Week 1- Myeloproliferative disorders Flashcards
(51 cards)
What are myeloproliferative disorders?
Myelo= myeloid lineage (red cells, platelets, granulocytes) Proliferative= to grow or multiply They are clonal haematopoetic stem cell disorders with an increased production of one or more types of haemopoetic cell. Basically proliferation of mature cells.
How do myeloproliferative disorders differ from acute leukaemia?
Maturation is preserved.
Which gene is responsible for the division of myeloproliderative disorders?
Presence or absence of BCRABL1 gene. If you have it- chronic myeloid leukaemia If you dont- one of the other three.
What makes up the BCRABL1 negative myeloproliferative disorders?
Polycythaemia (rubra) vera Myelofibrosis Essential thrombocytosis.
Where is BCRABL1 gene found?
On the Philadelphia chromosome.
What does chronic myeloid leukaemia cause in terms of cells?
Overproduction of granulocytes.
What does essential thrombocytosis cause in terms of cells?
Overproduction of platelets.
What does polycythaemia rubra vera cause in terms of cells?
Overproduction of red cells.
When would you suspect myeloproliferative disorders?
When there is: High granulocyte count +/- High red cell count +/- High platelet count +/- Eosinophillia/basophillia Splenomegaly thrombosis in an unusual place.
Which myeloproliferative disorder is splenomegaly most commonly associated with?
Myelofibrosis. However can be seen in the others.
In chronic myeloid leukaemia, what is blast crisis?
When you get proliferation of blast cells (so it appears like acute myeloid leukaemia) however it is a very late stage of chronic myeloid leukaemia.
What are the clinical features of chronic myeloid leukaemia?
Splenomegaly Hypermetabolic syndromes- increased rate. Gout Problems in the blood due to increased viscosity.
What laboratory features are there of chronic myeloid leukaemia? Think about blood counts etc.
Chronic myeloid leukaemia- lots of mature cells proliferating. Therefore normal Hb/decreased Hb. Leucocytosis, neutrophillia and myeloid precursors, eosinophilia, basophilia (not many conditions cause a rise in basophils however CML does).
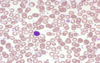
Which type of cell are the arrows pointing too in this picture? Also which myeloproliferative disorder does this indicate?

Eosinophils are shown- they have red granules in their cytoplasm.
Likely to be chronic myeloid leukaemia as there is basophillia and eosinophillia which are unlikley to be seen outwith this disease.
Which chromosomal abnormalitity is said to be the hallmark of chronic myeloid leukaemia? What changes to this chromosone produce which specific gene that causes CML?
The phillidelphia chromosone.
Translocation between chromosone 9 and 22. Causes BCR and ALB genes to stick together- causing BCR ABL causative gene.
What is the product of having the BCR-ABL gene?
What does this mean for treatment?
Causes a tyrosine kinase which causes abnormal phosphorylation (signalling) in the myeloid pathway leading to the haematological changes in CML.
Durable diseases may respond to tyrosine kinase inhibitors.
NOTE- the BCR ABL negative diseases may overlap so there may be difficulty distinguishing between them.
Name some common features of myeloproliferative disorders?
Asymptomatic- commonly picked up by chance due to people having blood tests done.
Increased cell turnover-e.g. gout, fatigue, weight loss, sweats.
Symptoms or signs due to splenomegaly
Why do you get a low haemoglobin in chronic myeloid leukaemia?
It stops the ability of the bone marrow to make normal healthy blood cells, meaning that anaemia will occur.
Describe this blood test:
What are you worried about?

This person has a low Hb- normocytic anaemia (due to MCV being normal)
High platelets- thrombocytosis
High WBC- leucocytosis- specifically neutrophils, eosinophils and basophils (neutrophillia, eosinophillia and basophillia)
In this patient you are worried about chronic myeloid leukaemia.
Describe this blood test?
Are you worried about chronic myeloid leukaemia in this case?

Hb is low- normocytic anaemia (as MCV is normal)
Raised WBC count- leucocytosis
Raised platelets- thrombocytosis
This person has a neutrophillia but the basophils and eosinophils are within the normal range
You are not worried because the clinical history suggests infection (empyema) which would also cause these blood results. Cancer investigation is only warranted if the clinical picture also fits.
What drug can be used for chronic myeloid leukaemia? Explain why?
Tyrosine kinase inhibitors e.g. imatinib
(tyrosine kinase causes abnormal phosphorylation leading to the haematological changes)
Describe the bloods in polycythaemia rubra vera?
High haemoglobin/haematocrit with erythrocytosis (a true increase in red cell mass). There can be excessive production of other lineages.
What is polycythaemia rubra vera important to distinguish from?
Secondary polycythaemia- chronic hypoxia (e.g. in COPD patients), erythropoetin secreting tumours)
Pseudopolycythaemia-e.g. dehydration, diuretic therapy. Concentrates the blood making the red cell mass SEEM more than normal. You will see an increase in haematocrit.