Wk 1 - Quiz + Case Study: Patient with Stomach Upset Flashcards
T or F: Simple antacids such as Rennies and Gaviscon are composed of magnesium trisilicate and/or aluminium hydroxide.
True
T or F: Alginate-containing antacids form a gel or ‘foam raft’ in the stomach.
True
T or F: Simple antacids work by neutralising stomach acid
True
In addition to GORD, can you name any other oesophageal disorders in which regurgitation can occur?
- Achalasia
- Oesophageal pouch
- Benign oesophageal strictures
- Rumination syndrome
T or F: Helicobacter pylori produces urease and a sheath.
True
T or F: Helicobacter pylori is a Gram-positive spirillum.
False (it is a gram-negative, spiral-shaped bacterium)
T or F: 95% of patients with duodenal ulcers are infected with Helicobacter pylori.
True
T or F: Animals can harbour their own species of Helicobacter that can be transmitted to humans.
True (e.g. H.Heilmannii in cats, dogs, pigs and cattle)
T or F: 30% of the world’s population carry Helicobacter pylori.
False (50-60% people world-wide carry Helicobacter pylori; up to 90% in developing countries)
What are the risk factors for hiatus hernia? List 6.
- Aged over 50
- Being overweight
- Being pregnant
- Smokers/cough that increase intra-abdominal pressure
- Weakening of the diaphragm muscle with age
- Present at birth due to developmental abnormality
What is the difference between a rolling hiatal hernia and a sliding hiatal hernia?
- In sliding HH, which is the most common type, the sphincter that forms a valve between the oesophagus and stomach slides up through the diaphragm.
- In rolling para-oesophageal HH, part of the stomach bulges up through the hole in the diaphragm alongside the oesophagus.
Which is more common sliding HH or rolling (para-oesophageal) HH?
Sliding hernia is more common
What are the two main forms of oesophageal cancer?
- Adenocarcinoma
- Squamous cell carcinoma
Squamous cell carcinoma occurs in the ________ of the oesophagus.
Squamous cell carcinoma occurs in the middle third of the oesophagus.
Adenocarcinoma occurs in the _____ of the ____ and at the ____.
Adenocarcinoma occurs in the lower third of the oesophagus and at the cardia.
In the oesophagus, which is more common adenocarcinoma or squamous cell carcinoma?
Adenocarcinoma
List a risk factor for both adenocarcinoma and squamous cell carcinoma.
Smoking
What are some risk factors for adenocarcinoma?
- Long-standing GORD
- Barrett’s Oesophagus
What are some risk factors for squamous cell carcinoma?
- Excess alcohol consumption
- Plummer-Vinson syndrome
- Achalasia
- Coeliac disease
- Tylosis (rare autosomal dominant disease
- Vitamin deficeint diet
Your patient is 55 years old and has indigestion but also presents with the following:
- Unintended weight loss
- Indigestion symptoms for the first time
- Severe pain
- Vomiting specks of blood
What is your initial diagnosis and what course of action do you suggest?
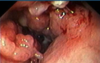
It is most likely to be dyspepsia. But they could be indicative of an ulcer or cancer. I would recommend hospital referral for gastroscopy and follow-up tests.
How does Omeprazole?
Proton pump inhibitor that inhibits gastric hydrogen-potassium-ATPase. PPI drugs will produce almost complete reduction in secretion of gastric acid.
What is usually the first line of investigation when someone presents with persistent GORD?
Gastroscopy - oesophagogastroduodenoscopy (OGD)
What is dysphagia?
Difficulty swallowing due to a local lesion. Pts often complain of ‘something sticking in my throat of chest’ during or immediately after swallowing.
List 7 ‘alarm signals’ associated with heartburn/dyspepsia type symptoms.
- Chronic GI bleeding
- Progressive unintentional weightloss
- Progressive difficulty swallowing
- Persistent vomiting
- Iron deficiency anaemia
- Epigastric mass
- Suspicious barium meal