11. Myositis Flashcards
What are the two main forms of Idiopathic Inflammatory Myopathies (IIM)?
Polymyositis
Dermatomyositis
(also: Inclusion body myositis, cancer-related myositis, collagen vascular disease-related myositis)
Myositis: what is the primary problem?
muscle weakness
IIM: define.
(pattern of onset? fixed v dynamic weakness? prox or distal muscles)
Slowly progressive, FIXED muscle weakness of proximal muscles
(Fixed meaning that the muscles are weak all the time)
IIM: what is the main lab finding?
Is there associated pain?
Puts you at increased risk for what?
Main lab finding: elevated CPK
Pain: not the primary feature, but there are post-exertional aches, cramps
Increased risk for malignancy
When I diagnose Myositis, what other diseases do I need to keep a lookout for?
Pulmonary involvement, malignancies
Polymyositis: Criteria? (5)
- Symmetrical weakness of limb-girdle muscles and anterior neck flexors
- Muscle biopsy evidence of necrosis of Type I and II fibers, phagocytosis, regeneration, variation in fiber type with inflammatory exudation.
- Elevation in serum or skeletal-muscle enzymes.
- Electromyographic triad of short, small, polyphasia motor units, fibrillations and sharp waves; and bizarre, repetitive discharges.
- Dermatologic features.
Bottom line: Muscle weakness with add’l findings on histology, labs, EMG, and skin
Both myopathies and neuropathies have muscle weakness. What is the pattern for each that allows us to distinguish them?
Myopathies:
Proximal, symmetric
Neuro Exam normal
Neuropathies:
Proximal, distal or asymmetric
Other findings on neuro exam
What is the most commonly measured enzyme when myopathy is suspected?
What else can be elevated?
CPK is most commonly ordered.
Aldolase, AST, ALT, LDH can also be elevated
Beyond a myopathy, what else can cause elevated CPK?
What is the most frequent reason for checking CPK?
MI, racial differences, trauma, exercise, drugs, genetic disorders, large muscle mass can elevate CPK.
Acute MI is most frequent reason to check.
What is a ‘normal’ CPK level?
What level should cause concern?
Normal: up to 200
If CPK is over 1000, be concerned. This is not likely due to one of the benign reasons for elevated CPK
CPK: good lab to follow to assess disease progression or treatment?
NO, it can be normal in pts with a myopathy, and it does not correlated with disease activity.
What can an EMG/nerve conduction study help me determine?
- Can differentiate between myopathic and neuropathic disorders. **most impt**
- can help localize the affected area
- can identify a good site to biopsy
How can MRI help me diagnose and treat myopathy?
can see increased fluid in muscle tissue, which indicates inflammation. tells us where to biopsy for diseased tissue.
MRI of the thigh. What’s going on in the top, middle, bottom pics? Where should I biopsy?

Top: normal.
Middle: areas of increased lightness = inflammation. Note patchiness. Biopsy these areas.
Bottom: different window that suppresses fat signal, brings out muscle tissue.
Polymyositis: what kinds of cells will you see on biopsy of the muscle tissue?
What will the pattern of inflammation be?
Will see cytotoxic CD8+ T cells invading muscle fibers.
DIFFUSE pattern. primarily invading muscle fibers rather than blood vessels.
This is a histo pic of normal muscle, just for reference

Ok.
Muscle histo of what disease process? what is notable?
This would stain + for what type of lymphocytes?
Polymyositis.
Note muscle atrophy, damage, inf cells
Would stain + for CD8+ T lymphs
What disease process?
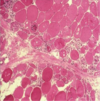
Polymyositis
Polymyositis: process of making the diagnosis?
-Rule out confounders (neurologic disease, muscular dystrophies, etc.)
Check for elevated muscle enzymes.
-Perform EMG and imaging (MRI).
-Muscle biopsy to confirm the diagnosis.
Dermatomyositis: definition?
Polymyositis plus rash!
Which is more likely to be associated with malignancy: polymyositis or dermatomyositis?
dermatomyositis.
Dermatomyositis: associated symptoms?
- Lilac (heliotrope) rash/discoloration of eyelids
- Periorbital edema
- Scaly, erythematous rash over MCP and PIP joints (Gottron’s sign)
- Rash over knees, elbows, medial malleoli
- Rash over face, neck, and upper torso (shawl sign, V-sign)
- Capillary nail fold changes and periungual erythema
What would we call this rash/pattern? Which myopathy is it associated with?

Shawl or V pattern
Dermatomyositis
What would we call this finding on his eyelids? What myopathy is it associated with? Why is there a tarp on the wall?

Heliotrope rash (lilac, on eyelids)
Dermatomyositis
No idea.
What is this rash called? Associated with what myopathy?

Gottran’s sign: Scaly, erythematous rash over MCP and PIP joints
Dermatomyositis
What is going on with this capillary bed? Associated with what myopathy?
Also associated with what 2 other diseases?

Upper L: normal
Upper R: redness
Lower pics: hemorrhage, dilation.
Dermatomyositis (also scleroderma, lupus)
Dermatomyositis: what kind of lymphoctes? what is pattern on biopsy?
B lymphs, CD4+ T cells
Perivascular pattern (rather than diffusely in fibers, as with polymyositis)
This muscle biopsy shows what disease process? what is notable?

Dermatomyositis
Note areas of normal muscle, with inflammation and atrophy around vessels
What lab is positive in 90% of myopathies?
ANA (anti-nuclear antibody)
Polymyositis and Dermatomyositis: what is the most common extramuscular target organ?
Lungs: can lead to pulm disease, pneumonia, alveopitis, fibrosis.
If a patient is positive for Jo-1 auto-antibody, what can you conclude?
What does Jo-1 target?
Pt has myositis. (most common myositis specific antibody).
Targets anti-histidyl tRNA synthetase
–> “Anti-synthetase syndrome”
If a patient is positive for Ro, La, or RNP, what can we conclude about their myositis?
Suggests that myositis is secondary to another autoimmune condition (Lupus, Sjogren’s)
If pt is positive for SRP, what can we conclude
SRP is associated mainly with polymyositis. Indicates a severe myopathy, refractory to treatment.
Define Anti-synthetase syndrome
Polymyositis or Dermatomyositis associated with anti-Jo-1 antibody.
Strong association with interstitial lung disease!
(also associated with Raynaud’s, arthritis, mechanic’s hands)
Pulmonary manifestations of anti-synthetase syndrome?
- Interstitial lung disease – inflammation leads to fibrosis
- Muscle weakness contributes to impaired breathing.
- Pharyngeal weakness can lead to aspiration pneumonitis
What types of malignancies do patients tend to get if they have malignancy associated with polymyositis or dermatomyositis?
Malignancies that are common to their current demographic (gender, age). So make sure your patients are up to date on their normal screenings.
Juvenile Dermatomyositis: what are the findings?
Like adult form PLUS:
-Vasculitis
-Lipodystrophy (changes in fat
distribution, often of face)
-Calcinosis (firm, painful CA nodules under the skin)
Amyopathic Dermatomyositis: how is it different from normal dermatomyositis?
Only the derm findings of dermatomyositis.
(pt has normal muscle strength, normal enzymes, normal histo)
May progress to the normal version.
Treatment for polymyositis and dermatomyositis?
Steroids. Prednisone.
Rhabdomyolysis: refers to what process of the muscle?
Rhabdomyolysis = Muscle necrosis.
Rhabdomyolysis: what test should I run? what might the result be?
CPK
levels will be HIGH (10,000 to 100,000+)
Rhabdomyolysis: causes?
Traumatic
Ischemic
Hyperthermia
Drugs/toxins (both prescription and illicit drugs)
Infection (bacterial/viral)
Metabolic
Drug-induced myopathies: what are the most common culprits?
STATINS
Steroids (esp prednisone)
(also: illegal drugs, EtOH, antimalarials, AZT)
Statin-induced myopathy: when should I suspect this? what dose of statin is required? how to treat?
Suspect with symptoms of myalgia, weakness in pt on statins
can occur with any dose of statin, at any point, but most common with higher doses and within first few months
Stopping the statin usually does the trick.
Steroid-induced myopathy: what is the primary manifestation?
Is this inflammatory? What is the cause?
How to dx, treat?
WEAKNESS.
Not inflammatory: due to Type II muscle fiber atrophy
Can occur with any dose of steroid, but more common with higher doses, with prolonged use
Dx: reduce steroid, see if it improves. Should see improvement within 24-48h.
Metabolic myopathy: what are these? What is the cause?
abnormalities in muscle energy metabolism, resulting in altered skel muscle function.
Genetic causes, may also be secondary to something else.
How will I distinguish a polymyoathy or dermatomyopathy from a metabolic myopathy?
Metabolic: sx are often DYNAMIC. get fatigue with exercise, feel ok at rest.
May be cardiac involvement, neuro deficits.
What are some causes of secondary metabolic myopathies?
Endocrine probs:
- hyper and hypo thyroid
- Acromegaly
- Cushing’s
- Hyper PTH
Elecrolyte disorders (Na, K, Ca, P, Mg)
Vit deficiency
Polymyalgia Rheumatica: is it a myopathy? how does it present?
What will the CPK level be?
is NOT a myopathy but easily confused with one.
RAPID onset of hip and shoulder PAIN.
CPK level will be normal.
Polymyalgia Rheumatica: what labs will be elevated?
inflammatory markers: ESR, CRP.
Polymyalgia Rheumatica: treatment? response to treatment?
Prednisone!
Often results in dramatic/rapid improvement (may be overnight)
Clinical pearl: what are the most common reasons for muscle weakness that are not myopathies?
Common things are common!
Hypothyroid, hypokalemia, EtOH abuse
Clinical pearl: minor elevations in CPK are not always pathologic: what might they be due to?
racial differences, body habitus, exercise, etc.


