Week 2 Flashcards
What proportion of oxygen is dissolved in the plasma? What proportion is carried by Hb?
2% in plasma (PO2) 98% with Hb (SO2)
Define O2 content, O2 capacity and O2 saturation
O2 content: the total amount of O2 in the blood (dissolved and with Hb)
O2 capacity: the max amount of O2 that can be combined with Hb (20 mL/100mL blood)
02 saturation: is the % of Hb binding sites bound to O2 (oxyHb/O2 capacity)
What is the PO2 and SaO2 of arterial and venous blood?
Arterial:
- PaO2= 100
- SaO2=100
Venous
- Pa02=40
- SaO2=75
What is the oxy-Hb dissociation curve?
A curve representing the relationship of oxygen tension and hemoglobin saturation. Each hemoglobin can carry 4 molecules of oxygen that bind cooperatively.
Describe the portions of the Oxy-Hb curve that correspond to oxygen loading and unloading.
At the lungs, Hb becomes saturated. At the tissues, a small change in pO2 results in a loarge change in oxygen saturation.

What does a rightward shift of the oxyHb curve mean? A leftward shift?
Right: Hb has lower affinity for O2
Left: Hb has higher affinity for O2
What causes a rightward shift of the oxyHb curve?
- Increased temperature
- increased pCO2
- decreased pH (Bohr Effect)
- increased 2,3 BPG (from anaerobic metabolism)
**everything that happens with exercise!
What does the oxyHb curve look like in anemia (with O2 content, as opposed to Sa02 on the y-axis)?

What is the effect of CO on oxygen content and oxygen carrying capacity in the blood?
Oxygen content decreases (because it is outcompeted by CO) and O2 carrying capacity decreases (?)(because binding spots are taken up by CO)

What is the effect of erythropoeitin (EPO) on the oxygen capacity and content of the blood?
Increases both , because you have more RBCs
What color is oxy, deoxy and carboxyHb?
- OxyHb: red
- deoxyHb: blue
- carboxyHb (COHb): cherry red (can be seen in deceased according to wikipedia)
What forms does Co2 in the blood exist in, and what is the percentage of each?
- Bicarbonate (90%)
- Disolved (5%)
- CarbaminoHb (5%)
What is the role of carbonic anyhydrase in the transport of carbon dioxide?
Carbonic anhydrase lives in red blood cells. CO2 diffuses from tissues, into the plasma and into the RBCs. There. it can either combine with Hb (carbaminoHb) or be converted to carbonic acid via carbonic anhydrase. The proton from this reaction binds Hb and does not diffuse. The bicarbonate is transported out of RBCs and Cl- is transported into RBCs to counter the bicarbonate. This is called the chloride shift.
What is the Haldane effect? What produces it?
- Deoxygenation of the blood increases its ability to carry CO2
- This is good beacuse it permits high loading of CO2 at the tissues (low pO2), and unloading of CO2 at the lungs (high PO2)
- In high pO2, oxygen binding creates conformational changes that make CO2, H+ binding less favorable
- In low pO2 (at the tissues), H+ and 2,3 BPG bind to Hb and create conformational changes that make CO2 binding more favorable.

Define bronchiectasis and list possible etiologies
Irreversible dilatation of the bronchial tree (bronchi and bronchioles) (vs. the reversible that can accompany infectious pneumonia)
Etiologies:
Congenital:
- cystic fibrosis
- primary ciliary dyskenesia
- kartagener syndromes
Post infectious
- necrotizing pneumonias (TB, HiB, S. aureus, viral, fungal (e.g. aspergillus)
Obstruction
- tumour
- foreign body
- mucus impaction
Other
- collagen vascular diseases (rheumatoid arthritis, lupus, scleraderma)
- post-transplant
Pathophysiology of bronchiectasis
Infectious: inflammation, necrosis, fibrosis, dilatation
Obstructive: secretions build up below the obstruction and inflammation ensue
Define bronchiolitis obliterans
Irreversible narrowing/compression of small airways by fibrosis, with or without inflammation
Etiology of bronchiolitis obliterans
Post-infectious
Envrionmental (fumes, dusts)
Other (post lung transplant, collagen vascular disease, drug-induced)
What is the common pathogenesis of all obstructive lung diseases?
Inflammation!
What are common symptoms of chronic obstructive airway disease?
Cough
dyspnea
wheeze
sputum production
What are 2 sources of mucus in the lung?
1) goblet cells
2) mucous glands found in cartilagenous airways
What are mechanisms of increased lung resistance (x5)?
- lumenal occlusion
- increased wall thickness
- loss of elasticity
- smooth muscle contraction
- obliteration of airways
What are the the mechanisms of increased lung resistance in COPD, bronchiectasis, bronchiolitis obliterans and asthma?
COPD: loss of elasticity, obliteration
Bronchiectasis: wall thickening, lumenal occlusion, obliteration
Asthma: smooth muscle spasm, wall thickening
Bronchiolitis obliterans: wall thickening, obliteration
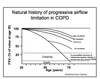
What is the natural progression of chronic obstructive airway diseases?
- A long asymptomatic period because the changes occur primarily in the small airways, and the most physiological resistance is at gen. 4/5 ish, so it takes a long time for the pathophysiological resistance to show up.
- exertional dyspnea usually comes first and progresses to dyspnea at rest.