Week 7 Flashcards
(119 cards)
What is the location of the thyroid in the body?
- Two lobe located in lower neck, anterior and anterolateral to the trachea
Blood supply of the thyroid?
- Blood supply
- R + L superior thyroid arteries (from external carotid arteries)
- R + L inferior thyroid arteries (from thyrocervical trunks)
Venous drainage of the thyroid
- Venous drainage
- R + L superior thyroid veins (into IJ veins)
- R + L middle thyroid veins (into IJ veins)
- R + L inferior thyroid veins (into brachiocephalic veins)
What is important to know about the recurrent laryngeal nerves? Also what is their function?
- R+L Recurrent laryngeal nerves
- Sensory below the vocal cords and motor function to all intrinsic muscles of the larynx
- Risk of damage during thyroidectomy
How many parathryoid glands are there? Where are they located?
Blood supply of parathyroid?
Parathyroid Glands
- 4 glands (2 on each side) located in posterior region of each thyroid lobe
- Inferior thyroid arteries supply 100% of the inferior parathyroid glands and 85% of superior parathyroid glands
- Superior thyroid arteries supply 15% of the superior parathyroid glands
What is the pathway of the hypothalamic-pituitary-thyroid axis?
How does negative feedback occur?
Regulation of Hypothalamic-Pituitary-Thyroid Axis
- Pathway: Hypothalamus releases TRH → anterior pituitary release TSH → TSH stimulates gland growth → TSH stimulation + dietary iodine → T4 and T3 (less) release
- Negative inhibition: TRH and TSH release inhibited by high levels of T3 and T4
How is the thyroid hormone synthesized? Provide a detailed pathway!
- Pathway:
- TSH binds to TSH receptor (basolateral) → activates Na-I symporter (basolateral) → iodine enters cells → iodine exits cell at apical side via Pendrin
- Synthesis of thyroglobulin (Tg) in ER of cell → Tg secreted at apical side of cell → thyroid peroxidase (TPO) located on apical surface catalyzes reaction between iodine and Tg → Tg-T3/4 → Tg-T3/4 enters cells → exits basolateral side of cell as T3 or T4
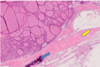
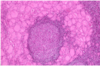
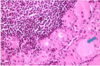
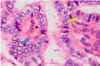
Know this image.

yeah.
How much of thyroid hormone is bound? What is it bound by?
- BOUND (99.95%) – to serum carrier proteins, which are made by the liver
- Thyroxine-binding globulin (TBG) – principle binding protein
- Thyroxine-binding prealbumin (transthyretin)
- Albumin
How much of thyroid hormone is free? What functions and actions does free thryoid hormone have?
- FREE (0.05%) – metabolically active form responsible for hormonal activity
- Available to peripheral tissues for intracellular transport
- Participates in negative feedback regulation
- Undergoes degradation and excretion
How does the conversion of T4 to T3 occur? What enzyme is involved? What’s so special about T3?
Peripheral Conversion of T4
- Serum T4 converted to T3 by intracellular 5’-deiodinase (D1) enzyme in many peripheral tissues
- Accounts for 85% (most) of body’s T3
- T3 is the biologically active and most potent form of thyroid hormone
- T4 converted to inactive reverse T3 (rT3) by peripheral tissues
What is the general mechanism of thyroid hormone? How does it act on peripheral tissue?
Give some examples of what would occur when thyroid hormone acts (hypothalamus, pituitary, beta receptors)
- MOA: binding to nuclear receptor at target tissues → interact with thyroid hormone response elements (TREs) sequences upstream of target gene promoters → regulation of gene expression
- Ex: T3 decreases gene transcription of TRH (hypothal) and TSH (pituitary) = gives NEGATIVE FEEDBACK
- T3 increases gene transcription of b-adrenergic receptors in heart, liver, muscle, adipocytes
What effects does thyroid hormone have on the following:
- BMR?
- O2/CO2
- Carbs/lipids/proteins
- Bones, intestines
- Metabolic
- Overall, increases Basal Metabolic Rate (BMR) and affects oxidative metabolism
- Increase O2 consumption, CO2 production, thermogenesis
- Affects Carbohydrate, lipid, and protein metabolism
- Increases glycogenolysis, gluconeogenesis, lipolysis, proteolysis
- Increase bone turnover, intestinal motility, erythropoiesis
- Normal CNS function
What effects does thyroid hormone have on the following:
- adrenergic?
- Brain?
- Bones?
- Sexual characteristics?
- Potentiates adrenergic stimuli/catecholamines
- Positive chronotropic and inotropic effect – increases HR and CO; decreases SVR
- Promotes normal Growth and Development
- Brain development and maturation
- Skeletal and muscle growth and maturation
- Sexual maturation
What is the best way to test your thyroid initially?
- Measurement of TSH level (highly sensitive; best initial test for primary thyroid dysfunction)
What are two other measurements of thyroid (other than TSH)?
- Measurement of circulating thyroid hormone levels
- FREE serum T4 (FT4) and free T3 (FT3) = most important
- TOTAL serum T4 (TT4) and T3 (TT3)
What are some things that can increase your total serum T4? How does this occur?
- Increase thyroid hormone binding proteins (increase total hormone levels):
- Hyperestrogenic states (estrogen Tx, pregnancy)
- Drugs (heroin, methadone, clofibrate, 5FU, major tranquilizers)
- Acute hepatitis
- Congenital TBG excess
What are some things that can decrease your total serum T4? How does this occur?
- Decrease thyroid hormone binding proteins (decrease total hormone levels due excessive negative feedback):
- Drugs (androgenic steroids, glucocorticoids, L-asparaginase)
- Protein malnutrition or loss (nephrotic syndrome, protein losing enteropathy)
- Cirrhosis
- Major systemic illness
- Congenital TBG deficiency
For the following conditions, know concentration of binding proteins, total plasma T4/T3, free plasma T4/T3, plasma TSH, and clinical thyroid state:
- Hyperthyroidism
- Hypothyroidism
- Estrogens, methadone, heroin, etc
- Glucorticoids, androgens, danazol

Describe thyrotoxicosis.
- Description: hypermetabolic state and increased sympathetic tone due to excessive thyroid hormones
List symptoms/signs of thyrotoxicosis.
- Clinical features: heat intolerance (due to high BMR), tachycardia/palpitations, arrhythmias (A-fib), weight loss (high BMR), nervous/tremor (increased sympathetic), warm/moist skin, excessive sweating, proximal weakness (proteolysis), frequent bowel movements, oligomenorrhea (prolactin induced), bone resorption, hypocholesterolemia (increased LDLr), hyperglycemia (gluconeogenesis)
What are labs of thyrotoxicosis?
- Dx: decreased TSH, increased T4
What are some treatments of thyrotoxicosis?
- Treatment: beta blockers, thionamides (methimazole, propylthiouracil), radioactive iodine (I-131 ablation), surgery (thyroidectomy)
What is the biggest complication of thyrotoxicosis? List pathophys, labs, and treatment for this.
- Complication: thyroid storm
- Pathophysiology: underlying hyperthyroidism + acute stress → elevated catecholamines → hormone excess → arrhythmias/hyperthermia/hypovolemic shock/coma
- Labs: increased LFTs
- Tx (4 Ps): propranolol, propylthiouracil, prednisolone, potassium iodide