucoma:
- Lanatoprost
- Timolol (beta blocker)
- Brimonidine (alpha agonist)
- Dorzalamide
- Pilocarpine

- Lanatoprost: eyelash growth, iris browning, skin pigmentation
- Timolol: dry eyes, corneal anaesthesia, reduced exercise tolerance, be careful in heart failure and asthma as can be absorbed systemically
- Brimonidine: lethargy, dry mouth
- Dorzalamide: lethargy, reduced K+, dyspepsia, avoid in pregnancy
- Pilocarpine: brow ache, decreased visual acuity
ALL DROPS CAN BE ABSORBED SYSTEMICALLY SO S/E

What is blepharitis and how is it managed?

- Inflammation of the eyelid margins causing itchy, dry, gritty eyes
- Could be due to staphs, seborrhoeic dermatitis, or rosacea
- Management: lid hygeine, hot compress, cotton bud with diluted baby shampoo cleaning twice a day, lubricating eye drops

What is a stye and how is it managed?
Hordeolum externum: Infection of the glands of Moll (sweat) and glands of Zeiss (sebaceous). They point outwards and are a red tender lump
Hordeolum Internum: Infection of tarsal glands, points inwards, more painful, can turn into chalazion
- Mx: apply hot compress several times a day until disappears, analgesia

What is a chalazion and how is it managed?
- Inflammation of the tarsal meibomian glands due to blockage of the gland. Points inwards and is painless
- Mx: hot compress, analgesia, rarely surgery to remove
What is entropion and how is it managed?
- Lid inturning due to degeneration of lower lid fascial attachments and their muscles
- Inturned eyelashes irritate cornea and can cause corneal ulceration
Mx
- Tape lid to cheek. Use lubricating drops to prevent eye drying out
- Surgery is definitive
- Same day referall if worried about sight

What is ectropion and how is it managed?
- Eyelid turns outwards so the inner aspect of the eyelid is showing
- Can lead to exposure keratopathy
Mx:
- May need no treatment if mild
- Regular lubricating eye drops to protect tear film
- Surgery

What is trichiasis and how is it managed?
- Inward growth of eyelashes
- Pain, ulceration, corneal damage
- Mx: epilation, laser therapy if recurrent
What is Pinguecula?
- Degenerative vascular yellow-grey nodules on the conjunctiva
either side of the cornea. Can try topical steroids if inflammed - If invading the cornea this is a ptyergium
- Usually in adult male, increased hair and skin pigment, sun-related
skin damage