Week 2 Flashcards
(89 cards)
What is the role of the hypothalamus and name 3 nuclei that are part of it?
- Hypothalamus maintains homeostasis by releasing tertiary-releasing hormones
- Nuclei involved: arcuate n. (releases GnRH), paraventricular n., and supraoptic n.
Where is the pituitary located and name the two parts of the pituitary?
- Pituitary: located at the base of the brain, comprised of adenohypophysis (anterior pituitary), neurohypophysis (posterior pituitary)
What does the HPG axis develop from embryologically?
- Development of HPG axis:
- Hypothalamus: develops from diencephalon
- Pituitary
- Adenohypophysis: develops from epithelial cells from infundibulum (roof of oral cavity)
- Neurohypophysis: downgrowth of the diencephalon
What is the action of the hypothalamus in release of GnRH? Provide the pathway including the nucleus that it comes from.
- Hypothalamus
- Action: Arcuate nucleus → parvicellular neurons to median eminence → release of GnRH
What is the action of the anterior pituitary when it receives GnRH? What does it produce and release? Provide the full pathway end to end.
Explain what causes certain hormones to be released.
- Anterior Pituitary
- Action: GnRH binds to GnRH receptor on basophil cells → GPCR pathway activated → activation of gonadotrope cells → production of luteinizing hormone (LH) and follicle stimulating hormone (FSH)
- FSH and LH are not co-secreted
- Fast GnRH pulses = LH, Slow GnRH pulses = FSH
- FSH and LH are not co-secreted
- Action: GnRH binds to GnRH receptor on basophil cells → GPCR pathway activated → activation of gonadotrope cells → production of luteinizing hormone (LH) and follicle stimulating hormone (FSH)
What are the endocrine targets of LH and FSH?
- Endocrine targets
- Ovaries and Testis: production of sex steroids
What are the two compartments of the lobules of testes and what kind of cells do they each have. What receptors are on these cells?
- Testis (males): divided into lobules which contain two compartments
- Intratubular compartment: contains Sertoli cells (SC), which express androgen and FSH receptors
- Peritrubular compartment: contains the Leydig cells (LC)
What is the endocrine function of Sertoli Cells? Explain the process of how they do what they do?
What are the three things that they produce?
- Intratubular compartment: contains Sertoli cells (SC), which express androgen and FSH receptors
- Endocrine function: FSH binds to FSHr on SC → production of sperm
- Sertoli cells produce: aromatase (converts androgen to estradiol 17-B), inhibin, and androgen-binding protein (ABP)
- Endocrine function: FSH binds to FSHr on SC → production of sperm
What is the endocrine function of Leydig Cells? Explain the process of how they do what they do?
- Peritrubular compartment: contains the Leydig cells (LC)
- Endocrine function: LH binds to LHr on LC → production of testosterone
- LC is steroidogenic (synthesizes steroids de novo from cholesterol)
What are three main target organs of testosterone? Explain what occurs at each organ!
- Target organs of testosterone
- Seminiferous tubules: collected by ABP
- Periphery/adipose tissue: testosterone → estrogen via CYP19
- Other (i.e. prostate): testosterone → DHT via 5alpha-reductase
What are the two cell types of ovarian follicles? What receptors do they express and what occurs at each cell type?
- Ovarian follicle (females):
- Two cell types:
- Granulosa cells: express FSHr, but no production of hormones
- Convert androgen → estradiol-17B (estrogen) + inhibin B
- Thecal cells: express LHr and produce androgens (androstenedione) and small amounts of testosterone
- Granulosa cells: express FSHr, but no production of hormones
- Two cell types:
What is the order of follicle growth? What hormone do the follicles become more dependent on as the antrum size increases?
Primoridal follicle, secondary follicle, tertiary follicle, graafian/dominant follicle, pre-ovulation, corpus luteum
FSH
Explain what occurs at the primoridial follicle and the secondary follicle?
- Primordial follicle: growth process is independent of HPG axis (no steroid hormones produced)
- Secondary follicle:
- Granulosa cells are inactivated at this stage
Explain what occurs at the dominant follicle!
- Graafian/dominant follicle: increasing amounts of estrogen are released here due to upregulation of CYP19
Explain what occurs pre-ovulation. What hormone surges? What hormone production is inhibited? What three things increase in expression?
- Pre-ovulation: buildup of estrogen provides positive feedback to hypothalamus to stimulate LH surge → ovulation
- Mural granulosa cells: estrogen production is inhibited
- Expression of StAR protein, CYP11A1, and 3beta-HSD increase → production of progesterone, which is stimulated by LH binding to LHr on mural granulosa cells
- Mural granulosa cells: estrogen production is inhibited
What is produced during corpus luteum? What happens when fertilized and if not fertilized?
- Corpus luteum
- Produces decreasing amounts of progesterone and inhibin A
- If fertilized: embryo releases hCG → corpus luteum remains alive for pregnancy
- If not fertilized: corpus luteum degenerates in 14 days → corpus albicans → YOU BLEED (Arsh)
- Produces decreasing amounts of progesterone and inhibin A
What are the effects of estrogen on the bone, liver, heart, CNS, and adipose tissue?
- Bone: closes epiphyseal plates
- Liver: increases circulating HDL and LDLr expression
- Heart: vasodilation and NO production
- CNS: neuroprotective
- Progesterone increases setpoint for thermoregulation and acts as a depressant
- Adipose tissue: decreases fat, especially on abdomen
Lmao, I guess make sure you understand this graph?

It is what it is.
For cryptorchidism, provide epidemiology, pathophys, complications, and treatment.
- Cryptorchidism
- Epidemiology: 4% at birth (most resolve spontaneously)
- Pathophysiology: arrest of testicular descent anywhere from intra-abdominal to intra-scrotal position
- Normal descent regulated by Mullerian inhibiting substance, androgen, and pulling of gubernaculum
- Complications: torsion, inguinal hernia, infertility, increased risk of malignancy
- Tx: perform orchiopexy if testis are undescended after 1 year
- Allows earlier detection of tumor and reduces complications
For hydrocele, provide description, epidemiology, pathophys, and diagnosis.
- Hydrocele: painless scrotal enlargement
- Epidemiology: newborns
- Pathophysiology: collection of serious fluid between parietal and visceral layers of tunica vaginalis
- Diagnosis: light to scrotum shows fluid
For testicular torsion, provide description, pathophys, complications, and tx.
- Testicular torsion: twisting of scrotal contents on spermatic cord
- Pathophysiology: high attachment of tunica vaginalis on spermatic cord → testes free to swing and tangle on spermatic cord
- Complications: Veins may become obstruction → hemorrhagic infarction
- Tx: emergent surgical correction to preserve viability
For Germ Cell Tumors of the testicles, provide epidemiology, risk factors, pathogenesis (genes), presentation, diagnosis, and types.
- Germ cell tumors
- Epidemiology: most common testicular tumor, ages 15-34, whites
- Better prognosis in infants
- Risk factors: cryptorchidism, Kleinfelter syndrome, testicular carcinoma in-situ, testicular dysgenesis syndrome, FHx of testicular GCT
- Pathogenesis: KIT-activating mutations and i(12p)
- i(12p)/CIS not associated with infant GCT
- Retain expression of NANOG and OCT 3/4 pluripotent cells
- Presentation: nodule, with dull aching pain
- Diagnosis: scrotal US, staging CT, serum markers, orchiectomy (often found by patient or partners)
- Types: seminoma and mixed GCT
- Epidemiology: most common testicular tumor, ages 15-34, whites
For seminomas of the testicles, provide epidemiology, description, diagnosis, prognosis, and pathology (gross and micro)
- Epidemiology: most common testicular tumor, not common in infants
- Description: remains localized within tunica albuginea
- Diagnosis: radiosensitive (respond to radiotherapy), HCG production is rare
- Prognosis: presents in clinical stage I (good prognosis); late metastasis
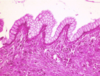
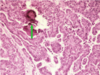
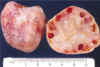
- Pathology:
- Gross: homogenous pale tan parenchyma (pic)
- Micro: fibrovascular septae with lymphocytes
For mixed GCT: provide presentation, diagnosis, prognosis, gross pathology, and the different subtypes (in order from poor to good prognosis).
Mixed GCT (NSGCT):
- Presentation: younger patients (compared to seminoma)
- Diagnosis: not radiosensitive (surgery/chemo), AFP (alpha-fetoprotein) and/or HCG biomarkers
- LDH correlates with tumor burden
- Prognosis: poor, metastasizes earlier via heatogenous/lymphatic route
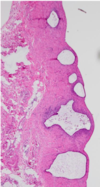
- Gross pathology: hemorrhagic/necrotic appearances
- Subtypes: from poor prognosis to better prognosis
- Choriocarcinoma:
- Embryonal carcinoma
- Yolk sac tumor:
- Teratoma