Week 4 Flashcards
(130 cards)
External obliques - attachments
What direction do the fibres of these muscles run in?
Attaches to the lower ribs (7-11, sometimes 12), pubic tubercle and linea alba
fibres run in the same line as the external intercostals, “hands in pockets”
Internal obliques - attachments
What direction do the fibres of these muscles run in?
Attachments - lower ribs, thoracolumbar fascia, iliac crest and linea alba
Fibres run in the same direction as the internal intercostals, “hands on chest”
Where does the linea alba run between?
From the xiphoid sternum to the pubic symphisis
Describe the rectus sheath. How does it differ…
- above the arcuate line
- below the arcuate line?
Why does this change occur?
The rectus sheath is immediately deep to the superficial fascia and is a combined aponeuroses of the anterolateral abdominal wall muscles (external ob., internal ob., and transv. abdo.)
- Above the arcuate line, the rectus sheath is split into anterior and posterior leaflets. The anterior leaflet is made up of the external oblique aponeurosis and the anterior portion of the internal oblique aponeurosis. The posterio leaflet is made up of the posterior part of the internal oblique aponeurosis and the transverse abdominis.
- Below the arcuate line, the rectus sheath is all anterior
This change occurs because abdominal organs sit lower in the body due to gravity - having all components of the sheath anteriorly provides more protection for the muscles

The spermatic cord in the male and the round ligament of the uterus in the female pass through which layer of the rectus sheath?
What does this layer become incorporated into in the male?
The spermatic cord and the round ligament pass through the transversalis fascia at the entrance to the deep inguinal ring
In the male, the transversalis fascia extends downwards as the internal spermatic fascia

What nerves supply the anterolateral abdominal wall? From what direction do they enter?
Nerves enter from the lateral direction
The 7th-11th intercostal nerves go on to become the thoracoabdominal nerves after they cross over the costal cartilage
Other nerves involved include subcostal (T12), iliohypogastric (L1) and ilioinguinal (L2)

Describe the arterial supply to the anterolateral abdominal wall
Superior epigastric artery (1.6mm)
- continuation of the internal thoracic arteries
- emerges at the superior aspect of the abdominal wall
- lies posterior to rectus abdominis
Inferior epigastric artery (3mm)
- branch of the external iliac artery
- emerges at the inferior aspect of the abdominal wall
- also lies posterior to rectus abdominis

What layers are passed through when performing a LSCS (lower segment caesarean section) incision?
What other procedure should be performed to make this incision easier?
Skin and fascia
(anterior) rectus sheath as below the arcuate line
Separation laterally of the rectus abdominis muscles
Transversalis fascia and peritoneum
Retract the bladder (urinary catheterisation can be performed to aid this)
Uterine wall
Amniotic sac

What layers are passed through when performing a laparotomy?
These procedures are relatively bloody/bloodless. What does this mean clinically?
Skin and fascia
Line alba
Peritoneum
Relatively bloodless, which means that the wound may be harder to heal and there is an increased risk of wound herniation/dehiscence
When performing laparoscopy and using lateral ports, what vessel must care be taken to avoid?
What landmarks can be used?
When performing lateral ports, care must be taken to avoid the inferior epigastric artery
The IEA emerges just medially to the deep inguinal ring. Hesselbach’s Triangle can be used to help avoid hitting IEA (rectus abdominis medially, inguinal ligament inferiorlaterally and IEA superolaterally)

When performing a hysterectomy, what structures must be carefully avoided? How can this be done?
The ureters should be avoided - they will vermiculate when touched, while uterine arteries will appear pulsatile. Can also use the memory aid “water under the bridge” as the ureter passes inferiorly to the artery and vein

Where might a woman give birth?
Which is most common?
Consultant-led unit
Midwife-led unit
Homebirth
96% of women in the UK still give birth within a hospital setting
Describe Ferguson’s Reflex
Stretching of the cervix causes the release of oxytocin, which stimulates uterine contractions and thus further pressure on the cervix causing more release of oxytocin. POSITIVE FEEDBACK MECHANISM
What do the following hormones do with regards to the onset of labour?
- Progesterone
- Oestrogen
- Oxytocin
Progesterone - keeps the uterus ‘settled’, prevents the formation of gap junctions and hinders the contractibility of myocytes
Oestrogen - makes the uterus contract and promotes prostaglandin production
Oxytocin - initiates and sustains contractions and acts on the uterus lining (decidual tissue) to promote prostaglandin release. Near the end of pregnancy, the number of oxytocin receptors found in myometrial and decidual tissues increases
‘Rupture of membranes’ refers to what? When might this occur?
Refers to rupture of the liquor - fluid that nurtures and protects the foetus and facilitates movement
Timing may be…
- pre-term
- pre-labour
- first stage
- second stage
- “born in a caul”
What cervical changes occur during labour?
Cervix softens through various methods…
- increase in hyaluronic acid leads to an increase in the number of molecules among collagen fibres
- decrease in bridging among collagen fibres = decrease in firmness
- cervical ripening (decrease in fibre collagen alignment and strength, and decrease in tensile strength of the cervix matrix)
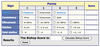
What is Bishop’s score used for? What is it made up of?
Pre-labour scoring system used to determine whether or not labour needs to be induced.
Made up of 5 elements…
- Position
- Consistency
- Effacement
- Dilatation
- Station of the pelvis
The higher the score, the more likely induction will be needed
Name the various stages of labour and what each comprises of
First stage (Latent Phase, 3-4cm dilatation, and Active Phase, full dilatation a.k.a. 4-10cm)
Second stage - delivery of baby
Third stage - expulsion of placenta and membranes
Describe the features of the First Stage of labour
Latent Phase
- mild irregular uterine contractions
- cervix shortens and softens
- duration is variable (may last a few days!)
Active Phase
- slow descent of the presenting part
- contractions progressively become more rhythmic and stronger
- analgesia, mobility and parity of the mother increase the variability of this stage
Describe the features of the Second Stage of labour
Spans from complete dilatation of the cervix to delivery of the baby
Nulliparous women
- considered prolonged if exceeding 3 hours (if regional analgesia)
- or considered prolonged if 2 hours with no analgesia
Multiparous women
- considered prolonged if exceeding 2 hours w/ regional analgesia
- or 1 hour with no analgesia
Describe the features of the Third Stage of labour
Describe the difference between expectant and active management at this stage
At what point would removal under GA be considered?
Spans from delivery of the baby to expulsion of the placenta and membranes
Average duration is 10 minutes, however can last 3 hours or longer
expectant management - spontaneous delivery of the placenta
active management - use of oxytocic drugs and controlled cord traction (lowers risk of PPH)
After 1 hour, preparations are made to remove the tissue under general anaesthetic

Explain Braxton Hicks contractions and how they differ from normal contractions.
How does having had previous children affect this phenomenon?
A.k.a. “false labour”
Tightening of the uterine muscles, thought to be in preparation for actual labour
Can start as little as 6 weeks into pregnancy, but typically occur in the 3rd trimester.
Unlike normal contraction, BH contractions are irregular and do not increase in frequency or intensity
BH contractions typically resolve with ambulation/change in activity
Previous pregnancies increase the likelihood of BH contractions due to increased uterus excitability
How can you tell if contractions are “true” and signalling real labour?
How are true contractions brought about?
Timing of the contractions become more evenly spaced and the time between them becomes shorter and shorter
The duration of each contraction also increases, and will also become more painful and intense over time
Oxytocin stimulates the uterus to contract by tightening the top of the uterus and pushing the baby inferiorly into the birth canal. This also usually promotes thinning of the uterus
Three key factors are in interplay between one another during labour, these being Power, Passenger and Passage.
Describe Power
= uterine contraction
The uterus is made up of smooth muscle and connective tissue, with a pacemaker region in the tubal ostia that causes waves to spread downwards. The waves generated from each ostia synchronise with each other
As the upper segment contracts and retracts, the lower segment and cervix relax and stretch
Normal contractions have fundal dominance
Frequency of contractions - 3-4 every 10 mins
Duration - 10-15 seconds, going up to 45 seconds







