13. Reproductive System (TT) Flashcards
(355 cards)
What are the different endocrine steps that must be fulfilled in each parent in order for successful transmission of fertile gametes and for the maintenance of pregnancy?
- Correct chromosomal complement (chromosomal sex)
- Functional testis or ovary containing germ cells (gonadal sex)
- Possess the correct internal and external anatomical male and female genitalia (phenotypic sex)
- Demonstrate appropriate sexual behaviour patterns (behavioural sex)
In other words, in order for a fertile adult to develop, they must have the karyotype of one of the sexes, functioning gonads and correct internal and external genitalia. There may be problems with the development of any of these that cause failure of normal sexual development.
How many chromosomes do humans typically have? How many of these are sex chromosomes?
46 chromosomes -> 22 pairs of autosomes and 2 sex chromosomes

What are autosomes and how many do humans have?
Non-sex chromosomes -> Humans have 22 pairs.
What is chromosomal genotype of the sex chromosomes for males and females?
- Males = XY
- Females = XX
Describe when the sex of a human is determined and how.
- It is determined at conception
- This is when the sperm introduces either another X or a Y into the egg, making the genotype XX or XY respectively
What are gonads?
- The organs that produce the gametes
- i.e. Testes or ovaries
How does the presence of a Y chromosome affect the gonads?
It causes the somatic cells of the gonads to develop into testes rather than ovaries.
What can be said about the genes of the Y chromosome?
- Most of the genes on it are unique to this chromosome
- There are around 20 genes benefiting males on this chromosome -> 10 of these are specific to the testes
What is an X-linked inheritance?
A pattern of inheritance for a genetic condition that occurs when a copy of a gene located on the X chromosome has a genetic variant.
Which chromosome determines sex and what is the evidence for this?
- The Y chromosome actively determines maleness
- Evidence for this came from two syndromes:
- Turner’s syndrome = XO genotype -> Results in an infertile female
- Klinefelter’s syndrome = XXY genotype -> Results in an infertile male
What is Klinefelter’s syndrome and what are the symptoms?
- It is characterised by the genotype XXY
- Symptoms:
- Infertility
- Small testes

What is Turner’s syndrome and what are the symptoms?
- It is characterised by the genotype XO
- Symptoms:
- Do not produce eggs

Describe how the Y chromosome leads to male development. [IMPORTANT]
- On the Y chromosome, there is a segment called the SRY gene (sex-determining region of the Y chromosome)
- It encodes a single sex-determining transcription factor (SRY protein) that controls signalling leading to male development
- It does this because the SRY protein controls downstream gene expression that triggers a cascade of events -> First, the development of the testes, which release molecules that lead to male internal genitalia differentiation and male external genitalia, along with other male characteristics
Draw the cascade by which SRY leads to differentiation of the entire male reproductive system. [IMPORTANT]

What does TDF stand for and what is it?
- Testes-developing factor
- It is another name for the SRY protein that determines testes development
What does SRY stand for?
Sex-determining region Y
What is the evidence for the importance of SRY is determining maleness?
- Humans with one Y chromosome and multiple X chromosomes are usually male -> Due to the presence of the SRY gene
- XX males (XX male syndrome, infertile) -> In this SRY gene is translocated to one of X chromosomes
- XY females -> This occurs due to the lack of, or mutation in SRY
Is the whole Y chromosome required for development of the male sex? What is the experimental evidence for this?
- Only the SRY region is required
- Experiments in mice show that introduction of the SRY region alone into XX mice is sufficient to give rise to male testes, internal genitalia and external genitalia
- However, these are not completely male because other genes on the Y chromosome are required for different characteristics -> For example, sperm cannot survive in the XX environment, making these mice infertile
What is the ‘default’ sex?
- The need for SRY to produce testes and male genitalia suggests that females are the ‘default’ sex
- However, the presence of two copies of the DAX-1 gene in an XY organism, can cause reversal to the female sex -> It has been suggested that DAX-1 acts as an ‘anti-testes’ factor
What are the different parts of the reproductive system that must form in development?
- Gonads
- Internal genitalia
- External genitalia
Does the presence of an XX or XY karyotype necessarily mean that ovaries or testes will form?
No, there may be problems in their development.
What are the main stages of the development of the gonads?
- Formation of a gonadal ridge
- Migration of primordial germ cells
- Differentiation of the undifferentiated gonad into either the testes or ovaries
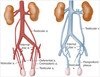
Describe in detail the process of gonad development. [IMPORTANT]
- Intermediate mesoderm gives rise to not only the nephric structures, but also a gonadal ridge on the medial aspect near the mesonephric region (in 5th week) -> This is induced by WT1, SF1 and LHX9, and it also involves the migration of primordial germ cells from the yolk sac via the hindgut
- There is continued migration of these primordial germ cells, and in the 6th week somatic support cells from the coelomic epithelium invest these cells and associate with them. Structures known as sex cords are formed by the support cells.
- Now the processes diverge for males and females.
In males:
- The sex cords proliferate by mitosis to give the testis cords (made of somatic support cells), which contain the germ cells trapped inside. The presence of SRY induces somatic support cells around the germ cells to form Sertoli cells. The primordial germ cells inside are now called the prospermatogonia.
- The primordial cells concentrate in the medulla and the cortex regresses.
- The testis cordis become canalised at puberty and differentiate into seminiferous tubules (site of the germination, maturation, and transportation of the sperm cells within the male testes).
- The Sertoli cells organise into the rete testis (network of delicate tubules that carries sperm from the seminiferous tubules to the efferent ducts)
- Leydig cells form and can secrete testosterone from the 8th week.
In females:
- The sex cords dissociate. The absence of SRY means that the somatic support cells instead differentiate into primitive follicle cells that envelope the germ cells, so that the primordial germ cells are in nests. These will become the primordial follicles. Meiosis commences but then arrests in the foetus. Primordial follicles start to develop but undergo apoptosis until puberty.
- The primordial follicles concentrate in the cortex and the medulla regresses.
- Oogonia proliferate.
The gonads then descend with the help of the gubernaculum, which is a ligamentous structure.
What part of which germ layer do the gonads form from?
Intermediate mesoderm (just like the kidneys and adrenals)