Week 1 & 2 Intensive Flashcards
What are the effects/ side effects of Barbiturates?
* CNS: depression, GABA receptors (inhibitory neurotransmitters bind), NO analgesia
* CV: increase in HR, decrease in arterial BP (decrease peripheral resistance, decrease SV, myocardial contractility), increased sensitivity of myocardium to cirulating catecholamine (arrhythmias common at induction)
* Resp: post-induction apnoea common especially following opioid premed, decreased ventilatory rate and tidal volume
How can you monitor the time, temperature and air removal of the steam sterilisers? Which class do you want?
* Chemical indicators
* Want class 6: it covers all variables with greater specificity/ reliability.. where class 1 changes colour to indicate it has been exposed to heat only
What are the disadvantages of inhalation anaesthetics?
* Requires expensive equipment (anaesthetic machine and vaporizer, breathing circuit and scavenger system)
* Must have an intimate understanding and know how to trouble shoot this equipment
* Must test this equipment before each case, and perform regular maintenance
* Significant dose-dependent depression of CV and respiratory function
What is different about monitoring small ruminants under GA?
* Rotation of the eye is not a useful indicator of anaesthetic depth
* HR should be within normal limits, 80-120 beats
* RR should be between 20 and 40 breaths/min
What would you tell the owner?

50% chance the dog will live for longer than 21 months with treatment. Less than 20% chance it will be alive at 2 years.
What are inhalation anaesthetics? What is vapour pressure? What is the vapour pressure for Isoflurane? What is the vapour pressure for Sevoflurane?
* Inhalation anaesthetics are volatile liquids that evaporate or vaporize at room temperature and pressure
* The vapour pressure of an inhalation anaesthetic is a measure of its ability to evaporate at a given temperature (20C) and pressure (1 atm= 760 mmHg)
* Isoflurane: 240 mmHg @ 20C and 760 mmHg
* Sevoflurane: 160 mmHg @ 20C and 760 mmHg
What side must the sheep be on for an endotracheal intubation?
Left side lateral recumbency- head going down
What is the problem with partial agonists and agonist-antagonists? How are pure agonists better?
They are unreliable, they are only “sometimes” potent analgesics
* They are reliable, best for severe pain, can be topped up
Why should you never administer anticholinergics with alpha 2 adrenoceptor agonists to offset the bradycardia?
Severe hypertension can result
When might you use Fentanyl and Alfentanil? What are the dangers?
* Fentanyl is 100 x more potent than morphine and alfentanil is 50 x more potent
* short acting agents- mainly used intra-op as bolus or infusion
* useful for animals who emerge in severe pain
* bradycardia and resp depression common!
What are repercussions of pain?
* Sleep disorders (anxiety)
* Aggressivity
* Neuroendocrine modifications- resp function, CO, decrease gastric and intestinal motility, electrolytes in balance
* Hypothalamo-hypophyso-surrenalian axe
- Glucocorticoids= hyperglycemia, catabolism of protein, depression immune system
Induction and maintenance dose of sevoflurane?
Speed of induction, recovery and depth during maintenance?
Induction: 5%
Maintenance: 2-3%
* Faster induction and recovery and changes in depth during maintenance than with halothane and isoflurane
What are the physiological effecst of opioids?
* CNS depression (or excitement in horses and cats)
* CVS: minimal effects, possible sinus bradycardia (vagal centre)
* Respiratory system (depression, drug and dose-dependent)
* histamine release (pethidine and morphine)
* GIT depression
* Release of ADH (urine retention)
* Hypothermia (sometimes hyperthermia in cats, horses, swine)
* Emesis (CTZ)
* Pupillary diameter (miosis in dogs; midriasis in cats)
What is Preferred Body Temperature (PBT)?
* the temperature at which metabolism is optimal
What would a vaginoscopy show in pro-oestrus? Oestrus? Dioestrus?
* pro-oestrus: pink, swollen, rounded folds, moist
* oestrus: pale-pink, shrunken/angular (crenulated), dry
* dioestrus: hyperaemic areas, rounded folds
What is the rate at which equilibrium is reach determined by?
* anaesthetic concentration gradient
* solubility in blood and tissues
* changes in alveolar ventilation
* changes in alveolar blood flow
* changes in matching between alveolar ventilation and blood flow
Drugs for a seizure in a dog?
* Diazepam
* Midazolam
* Levetiracetum
What does chemosensitivity (sensitivity of the tumours are to chemo drugs) depend on?
* Drug uptake into cell
* Interaction with cellular target
* Generation of lethal damage to cell
* Repair and response to that damage
What is a flail chest?
Ribs are broken, tries to breathe in = ribs collapse
What does vaginal cytology reflect? What is it not useful for?
* Vaginal cytology reflects endogenous oestrogen levels
* Excellent to determine dioestrus (D1)
* Good to determine proestrus or anoestrus
* NOT useful to determine ovulation or ideal time of breeding
MCV? MCH? MCHC? RDW?
MCV (PCV/RCC)- Mean corpuscular (red cell) volume– measures the volume of all the red cells going through and avgs it
MCH (Hb/RCC)- mean corpuscular haemoglobin (how much Hb does each red cell have)
MCHC (Hb/(RCC x MCV))= mean corpuscular hemoglobin concentration (** MORE SPECIFIC MEASURE)
RDW- red cell distribution width (measure of anisocytosis)
NRBC- nucleated red blood cells
Primary vs. delayed haemorrhage
* primary- inevitable but this can be reduced by good surgical technique and preemptive haemostasis
* delayed haemorrhage can be due to inadequate primary haemostasis (often masked anaesthesia induced hypotension) or failure of haemostasis (e.g. slipped ligature or necrosis of ligated/ coagulated vessels)
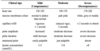
What are the commonly used classes and drugs in those classes in vet medicine?
* Phenothiazine: Acepromazine
* Alpha-2 adrenoceptor agonists: Xylazine, (dex)medetomidine, romifidine, detomidine
* Benzodiazepine: Diazepam, midazolam

Miller’s knot- type of simple (circumferential) ligature that is particularly useful for ligating a vascular pedicle– binds itself as it tightens
Who requires more drug– smaller or larger patient on a mg/kg basis?
* Smaller patients (surface area to volume ratio)
All bodily fluids are potentially infectious and direct skin contact should be avoided.
True
What is a multidimensional pain scale?
* composite of a number of SDS– relating to particular aspects of behaviour associated with pain (pictorial… behaviour/demeanor)
* May also have a physiological component
When might you use the metatarsal artery?
Femoral/pelvic fractures
Fractious animals
obesity, heavy muscling, jack russels
What are the sites of action of anaesthesia– and what do they cause?
* Supraspinal
- loss of consciousness
- amnesia
- analgesia
- attenuation of autonomic responses
* Spinal
- muscle relaxation
- analgesia
- attenuation of autonomic responses
What is haematocrit vs. Packed Cell volume
* Haematocrit= RBC count x RBC volume- calculated in the analyzer
* Packed Cell Volume- spin the tube down and measure how much red cells make up the total volume of plasma
What are the side effects of Xylazine?
* Sensitizes the myocardium to catecholamine
* emesis (more frequent than romifidine or medetomidine)
Side effects of isoflurane? How do they go with muscle relaxation? Analgesia?
* Neuro: decreases cerebral metabolic consumption, dialtes cerebral vasculature, can increase ICP
* Resp: decreases minute volume, increase PaCO2, airway irritant (coughing and laryngospasm), effective bronchodilator, apnoea occurs when anaesthetic depth is excessive
* CV: decreased CO, reflex increase in HR, decrease in cardiac contractility and SV, decreased BP, large decrease in vascular resistance, profound hypotension when anaesthetic depth is excessive
* Good muscle relaxation
* No significant analgesia
How do you safely correct hypotonic fluid loss (hypertonic dehydration)?
*DO NOT drop Na+ by > 0.5-1 mmol/hr or > 12 mmol/24 hours
What else other than enzymes do you look at to assess hepatic function?
* Urea synthesis, cholesterol synthesis, albumin synthesis, glucose synthesis, bilirubin conjugation, bile acids uptake and excretion, ammonia uptake and metabolism
Why perioperative analgesia?
* Multimodal, limit development of peripheral sensitisation and central sensitisation, block neuroendocrine response, reduce major complications, improves outcome

What are the main gram positive cocci and rods of veterinary importance?

When monitoring a horse under anaesthesia, what are you looking for regarding the nervous system? Respiratory system? CV system?

What dictates the surgical dose? Or prognosis?
Tumour type, grade and stage
Why is Alfaxalone especially good?
* high therapeutic index
* lack of cumulation in the body (ideal for CRI)
* rapid, complete recovery of consciousness
* lack of irritant effects and activity when given peri-venously (IM/ SC)
What is conjugated vs. unconjugated bilirubin?
Conjugated means it has been processed through the liver. Unconjugated is the form straight from haemoglobin
** not terribly helpful, but it can help if elevated bilirubin and almost entirely unconjugated that’s when you think pre-hepatic… by the time we diagnose, it is usually a mix of the two
What are the clinical uses of benzodiazepines?
* Excellent agents for sedation in the “poor risk” patient, alone or with opioid drugs BUT unreliable in “healthy adult” patients
* increase muscle relaxation during anaesthesia
* offset muscle hypertonicity caused by ketamine
* stimulate appetite in anorexic patients
* treatment of seizures
* decrease dose of induction agent
What is a simple descriptive scale for pain?
* Describes intensity of pain
* No pain, mild, moderate, severe
* Not very sensitive
What are the signs of Stage IV of anaesthesia?
* Signs of severe shock
* Weak pulse, not breathing
* Dilated pupils
* Reflexes are absent
* lost control of sphincter tones
Physiological considerations of small ruminants
* secretions of large volumes of saliva e.g. 50 L of saliva in 24 hours…. consequence: potential airway obstruction or aspiration
* Regurgitation- possible aspiration of ruminal contents
* positioning: compression of the diaphragm– lateral or dorsal recumbency… consequences: decrease in ventilation, increase ventilation- perfusion mismatch, hypoxaemia and hypercapnia
* Compression of the major abdominal vessels: dorsal recumbency, abdominal viscera, decrease venous return, decrease CO, decrease BP
* Tympany: due to impaired eructation– gas produced through continuous fermentation of ingesta accumulates in the rumen– caused by lateral or dorsal recumbency, heavy sedation and anaesthesia.. consequences: respiratory distress, decreased CV function
What are the effects/ side effects of Ketamine (IV anaesthetic)?
* dissociative anaesthesia
* amnesia/ hallucinations in recovery
* analgesia (somatic > visceral)
* immobility
* GABA and NMDA receptors
* increased ICP
* may cause seizures
* CV: direct negative inotropic effect in vitro, increased sympathetic tone in vivo, increased HR, contractility, CO, and arterial BP, increased myocardial oxygen demands
* Resp: apnoea, bronchodilation, apneustic breathing
* increased muscle tone
* Pain on injection
What are Metronidazoles?
* Anaerobic infections
* Particularly mouths, osteomyelitis, peritonitis
* Can use as a flush
* Flagyl- often use human brands
What retractors can be bent repeatedly especially useful in abdominal and thoracic operations?
Ribbon malleable retractors
Safe handling of chemotherapeutic drugs
* Rigorous training
* Full PPE- mask, gowns, hood
* Closed system- minimum aerosolization when administered
How long should you fast monogastric, ruminants, and small mammals, birds and neonates before surgery? Withhold water?

When receiving a histopathology report regarding a mass removed, what 3 pieces of information will you receive in return?
- Diagnosis- cell of origin
- Grade (invasion, Mitotic Index (MI))
- Assessment of adequacy of margins
What is the effect on the ECF in hypotonic fluid loss?
Hypertonic ECF
* Hypertonic dehydration
What is a partition coefficient?
Measures of solubility in blood and tissues at a given temperature (37C)
* The ratio of inhalation anaesthetic concentration in two compartments or tissues (blood:gas)
What are the pharmacokinetics of intravenous administration of a drug?
* plasma concentration decreases rapidly as a result of both distribution out of the vascular space and elimination
* Recovery depends upon distribution and elimination of half lives
What are the contraindications for opioids?
* Pre-existing respiratory depression
* head trauma
* pancreatitis
Steroidal anti-inflammatory drugs used in horses
* Prednisolone, Dexamethasone
* Reduces inflammation
* Significant systemic side effects: delayed wound healing, abortion in the last trimester, laminitis
* Long duration of action (12-24 hours)
Four Common Features of the Diagnostic Process
* Signalment: patient, wider system (e.g. farm)
* History: disease distribution? time & space; are there associations with events, places, things that suggest RISK FACTORS
* Clinical exam of: Animal (are there other cases? Environment; Management (e.g. examin records)
* Further tests and special examinations: rule ddx in or out (during process or to finalize it); use response to treatment
What is the ideal heating of a reptile’s environment?
* temperatures similar to field conditions with temperature variation allowing the animal to choose its thermal environment (thermoregulate)
What is balanced anaesthesia?
* A collection of component changes in behavior and perception
* Components of the anaesthetic state including loss of consciousness, amnesia, analgesia, muscle relaxation, and attenuation of autonomic responses
What are some fluids that are alkalinizing? When would you give them?
* LRS, Normosol- R, Plasmalyte-148 (all are balanced isotonic)
* all contain buffers (lactate, acetate, gluconate) and have lower chloride concentrations
* ideal initial fluid therapy while test results pending as the vast majority of illnesses result in metabolic acidosis e.g. uremic acidosis, ketoacidosis, lactic acidosis
Topical haemostatic agents?
Stypics e.g. silver nitrate (only use on nails as causes pain and burns tissue), potassium permanganate
* Porcine gelatin sponges– swells and causes tamponade
* Oxidized regenerated cellulose- forms gelatinous clot on contact with blood, creating mechanical tamponade and barrier to bleeding, bactericidal, absorbed over 2-6 weeks
* Bone wax- sterile beeswax with softening agents, creates mechanical barrier to bleeding (difficult to adhere to bleeding bone), often used in spinal surgery… inhibits bone healing– do not use on fractures or sternotomies
* Bovine collagen- mechanical tamponade plus enhances platelet aggregation
* Polysaccharide spheres- swelling provides tamponade/ mechanical barrier
*
What is pattern recognition?
I know what that is and exactly what causes it
With an icteric patient, what questions do you ask?
Is it pre-hepatic, hepatic, or post-hepatic?

What would you find generally in uncomplication hypovolaemia?
If doing AI, where do you deposit frozen semen?
Uterus
What can imitate renal failure?
* Medullary hypotonicity or impaired ADH action can mimic renal failure
- Hypochloridemia due to upper GIT obstruction
- HypoA
- HyperA
What is meant by prudent use of antimicrobials?
* Treatment- known infection
* Prophylaxis- not currently ill with a particular disease, but at high risk of acquiring an infection
* Metaphylaxis- mass medication of a group of animals, in advance of an expected outbreak of disease
Minimise resistance by:
* appropriate antibiotic choice
* Appropriate antibiotic use
* Minimizing use
How long do you withhold food and water for horses?
* Food at least 8 hours
* Water for at least 2 hours
When is chemotherapy generally used?
* Lymphoma
* Mast cell tumours
* Multiple myeloma
* Nasal tumours
* Transitional cell carcinoma (bladder/urethra)
* Haemangiosarcoma
* Osteosarcoma
* Other solid tumours as adjunctive therapy
What are the four different groups of penicillins?

How would you split up the fluids for rehydration therapy? What are some factors that might cause you to consider administering more slowly?
If relatively acute in onset, can replace first half of deficit over 6-8 hours and remainder over 16-18 hours.
* if relatively chronic (days) or acute can also replace at a consistent rate over 24 hours (or more if necessary)
* cardiac dysfunction, oliguric/anuric renal failure, other forms of fluid intolerance e.g. vascular leak
Normal respiration SA?
* Normal RR= 15-25 bpm
* Normal respiratory pattern:
- diaphragmatic contraction 70-80% of a resting inspiration
- diaphragmatic contraction results in passive abdominal movement
- on inspiration chest and abdomen move out together
What are Sulphonamides?

Side effects of sevoflurane? Muscle relaxation? Analgesia?
* Neuro: decreases cerebral vasculature, can increase ICP
* Resp: decreases minute volume (ventilation), increase in PaCO2, effective bronchodilator, apnoea occurs when depth is excessive
* CV: decreases CO, decrease in myocardial contractility and SV, CO is lower than iso, decrease in BP mainly due to decrease in CO, BP is higher than iso
* Good muscle relaxation
* no significant analgesic
What are proto-oncogenes? What are tumour suppressor genes?
* Proto-oncogenes: Tumour cell growth is mediated by proto-oncogenes that can arise spontaneously or during the development of the tumour. Effects that increase growth of cells to avoid apoptosis. May alter the function of cells that develop during cancer.
* Tumour suppressor genes: Proto-oncogenes counter acted by tumour suppressor genes that discourage growth– so there is a balance.
What percentage of tensile strength do wound attain?
70-80% of normal tissue
Is it most likely a stress leukogram, inflammatory leukogram, or an excitement leukogram?

An inflammatory leukogram (no left shift, but toxic change)
How do you choose an antibiotic?
* legally prescribing and dispensing an appropriate active ingredient that gets to the site of infection at levels above the MIC for an appropriate period, taking into account:
* prudent use of antibiotics
* cost
* Compliance
* Drug interactions
What role does surgery play in the treatment and management of cancer?
* Diagnosis: biopsy
* Tumour staging- LN, distant organ biopsy
* Curative surgery- local tumour control
* Palliation- advanced diseaes for quality of life (splenectomy for haemangiosarcoma, life expectancy is 3 months… amputation for pathological fracture)
* Prevention- OHE to prevent mammary cancer
* Cytoreduction as part of multimodal therapy- radiation/ chemotherapy/immunotherapy
Sedatives used in horses? Characteristics of each?
* Acepromazine: sedation, no muscle relaxation or analgesia, significant CV side- effects: vasodilation and hypotension, use with caution in stressed or hypovolemic horses, long duration of action: half-life: 3 hr
* Diazepam: reliable sedation in foals, unreliable sedation in adults, excellent muscle relaxation, no analgesia, few CV side effects, poor IM absorption, long duration of action half-life 9.7 hours
What is dose intensity (chemotherapeutic drugs)?
* Amount of drug per unit time
* Can be increased by increasing dosage at particular administration
* Can be increased by shortening time interval
* Optomising dose intensity improves outcome
Types of pain
* Physiological pain (or adaptive pain)- warning for potentially harmful stimulus, localized and transient
* Pathological pain- tissue damage has occurred, ongoing pain… acute (pancreatitis) or chronic (inflammation of a joint)
What does vaginal cytology look like in a bitch in oestrus?
* > 90% cornified cells marks beginning of “cytological oestrus”; superficial and anuclear squamous cells (anuclear, largest vaginal epithelial cells, resemble “cornflakes”)
* bacteria can be present
* BUT no neutrophils should be present

Analgesics used in horses
* Butorphanol: kappa agonist, mu antagonist, analgesia (visceral), no sedation or muscle relaxation, CV side effects, limited effect on GI motility and transit time, short duration of action (1-2 hours)
* morphine: mu, kappa, delta agonist, analgesia (somatic), no sedation or muscle relaxation, significant behavioral and CV side effects at higher doses, effect on GI motility and transit time, short duration of action (2-4 hours)
Is movement always a sign of light anaesthesia in a sheep?
No
Local anaesthesia for castration– anatomical nerves? Nerves that you perform block on and dose?
(Anatomy: testicles L3 and L4; scrotum S2, S3, S4, S5)
* Intratesticular: Lidocaine 2-4 mL/100 kg/site
* Spermatic cord: Lidocaine 1-2 mL/100 kg/ site
* Scrotum: Lidocaine 1-2 mL/100 kg


Why are platelet counts often inaccurate from the analyzer? What can lipaemia cause a false reading of?
* Platelet clumping can show low on the analyzer
* Lipaemia- can falsely inscrease total solids, Hb, MCH, and MCHC
What is ligation? What are the two types?
* use of suture material and surgical knots to occlude blood vessels– vascular strangulation
* Simple (circumferential)- after applying haemostat, elevate it away from the tissue to place ligature around clamped vessel– strangulation used with a simple knot and safety against slippage is ensured by the double knot
* Transfixation- usually used on pedicles, sometimes in combination with simple (circumferential) ligatures
In an exploratory laparotomy what will you find in the caudal right quadrant?
* Bladder and ureters
* Prostate or uterus/ ovaries
* Open omental bursa to visualize L limb pancreas
What is the “worst drug rule” in chemotherapy?
* Use the least potent/ effective drug first
* If you use the best drugs first and there are cells resistant to that drug then you only have the worst drug to use against those tough cells
Where alpha-2 analgesics & anxiolysis?

What is the problem with povidone iodine? What other solutions is this not the case?
Inactivated by organic material
* Chlorhexidine gluconate- works in the presence of organic materials & alcohol works but reduced efficacy in the presence of organic materials
How is Thiopental metabolized?
* Induction and arousal from anesthesia depends largely on redistribution not from metabolism
* hepatic metabolism 5% total dose is metabolised per hour
What are the different classes in an anaesthetic risk assessment?

What are the two negatives about multifilament?
Greater tissue drag, increased tendency for bacterial colonization due to interstices between strands– should be avoided in contaminated environments
How can you monitor cardiovascular function clinically?
* HR from ECG (normal QRS complexes, Is there a P wave in front of every QRS?, Is there a QRS after every P wave?), pulse oximeter, stethoscope
* BP related to CO and to vasomotor tone


What kind of virus is Hendra virus?
Hendra virus is an enveloped RNA virus that is classed as a Category A and is sensitive to soaps/detergents and many disinfectants

Liver function is okay… we know there is liver damage though, so it has to be hepatic.

Mayo-hegar needle holder
What is the most widely used hand scrub? How does it work? What is the solution?
4% Chlorhexidine Gluconate
* Broad spectrum gram positive, lesser extent gram negative
* Not sporicidal, some viruses
* acts by altering the bacterial cell wall and precipitates intracellular contents
* Immediate action with ongoing residual action by binding to keratin
* Active in the presence of organic matter
What happens with hypertonic fluid loss? What are some of the possible causes? CNS effects?
* solute is lost in excess of water
* results in hypotonicity of the ECF (hypotonic dehydration)
* hyponatremia, hypoosmolality** neurons do not like to be swollen so they pump out molecules
* e.g. severe burn injury, hyperadrenocorticism, iatrogenic
* CNS effects: chronic hyponatraemia–> decrease in neuron idiogenic osmoles to match ECF tonicity
- rapid correction of ECF hypoosmolality–> neuron shrinkage!! Causes demyelination known as central pontine myelinolysis or osmotic demyelination syndrome
What happens with isotonic fluid loss? What are some examples where isotonic fluid loss can occur?
Similar loss of solute and water
* No change in ECF osmolality and no fluid shifting
* Na+ and osmolality remain within normal limits
e.g. haemorrhage, vomiting, diarrhoea
What are the 6 common antibiotics used in large animal medicine?
- Penicillins
- Cephalosporins
- Macrolides
- Aminoglycosides
- Tetracyclines
- Sulfonamides
What does the circuit volume and oxygen flow rate do?
* control the speed at which the anaesthetic concentration can be changed
What is sepsis, asepsis, antisepsis, antiseptic?
* sepsis: presence of pathogens (or their toxins) in tissues
* aspepsis: the absence of microorganisms in living tissue
* antisepsis: prevention of sepsis by the destruction or inhibition of microorganisms
* antiseptic: a chemical agent that either kills pathogenic microorganisms or inhibits their growth
What falls under the non-critical category in the Spaulding’s risk classification system of surgical related items? Examples? What level of “clean?”
* contact with intact skin
* exam tables, BP cuffs
* clean as necessary with detergent and water
What are doses of chemotherapeutic drugs calculated based on?
* Body surface area
* Metabolic basis, presuming smaller animals have faster excretion etc.
What are the 3 key steps to patient skin preparation?
* bathe the patient pre-op with 4% chlorhexidine scrub solution
- Pre-wash- 0.5 % chlorhexidine gluconate
- Removal of detergent- 70% alcohol spray
- Application of an approved surgical skin antiseptic product- 0.5% chlorhexidine tincture (CHG) spray OR providone iodine and alcohol
Why does haemorrhage need to be controlled?
* Severe haemorrhage leads to hypotensive shock
* Bleeding obscures the operative field
* Blood within the operative field irritates tissue, prevents tissue apposition, delays healing and potentiates infection
* Blood on instruments, drapes and tissues is an ideal medium for bacterial
What is the key abnormality method?
Identify the main problem
- identify body system associated with signs
- identify lesion in the body system
- identify aetiology/agent likely to cause lesion
What is the problem with too small of a staple? Too large?
* too small staple- won’t incorporate all layers and may cause ischaemia to wound edges
* too large they may not achieve adequate tissue apposition or haemostasis
What is the difference between epidural anaesthesia and epidural analgesia?
Epidural Anaesthesia:
(Anatomy: Spinal cord ends below S1 or S2, epidural space, subarachnoid space)
* Intercoccygeal epidural (C1-C2): Lidocaine: 1 mL/100 kg
*Complications severe ataxia and excitement if pelvic plexus nerve roots blocked (L5- S2)
Epidural Analgesia:
(Anatomy: spinal cord ends below S1 or S2, epidural space, subarachnoid space)
* Intercoccygeal epidural (C1-C2)
* Strict aseptic technique
* Morphine: 0.1 mg/kg diluted in saline (4-6 mL/100 kg)
Chemotherapy principles (3 main)?
* Treatment should begin when tumour cell population is smallest
* Multi-drug protocols minimize likelihood of resistance
* Drugs should be administered at the maximum tolerated dose
General Anaesthetics used in horses
* Ketamine: NMDA receptor antagonist, dissociative anaesthetic, analgesia at subanaesthetic doses, poor muscle relaxation, limited CV side effects, very short duration of action (20 minutes)
What do you HAVE to look at when interpreting Calcium and phosphate?
Look at albumin when interpreting Calcium. Most of total calcium is albumin bound.
* Think about the balance- absorbed from the GIT, deposited in bone or resorption depending on need, renal excretion, leakage from cells (phosphate)
* Consider hormones PTH, vitamine D, PTHrP
What diagnostic tests might you run prior to anaesthesia?
* CBC: anaemia, inflamm
* Biochem: colloid oncotic pressure (albumin), hepatic function (SDH, GGT, bile acids), renal function (BUN, creatinine), Muscle enzyme abnormalities (CK, AST), Electrolyte abnormalities (Na, K, Ca, Cl), Tissue perfusion (Lactate)
* Urinalysis (renal function- specific gravity)
* Diagnostic imaging
Preferred sutures of the fascia?
Synthetic, monofilament, non-absorbable or synthetic absorbable (long acting)

Yankauer suction- large volumes from abdominal cavity or thorax– not fine dissection
Frazier Ferguson- can place index finger over hole and varies the suction
Poole- multiple opening at its tip which reduces plugging problems encountered with omentum and removal of fluid from abdominal cavity (disposable available)

What suture gauge for dog > 20 kg? Small dog/ cat?
Dog > 20 kg= ‘0’ suture gauge
Small dog/ cat- 3/0–> 2/0
What do you assess with the respiratory system?
* Respiratory rate
* Respiratory effort
* Auscultation
What is palliative treatment for round cell tumours? Carcinoma/sarcomas?
* Round cell tumours: Prednisolone
* Carcinoma/sarcoma: Piroxicam or meloxicam
Preferred sedation protocol in small ruminants?
Sedation and muscle relaxant:
* Diazepam or midazolam
Analgesia:
* Butorphanol
* Buprenorphine (longer duration of action)
What materials are staples made from?
Stainless steel, titanium (reduced CT/MRI artifact), absorbable
Metabolism of NO? Consequences of prolonged exposure?
100% eliminated unchanged by the lungs
* Vitamin B12 deficiency with prolonged exposure (megaloblastic anaemia, polyneuropathy)
What are the medications that can reduce anxiety or high arousal levels in dogs? Noise phobias?
* Selective Serotonin Reuptake Inhibitors (SSRI)
* Tricyclic Anti-Depressants (TCAs)
* Clomipramine
* Tazodone (SARI- Serotonin 2 A Antagonist Re-uptake Inhibitor)
* Beta blockers- propranolol- blocks adrenergic activity– useful in combination with an SSRI or TCA
* Noise phobias: Benzodiazepines or Trazodone (SARI)- best used prior to the noise event
Why does cachexia often go with cancer? What does this mean for prognosis?
* Weight loss despite adequate nutritional intake because glucose is the main substrate for tumours (tumours can’t use lipids)
- high energy conversion to lactate and back
- protein (muscle mass) broken down to supply amino acids
** Poor prognostic indicator
Normal heart rate in dogs and cats? Arrhythmia? Hypovolaemia?
* Dogs 80-120 bpm
* Cats 160- 220 bpm
* > 220- 240 is usually an arrhythmia
* Heart sounds are quiet with hypovolaemia
What does the anaesthetic vaporizer do?
* Controls the maximum anaesthetic concentration that can be reached
Why combine tranquilizer/sedative agent with opioids for premedication?
* Synergistic effects
* Produces reliable “safe” sedation
* Reduces dose of induction and maintenance agent
* Pre-emptive analgesia
What are some red flags with fluid therapy?
* heart disease, pulmonary disease, sodium derangements, hypoalbuminaemia, severe anemia, oligoanuric renal failure, TBI, vascular permeability, underlying disease (Addison’s, DKA, FUO)
Where do you give local anaesthesia for dehorning goats?
* Cornual branches of the zygomaticotemporal and infratrochlear nerve in goats
* GA may be preferred in young animals to avoid toxicity and in adults with large horns

What are the three questions to ask when assessing anaemia?
- Regenerative or non-regenerative?
- loss (haemorrhage, haemolysis)
- decreased production - Is the protein level low, normal or high?
- Are there clues on the blood film?
How is Propofol metabolized?
* hepatic metabolism and redistribution
* extra-hepative metabolism– lung, kidney, blood??
* slower in cats than in dogs (phenol compound)
Indications for laparotomy?
* GI disorders- FBs, torsion, rupture
* Urogenital abnormalities unresponsive to medical treatment
* Abdominal disorders of unknown origin
* Penetrating trauma
* Acute abdomen
* Generalized peritonitis
* Diagnosis and treatment of portosystemic shunts
* Splenic abnormalities
* Uncontrolled abdominal haemorrhage
Cause of central sensitisation?
* Indirect consequence of tissue trauma and inflammation
* constant activation of peripheral receptor
- Glutamate, asparate, substance P are released (constant activation of AMPA and neuropeptide receptors on dorsal horn; increased response to both nociceptive (hyperalgesia) and non-nociceptive (allodynia) stimuli)
What is the blood:gas partition coefficient for Isoflurane and Sevoflurane?
* Isoflurane: 1.4 @ 37C
* Sevoflurane: 0.7 @ 37C
How is Ketamine metabolized?
* Hepatic metabolism in dogs and horses
* Mainly excreted unchanged via the kidney in cats
* rapid recovery in most species due to redistribution from CNS to body tissues
What happens when inhalation anaesthetic agents are more soluble in blood and tissues? Example?
* Halothane
* Induction of anaesthesia is slower
* Changes in depth are slower during maintenance of anaesthesia (less control of depth)
* Recovery of anaesthesia is slower
What are the precautions to take with Thiopental?
* IV only (skin slough- treatment saline and lidocaine), thin dogs, hypovolaemia, liver dysfunction, age, obesity, hypoproteinaemia-acidosis
What are the different depths of anaesthesia by MAC?
- 0 MAC = light surgical plane
- 5 MAC = moderate surgical plane
2 MAC = deep surgical plane
3 MAC = mostly dead
What are some indications for laparoscopy?
* Abdominal cryptorchid testes
* Ovariectomy/ ovariohysterectomy
* Liver biopsy
* Lap- assisted gastropexy
* Lap- assisted cystotomy
What are the maintenance vaporizer setting for Isoflurane and Sevoflurane for cats, dogs, and horses?
* Isoflurane:
- Cat 1.6%
- Dog 1.4%
- Horse 1.4 %
* Sevoflurane
- Cat 2.6%
- Dog 2.3%
- Horse 2.3%
What are surgical oncology principles?
* the first surgery is the best chance to effect a local cure
* Excise biopsy tracts
* Early vascular (venous) ligation to reduce tumour embolic spread
* Gentle tissue handling to reduce tumour embolic spread & to reduce seeding into the wound bed, thoracic or abdominal cavities
* Lavage excision bed
* Change gloves and close wound with separate set of instruments
* Submit all resected tissue for histopathology (NOT a choice, if it is worth removing, it is worth submitting)
* Ink margins
* Submit as whole specimen
Isoflurane induction and maintenance doses? How does speed of induction, recovery, and depth during maintenance compare to halothane?
* Induction: 3%
* Maintenance: 1-2%
* Faster induction, recovery, changes in depth during maintenance
What are the other related surgical instruments?

Kern and Lane bone-holding forceps– available with or without ratchets
* Lowman bone clamp- long bone use
* Richards bone-holding forceps- tubular bones
* Verbrugge bone clamp- rapid fixation of fragments (large dogs)
* Reduction forceps with speed lock- hold fragments in place rapidly, with point maintain fracture fragments in reduction during fixation
Where would you perform a paravertebral block in a small ruminant? What gauge, length needle? Standard dose for T13? How far away from dorsal midline?
next to T13, L1 and L2
* 23 gauge, 8.9 cm spinal needle
* Inserted 2.5-3 cm lateral to the dorsal midline
* 2 mL for ventral branch, 1 mL for dorsal branch

What is the shelf life of sterile packs?
* event related not time related
* published guidelines: 96 weeks for plastic/ paper wrapped items post steam sterilisation
What are the advantages and disadvantages of staples?
Advantages: reduced surgical time, ease of application, if used correctly, integrity/security of closure is equivalent to hand sutured
Disadvantages: cost
What does HEAPPC stand for?
History and Examination
Assessment, Problem List (each problem has ddx)
Plan (each problem has a plan)
Communication
What are Halsted’s Principles?
* Observe strict aseptic technique
* Thorough knowledge of anatomy and technique
* Control haemorrhage meticulously
* Gentle tissue handling- every damaged cell places additional demands on the body’s recovery mechanisms; appropriate location of incisions and adequate incision length
* Preserve blood supply to tissues
* Accurate tissue apposition with minimal tension
* Eliminate dead space
What will vaginal cytology in a bitch in anoestrus look like?
* Non-cornified cells
- mainly small, round parabasal cells and intermediate cells (larger than parabasal cells, higher cytoplasm: nuclear ratio)
* Neutrophils can be present
* Bacteria can be present

Muscle enzymes?
CK and AST
* CK more specific
* AST is from red cells and liver
* But look at both
(ALT and LDH)
* We see myoglobinuria in the urine if there is muscle damage
What are important things to know about using Propofol as an IV anaesthetic? And side effects?
* emulsion lipid based (white)
* support bacterial growth and must be discared within 6 hours after opening
* do not keep in fridge
* CV depression
* resp depression
* pain on injection
Causes of prerenal azotaemia
* Dehydration–> concentrated urine
- often greater increase in Urea than Creatinine
- other clinical evidence
* GIT protein absorption or bleeding
- incrased urea only unless concurrent dehydration
What are the ABCs?
* Airway: is there a patient airway?
* Breathing: is the animal making useful breathing efforts?
* Circulation: is there a heart beat with pulses?
To avoid inhalation of zoonotic agents such as Hendra virus, what mask is recommended for field work?
P2 (N95) respirator mask
What is radiation therapy? What is the dose of radiation therapy used in cancer treatment limited by?
* The use of ionising radiation to cause cell death via application of energy to DNA– proliferating cells are radiation sensitive (neoplasms and renewing cell populations)
* surrounding normal structures e.g. skin, eyes, brain, GIT, bone, lungs
Lipids- cholesterol and triglycerides, levels depend on?
* Intake (post prandial increase)
* GIT absorption (pancreatic function)
* Hepatic synthesis (corticosteroids, insulin, thyroid hormone, lipase)– if you have a bile blockage, you often have an increase in cholesterol
* Tissue metabolism (corticosteroids, insulin, thyroid hormone, lipase)
* Loss (lymphangiectasia- pathological inflammation of lymph vessels esp in the small intestines, can be congenital, secondary can be caused by granulomas, cancer, or increased central venous pressure causing abnormal lymph drainage secondary to pericarditis or right sided heart failure)
What are Macrolides used for? Different sorts?
Gram positive drugs used for respiratory, mastitis and prostates and as in-feed medication in large animals
* Erythromycin, Tylosin, Tulathromycin, Oleandomycin
* Some topical forms in small animals - especially ears (e.g. Tilmycosin)
What are the different categories and the drugs that fall under those categories of opioids?
* Full (pure mu) agonists: morphine, methadone, meperidine, hydromorphone, fentanyl, alfentanil, remifentanil
* Partial mu agonists: buprenorphine
* Kappa agonist- mu antagonists: butorphanol, nalbuphine
Why multi-modal (balanced) analgesia?
* Pain pathways are long and complicated and different drug classes act at different sites
* Multi-modal approach improves efficacy and reduces side effects
Time of breeding fresh/chilled? Frozen?


hand-held Meyerding retractor - retracting large muscle during long bone or pelvic fracture repair
What are the three types of fluid therapy?
- Acute resuscitative– correction of intravascular deficit. Rapid IV fluid therapy targeting restoration to perfusion. e.g. 15 ml/kg over 15 minutes
- Rehydration therapy– correction of interstitial or intracellular deficit– gradual restoration over 24 hours, for example (intracellular hydration care re: cerebral oedema)
- Maintenance requirements- volume of fluid needed to maintain zero fluid balance– considers sensible and insensible (evaporative- cutaneous, respiratory, faeces, saliva) + ongoing losses

Gelpi pernineal retractor


Sedative Analgesics in horses
* Xylazine: alpha 2 agonist, sedation, analgesia, muscle relaxation, significant CV side effects: peripheral phase: initial increase in BP reflex decrease in HR, central phase: decrease in BP and HR, Decreased GI motility, short duration of action (30 minutes)
* Romifidine: alpha 2 agonist, sedation, analgesia, muscle relaxation, CV effects, decreased GI motility, long duration of action (60 minute)
* Detomidine: alpha 2 agonist, sedation, analgesia, muscle relaxation, CV effects, decreased GI motility, long duration of action (60 minutes)
*Medetomidine: alpha 2 agonist, sedation, analgesia, muscle relaxation, CV side effects, decreased GI motility, short duration of action (30 minutes)

How do you calculate how much for rehydration therapy?
Deficit (ml) = Estimated deficit (%) x body weight (kg) x 1000 ml/ 1 L
e.g. 10 kg dog, 5% deficit: 0.5 x 10 x 1000= 500 ml
What is a transfixing ligature?
* Used for large blood vessels or vascular pedicles when increased security is required e.g. closed castration, vessels in amputation
* Typically placed after and distal to a simple ligature


Campylobacter foetal liver


Which sedative has caused pulmonary oedema and fatalities in sheep?
Xylazine
If ewes are old enough, right season, and no toxins… what is the largest factor on fertility?
Condition score aim for 3 at mating and lambing
** Short-term increased protein intake pre-mating
For Merinos: Extra 1 CS (7-10 kg bodyweight)= extra 10-20% lambs born

Gosset- ideal for smaller patients

What size margin should you give a mass with a high likelihood of local recurrence?
2-3 cm lateral margins (5 cm for high grade soft tissue sarcoma (STS)) OR one fascial plane deeper than compartment of origin
What is the concentration of Isoflurane and Sevoflurane in the vaporizing chamber?
* Isoflurane: (240 mmHg/ 760 mmHg) * 100 = 32%
* Sevoflurane (160 mmHg/ 760 mmHg)* 100 = 21%
Why is endotracheal intubation necessary during anaesthesia?
During anaesthesia deglutination reflexes are lost and endotracheal intubation is necessary to secure the airway. It also allows for the delivery of inhalant anaesthesia and mechanical ventilation.
What are cathartics? Examples?
* Speed up GIT emptying
* Useful for solid poisons
* Examples: Sorbitol, Epson Salts (MgSO4), Paraffin Oil
What signs do we look for to assess pain in an animal?
* Demeanour, posture, vocalisation, attention to wound, mobility, interaction with people, response to handling
* HR RR and pupil dilation
What are the intravenous anaesthetic agents?
* Barbiturates (thiopental, pentobarbital, phenobarbital)
* Dissociative agents (ketamine)
* Imidazole derivative (etomidate)
* Steroids (alfaxalone)
* Phenol derivatives (propofol)
What do anaesthetic agents do to bleeding?
Cause hypotension and hypothermia which both reduce/mast the amount of bleeding
How is halothane metabolized?
* 80% eliminated unchanged by lungs
* 20% metabolized by liver and eliminated in urine
What causes peripheral sensitisation? Purpose?
* Tissue trauma (inflammatory mediators from damaged cells- H+, K+, PG, plasma (bradykinin), plateletes (serotonin), mast cells (histamine), macrophages (cytokines))
* Inflammation- sensitising soup of chemical mediators
* Purpose: promote healing by enhancing perception of pain, protect against future damage

What are essential parts of cancer diagnosis?
* Examination of draining lymph nodes– palpation/ FNA/biopsy
* Imaging +/- cytology/ biopsy of distant organs– lungs, abdominal organs, LN, liver
* Haematology, Biochem, Urinalysis– looking for othe organ involvement, incurrent disease and/or paraneoplastic syndromes
What are the kinds of non-absorbable sutures?
* Silk, polypropylene, Nylon, polyester

Dehydration


What is a capsule history?
* age, breed sex
* Primary complaint
* Duration of the problem
* Appetite, water intake and activity
* Vaccination status
* Any current medication
When does the most rapid gain of wound strength occur after injury? What happens by day 21?
* between days 7 and 14 after injury corresponding to the rapid accumulation of collagen in the wound. By 21 days, the collagen content is at its maximum– but wound strength is only about 20% of its final strength

History: Dyspnoea
* Less air in the lungs
* bacterial aspiration pneumonia
Test: broncho alveolar lavage
What are the 6 antibiotics used in small animal medicine?
- Penicillins (Amoxycillin, Betamox, Clavulox, Clavubactin S)
- Cephalosporins (Cephalexin, KefVet)
- Tetracyclines (Vibravet)
- Sulfonamides
- Fluoroquinolones (Tribrissen)
- Metronidazole


What is the ASA status?
1- a normal healthy patient to 6- A declared brain-dead patient whose organs are being removed for donor purposes
What are the main effects of Benzodiazepines?
* Muscle relaxation
* Anxiolytic
* Appetite stimulation
* Minimal CV and resp effects
* Anti-convulsant
* Potential for complete reversal (flumazenil)
* Anti-arrhythmic
What is cancer?
Group of cells that have continued to proliferate, lack ability to die… ignore the signals for apoptosis
When should you give analgesics?

When is mechanical ventilation indicated?
* GA
* Oxygenation failure: low PaO2 even with O2 therapy
* Ventilation failure: High CO2
* Post cardio-pulmonary resuscitation
What are the types of short/ midterm absorbable sutures?
Natural sutures e.g. catgut– enzymatic absorption
* Synthetic sutures– absorbed via hydrolysis (reaction with water)– more rapid in urine
* Glyconate (Monosyn)- 50% strength at 2-3 weeks, absorbed completely in 60-90 days
* Polyglycolic acid (Dexon)
* Polyglactin 910 (Vicryl)- braided
Initial approach to the small animal emergency patient
- ABCs: airway, breathing, circulation
- capsule history: important points from the owner
- major body system assessment
- prioritised problem list: What’s going to kill it first? stabilize most life threatening problem first
What does planning appropriate definitive therapy require knowledge of?
* Tumour type (what is it?)
* Tumour grade (how bad is it?)
* Tumour stage (Where is it?)
** Results of biopsy and clinical staging tests provide information on expected biological behaviour and therefore prognosis, which helps us select optimal treatment options
* Knowledge of tumour type, grade, and stage dictates “surgical dose”
First principles with poisonings?
* Stabilize vital signs
* history and evaluation
* stop ongoing absorption
* give antidote if available
* increase toxin clearance
* supportive care
What is monitored in the bone marrow mostly during chemotherapy? Why? When are CBCs conducted? What will do if severe neutropenia (<1.5) occurs?
Neutrophils- shortest of the lifespan (Red cells are not as impacted)
* Neutrophils can help us adjust dose– if too high a dose at risk of secondary infection
* Check full CBC 1 week after giving chemotherapy and before each treatment
** If severe neutropenia then drop the next dose by 25%, PO aerobic antibiotics, if severe neutropenia + pyrexia–> IV antibiotics… some oncologists recommend 10 days prophylactic antibiotics with each new chemotherapy regime/ drug
What is in the semi-critical category of risk according to Spaulding’s risk classification? Examples? What level of “clean?”
* contact with intact non-sterile mucosa or non-intact skin
* e.g. endoscopes, anaesthetic equipment
* sterilisation is preferable, otherwise high level disinfection required
Which drugs act peripherally and which act spinally? Supra spinally?
Supra-spinal
* Opioids
* Alpha 2 agonists
* Centrally acting NSAIDs
* Tramadol (weak opioid, serotoninergic, NMDA)
* Tricyclic Anti-depressants

What are the methods of haemostasis?
* Avoid bleeding by knowledge of relevant anatomy and careful dissection
* Digital pressure/ tamponade (allows clot to form 30 seconds for soft clot then 2-3 minutes for cross linking of fibrin– definitive haemostasis can be applied for 4 minutes)
* Haemostats
* Ligatures (best haemostatic security- simple or double)
* Vessel sealant devices
* Topical local haemostatic agents
How might you administer hypertonic or hypotonic fluids?
Central vessels
Why is providone-iodine not used stand alone? When is it contra-indicated?
* Low residual activity (unlike chlorhexidine)
* Inactivated by organic material
* contraindicated in neonates and is noted as having a high incidence of skin reaction
Why do anaesthetic agents reduce/ mask the amount of bleeding?
Cause hypotension and hypothermia
What type of instrument steriliser is recommended? Stats for achieving sterile instruments? How long would it take in each phase and total?
* Steam sterilisers
* Time required:
- 121 degrees for 15 minutes at 101 Kpa
- 132 degrees for 4 minutes at 203 Kpa
* Autoclave cycle times: 4 minute sterilisation time + 2 minutes safety margin + 16 minutes penetration + 25 minute drying time = 47 minute total cycle
What is maintenance in regards to fluid requirements?
* The volume of fluid needed to maintain zero fluid balance
* sensible losses- urine: varies with disease, generally 1-2 ml/kg/hr in health
* insensible (cutaneous, respiratory), faeces, saliva– expect 0.5-0.8 ml/kg/hr when healthy and resting– much higher when exercising, hyperthermia, etc.
What is MAC?
* Minimum Alveolar Concentration
* Minimum alveolar concentration (partial pressure) of an anaesthetic that produces immobility in 50% of subjects exposed to supramaximal noxious stimulus (skin incision or tail clamp)
* Measure of potency (ED50) that allows us to compare inhalation anaesthetics across species
Signs of chronic pain? Good assessment too?
* Behavioural changes: depression, sleep disturbance, irritability/aggression, social withdrawal, decrease in appetite, decrease interest in exercise, loss of playfulness
* reduced mobility (stiffness, lameness)
* lick granuloma etc.
* Helsinki Pain Index

Czerny retractor- deep or shallow
What are some possible complications for IV fluids?
Phlebitis, extravasation (leakage of fluid/cells out of vasculature), thombosis (especially with central lines), catheter related infections/ sepsis, embolism (catheter, air), risk of volume overload, exsanguination
What would you see on a leukogram in an inflammatory response? Stress response? Physiological leukocytosis?
* Inflammatory response
- neutrophilia and/or monocytosis
- left shift or toxic change
* Stress response
- lymphopenia
- mature neutrophilia +/- monocytosis (dog)
* Physiological leukocytosis
- neutrophilia and lymphocytosis in a young animal
Preferred sutures in muscle? Cardiac muscle?
Synthetic absorbable or non-absorbable sutures, Nylong and polypropylene cardiac muscle
What is hypothetico-deductive reasoning?
Problems most likely due to x and I’ll examine, test, etc. to verify
What are the advantages to TIVA?
* absence of theatre contamination
* rapid, smooth induction
* seamless transition from induction to maintenance
* easy to deepen anaesthesia
* rapid, predictable recovery of better quality
* Safer for patients with MH (malignant hyperthermia- severe reaction to anaesthetic drugs, genetic), asthma and other allergic conditions
* less stress response to surgery
* absence of nausea and vomiting/ appetite stimulation (propofol)
What would you see in a dehydrated patient?
* History of vomiting, diarrhoea, anorexia
* Clinical signs:
- Increased Hct/RBC/Hb (assuming no blood loss0
- Increased albumin (assuming no protein loss)
- Increased Na and Cl (assuming no electrolyte loss)
- Increased Urea with normal creatinine
Major Body System Assessment?
* Cardiovascular: pulses, mucous membranes, CRT, HR, cardiac auscultation
* Respiratory: RR, RE, pulmonary auscultation
* Neurological: gait, mentation
* Abdominal palpation
* Body temperature

How do you prevent ongoing absorption?
* Emesis
* gastric lavage
* Enema
* Cathartics & adsorbents
* Washing skin or eyes
When does ovulation occur after d0? When do oocytes mature? When does the cervix close? When is D1 in relation to d0?
* Ovulation occurs: 2-3 days
* oocytes mature: 4-6 days
* Cervix closes day 7
* D1 in relation to d0 is day 8

What is plasticity? Pliability? Suture pull out value?
Plasticity- degree to which suture will deform under load but then will go back to its original shape/ length when load is ceased
Pliability- ability of suture to change shape, related to ease of handling
Suture pull out value- load required to pull a suture loop out of tissue. relates mainly to tissue strength: fat<muscle>
</muscle>
What are the general effects of alpha 2 adrenoceptor agonists?
* dose-dependent sedation/hypnosis
* analgesia
* muscle relaxation
What are the 3 generations of Cephalosporins (why 3 generations?)? How do they work?

What are you evaluating with a pulse?
* rate and rhythm
* pulse profile: strength/ height, duration/ width, variability
* synchronicity with heart beat
* more difficult in cats
What are the two ways to administer TIVA? Advantages and disadvantages?
* Intermittent bolus– okay for cases < 5 minutes, simple, no special equipment required but large total drug dose and slow recovery
* Constant rate infusion (CRI)- smoother anaesthesia, deeper with time, risk of awareness of side effects (rate)
* Variable rate infusion (VRI)- smoother, lower total drug dose, faster recovery, frequent adjustment needed
* Target controlled infusion- computer, set of PK parameters for a given population, syringe driver– achieves stable plasma concentration, simple to use, easy to change in response to clinical effect
What are some long acting absorbables?
* Polydioxanone (monoplus, PDS)- 50% strength lost at 6 weeks
* Polyglyconate (Maxon)
* Glycomer 631 (Biosyn)- 50% strength at 2-3 weeks, but takes 90-110 days to be completely removed
What are the ways of making a diagnosis
Pattern recognition
Hypothetic deductive reasoning
Problem-oriented approach
Key abnormality method
To avoid ruminal tympany and regurgitation, what precautions should you take with a small ruminant during recovery from anaesthesia?
* be placed in sternal recumbency
* Endotracheal tube left in place
* Keep cuff inflated until swallowing
How do we avoid tumour cell resistance?
* Use multi-drug protocols that target different stages of the cell cycles, different modes of action, shouldn’t interfere with each other’s actions, not have overlapping toxicities

Hohmann retractor- large blades used in pelvic and long bone fractures. mini-Hohmann– used for exposure of the meniscus in the stifle joint and other fine work
Side effects of Halothane?
* Neuro: decreases cerebral metabolic consumption, increases cerebral blood flow therefore ICP
* Resp: decreases minute volume (ventilation), small increase in RR, increase in PaCO2, effective bronchodilator, apnoea occurs when anaesthetic depth is excessive
* CV: decreases CO due to decrease in myocardial contractility and SV, decreases BP du to decrease in CO, sensitizes heart to catecholamine induced arrhythmias
* poor muscle relaxation
* no significant analgesic effect
* Trigger for malignant hyperthermia
How is sevoflurane metabolized? Hepatic blood flow and oxygen delivery? Reactions with soda lime?
More than 97% eliminated unchanged by lungs
* less than 3% metabolized by liver and eliminated in urine
* Hepatic blood flow and oxygen delivery are better maintained than with halothane
*reacts with older formulations of soda lime and one of the breakdown products in potentially nephrotoxic
When is the optimal time for gastric lavage?
Within 1-2 hours of ingestion
What would vaginal cytology look like in a bitch in prooestrus?
* Shift from parabasal and intermediate cells to superficial cells (pyknotic nuclei, angular shape to the cytoplasm)
* Numerous red blood cells
* Neutrophils commonly observed
* Bacteria commonly observed

Nitrous Oxide MAC cat, dog, horse? Partition coefficient at 37C?
Cat: 250, Dog: 200, Horse: 200
PC: blood/gas: 0.5
What is the therapeutic index of a drug? How might it differ in chemotherapy than other types of drug therapy?
Ratio between toxic and therapeutic dose
* In chemotherapy, it really is the maximum drug tolerated– highest dose that can be given without unacceptable side effects
Off label vs. against lable
* Off label okay- use in a different way to label, in SA need consent from client and to be able to justify use e.g. to vet board and in food producing animals- single animal treatment only, need appropriate withholding periods
** Against label is counter to what the label says
Local anaesthesia of the mandible? What nerve? What dose?
(Anatomy: sensory (V))
* Mental: Lidocaine: 2-3 mL

What is the weakest point in the suture loop?
Knot- knot security is defined as the knot holding capacity expressed as a percentage of the original tensile strength of the suture material
What are EAGAR ratings?
Expert Advisory Group on Antimicrobial Resistance
* High- essential antibiotics for treatment of human infections where there are few or no alternative for many serious bacterial infections
e.g. 3rd generation Cephalosporins and Fluoroquinolones
* Medium- there are other alternatives but less than those for those classified as low
e.g. Anti-staph penicillins (Cloxacillins), amoxicillin- clavulanate, Trimethoprim-sulphonamides
* Low- reasonable number of alternative agents in different classes available to treat most infections even if antibiotic resistance develops
e.g. narrow spectrum penicillins, amoxicillin, tetracycline, neomycin, streptomycin, erythromycin
With an exploratory laparotomy what will you remove to increase visualization?
Falciform ligament, suction peritoneal fluid
What are the main effects of Acepromazine (Phenothiazine)?
* tranquillization
* anti-arrythmic
* anti-emetic
* spasmolytic
* antihistamine
* alpha 1 receptor blockade
What is used in orthopaedic surgery? Advantages? Disadvantages?
* Stainless steel- susceptible to cyclic stress and biofilm formation but is malleable and corrosion resistant, scratch resistant….
* Titanium- lighter than stainless steel for same strength, elasticity/ stiffness closer to bone, improved cyclic loading, improved osseointegration (surface to which bone can grow), less artifact for CT and MRI, more expensive
* Polymethylmethacrylate (PMMA, bone cement)- functions for fixation and load distribution with orthopaedic implants e.g. total hip replacement, pelvic or spinal fractures (composite repairs)… functions by interlocking with bone– cement– filler not a glue….. disadvantages: porous so infection impossible to eliminate once established
* Tantalum- modulus of elasticity is close to subchondral bone, texture and porosity is similar to cancellous bone so encourages osseointegration/ biological fixation.
Complications with laparotomy
* Seroma (pocket of clear serous fluid)
* Hypothermia (esp. young and small)
* Dehiscence and evisceration (wound ruptures along a surgical incision)
* foreign materials left in abdomen
* adhesions- restrictive or non-restrictive
* Peritonitis
* Infection
* Self trauma- suture knots too tight
* Skin irritation from clippers
Possible supportive medications for suspect poisoning?
* GI protectant (sucralfate, ranitidine, omeprazole/pantoprazole, misoprostal)
* Antiemetics (metoclopramide, maropitant)
* Analgesics


What do you often find with pancreatic disease?
Elecated amylase and lipase, cholestasis (Total bilirubin, conjugated bilirubin), elevated glucose
Other findings with pancreatitis
* Inflammatory leukogram
* Lipaemia
* Hyperglycaemia

What are the two Benzodiazepines?
* Diazepam
* Midazolam
(not licensed in animals)
When is Thiopental used?
* induction
* GA for short procedures
* onset of GA after IV injection: 15-30 seconds
* duration of GA: 10-20 minutes
What is the most accurate measure of marrow response to erythrocyte loss?
Reticulocytosis
How big should the vascular clip be in relation to the vessel diameter?
* Vessel diameter should be between 1/3- 2/3 of clip length
What are the physical signs of anaesthetic depth?
Palpebral and corneal reflex, eye position, jaw tone
** also monitoring mucous membrane colour, CRT, sublingual pulse, chest movement, skin temperature
What is the problem-oriented (database) approach?
Identify all the problems. Think of differentials for every problem. Test and examine to rule each in or out.
What is total protein? What does the level depend on?
Albumin + globulins
* Synthesis (liver function, inflammation) or loss (renal, GIT, third space, exudation)
* Hydration status
* Colostrum absorption in neonates
Side effects of NO? Muscle relaxation? Analgesia?
Neuro: Increases ICP
* Resp: does not change minute volume, effective bronchodilator, apnoea if excessive anaesthesia
* CV effects: symp nervous system, increases CO, increases BP
* No muscle relaxation
* Significant analgesic effect (NMDA)
Where do alpha 2 adrenoceptor agonists work?
* widespread distribution throughout the body
- sympathetic nervous system
- vascular endothelium
- CNS (spinal and supra-spinal)
- platelets
- uterus
- gut
Other than drugs, how else can you reduce pain?
Immobilisation, control of swelling/ oedema, check regularly (dry, comfortable), regular observation, monitoring urine output (ensuring bladder is emptied regularly), frequent turning, offer food, minimize stress
* Cryotherapy, thermotherapy (muscle relaxation)
* Active and passive exercise programs
* Transcutaneous electrical nerve stimulation (TENS)- joint mobility, decreased oedema, minimize disuse atrophy, muscle strengthening, sensory awareness, decrease pain
* Physical therapy
* Massage
What are the different laparotomy approaches? Why?
* Ventral midline (most common)
* Paracostal (extension for increased exposure- liver)
* Flank (ovariohysterectomy, grid gastropexy)
* Retroperitoneal (adrenal neoplasia)
What is transfixing?
* used for large blood vessels or pedicles when increased security is needed
* Halsted, modified transfixation and figure of eight techniques described
What is the name of the other intestinal forceps that are non-crushing, occluding forceps?

Allis tissue forceps- interlocking teeth
Babcock intestinal forceps
* Doyen intestinal forceps- delicate atraumatic grip- resection or anastamoses of stomach or intestinal
What the body fluid compartment rule?
60:40:20:15:5
total body water: intracellular fluid: extracellular fluid: interstitial fluid: intravascular fluid
Halothane MAC Cat, Dog, Horse? Partition coefficient at 37C
MAC (%)
* Cat 1.2
* Dog 0.9
* Horse 0.9
Partition coefficient @ 37C
Blood/gas: 2.4
Causes of renal azotaemia? What USG would you see in cats, dogs, horses and cattle?
* Poorly concentrated urine despite dehydration
- cats USG < 1.035
Dogs USG < 1.030
Horses and cattle USG < 1.025
* Acute renal insufficiency
- history
- hyperkalaemia
- oliguria or anuria
* Chronic renal insufficiency
- history
- polyuria
- often hypokalaemic
When should you NOT use Ketamine? What should you use in conjunction with Ketamine?
* Not for epileptic patients
* Not in cat with kidney dysfunction
* Not in glaucoma or “brain” patient
** use with muscle relaxant
When may rams not inseminate ewes?
* Poor libido
* Balanoposthitis (knob rot)
* Musculoskeletal problems
* 5 T’s: Teeth, torso, toes, tossle, testes
* Poor sperm output (not enough testis- size)
* Poor semen quality (heat: fever, scrotal mange; orchitis)

Classic muscle damage pattern
(not liver- ALT is hardly increased)

Cardiovascular forceps e.g. Debakey forceps
allow occlusion of only a portion of the vessel
In an exploratory laparotomy what will you find in the cranial left quadrant?
* Diaphragm
* Liver and gall bladder
* Stomach
When to biopsy?
* If FNA cytology non-diagnostic or equivocal
* If type of treatment would be altered
* If extent of treatment would be altered
* owners willingness to treat would change
* malignant neoplasia- to grade and plan
* goal is diagnosis for prognostic purposes
Halothane induction and maintenance? How does it compare to speed of induction and recovery and changes in depth during maintenance to iso and sevo?
Induction: 3%
Maintenance: 1-2%
** Slower induciton and recovery than Iso and sevo
* slower changes in depth during maintenance
What is responsible for the anaesthetic effect on the brain?
* Partial pressure– the blood, brain and other tissue compartments must fill up with anaesthetic before the partial pressure in the alveoli equilibrates with the partial pressure in the brain
* at equilibrium, the partial pressure is the same in each compartment but the concentration of anaesthetic in each compartment is dependent on solubility (partition coeffecient)
What classification does Etomidate fall under? Some facts?
* Imidazole derivative (IV anaesthetic agent)
* Kept away from light
* No CVS effect
* Mild respiratory depression
What is a pulse oximeter? What is the threshold for hypoxemia? What might you see in a hypoventilating patient?
Measures the saturation of oxygen with haemoglobin (SpO2) & HR
* arterial oxygen tension of 60 mmHg – oxygen saturation > 90%
* SpO2 can be normal in hypoventilating patients when the inspired oxygen fraction is increased (which normally should be the case during anaesthesia)
How do you calculate maintenance requirements?
[(BW x 30) + 70 ml/kg/day] / 24 hours
e.g. 4.79 ml/hr for a 1.5 kg animal
What are clinical signs of haemorrhage?
* Tachycardia, hypotension, poor peripheral perfusion/ peripheral vasoconstriction, weak pulses (decreased pulse amplitude), pale mucous membranes, slow CRT, mental depression, delayed recovery from anaesthetic

Weirlaner retractor– pointed or blunt– grip lock mechanisms
What is a common cause of failed fertilization due to bacterial disease? What does it cause? How does it spread? What do you do to the flock?
Brucella ovis– mainly male infertility… epididymis & testicular granulomas, ewe abortions rare
* Homosexual spread mechanical between male to male
*Lifelong infection, need to eradicate– cull and replace from accredited flock OR test and slaughter– serology 2-3 weeks apart

What happens to the anaesthetic concentration when the volume of the breathing circuit is small and the oxygen flow rate is high?
* The anaesthetic concentration changes very quickly
What are the kinds of things you want to know prior to surgery in a horse?
* Nervous system, CV and resp health?
* Medical history?
* Vaccinations (tetanus)?
*Allergies (penicillin)
* Genetic conditions (exertional rhabdo, hyperkalemic periodic paralysis)
What type of light is essential for reptiles? Why?
UVB- blocked by plastic and glass
* many reptiles use UVB to synthesize vitamin D3 and calcium metabolism
If you are using local anaesthesia on the eyelids, what would you use and what nerves are you blocking? Where?
(Anatomy: Sensory (V), Motor (III, IV, VI, VII))
* Supraorbital: Lidocaine: 1 mL
* Auriculopalpebral: Lidocaine: 2-3 mL

Advantages and disadvantages of cyanoacrylate glues?
Advantages: rapid application, application non painful (do not need GA), cheap
Disadvantages: low strength c/w sutures, shouldn’t be used on their own
Preferred sutures in a tendon?
Nylon and stainless steel, polydioxanone, polyglyconate
** prolonged tensile strength)
What is the ECF osmolality equation ? What is normal in dogs? cats? What is the tonicity equation
ECF osmolality (mOsm/kg) = 2 ([Na+] + [K+]) + Glucose + BUN
Normal in dogs = 300 mOsm/kg; cats= 310 mOsm/kg
Tonicity= Effective osmolality= 2 ([Na+] + [K+]) + Glucose
Where do Anti-inflammatory topical agents work?

ALT- good way to remember? What other enzyme also tells us similar things to ALT? What do you look at for cholestasis in a dog?
“Liver Trauma”– Also AST
* Cholestasis- ALP, GGT
How long do we suggest fasting and minimal water deprivation in monogastric animals (dogs, cats, horses)?
Ruminants?
small mammals, birds, neonates?
monogastric- 12 hours, no water withdrawal
ruminant- 12-36 hours (depending on size), 12 hour water withdrawal
small mammals, birds, neonates- short to no fast due to risk of hypoglycemia, no water withdrawal
Visual analogue scale for pain assessment

What is the one licensed alpha 2 antagonist? What will it reverse? Effects?
Atipamezole (Antisedan)– will reverse Xylazine, medetomidine, and dexmedetomidine
* will not fully reverse CV depression
Electrolyte levels depend on?
* Hydration status
* Loss (renal (Aldosterone), GIT, third space, exudation)
* Transcellular shift
* Na and Cl usually shift together
* Selective Cl loss occurs with vomiting and abomasal disorders
Topical vasoconstrictor? Dilution? Disadvantages?
Adrenaline- injected up the nose to control epistaxis or onto bleeding gastric ulcers
* Diluted 1:1000 to 1:10000 U/ml
* Disadvantage: systemic effects on CVS, profound local vasoconstriction leading to ischaemia
Nutritional recommendations with cancer
* High fat diets (theoretically cancer cannot use lipids for energy), calorie dense, increase protein content if renal function is acceptable, omega-3 supplementation
* Avoid high anti-oxidant diets because may interfere with chemotherapeutic agents
BUT if appetite is poor- get them to eat whatever they will
Stress leukogram? Inflammatory leukogram? Excitement leukogram?

Stress leukogram
What does vaginal cytology look like in a bitch in dioestrus?
* 1st day with <50% keratinized epithelial cells marks D1
* increase in parabasal and intermediate cells
* Many neutrophils observed
* “meoestral cells”: neutrophils found in cytoplasm
* copious amounts of vaginal discharge sometimes observed–> “Dioestral dumping”

Incisional biopsy vs. Excisional biopsy
* Incisional:
- diagnosis: cell origin, grade (invasion/mitotic index)
- complete removal not possible
- diffuse organ change (e.g. liver)
- include normal tissue
- multiple biopsies
- for cores, at least 5mm long
* Excisional: Definitive surgery & diagnosis
- surgical dose not altered by knowledge of tumour type (e.g. splenectomy for splenic mass)
- benign tumor based on cytology (lipoma)
- lymph node (staging)
- provides grade information
How do you monitor cardiovascular function?

What are Fluoroquinolones?

What are the three categories of crystalloids?
* isotonic- balanced (composition resembles ECF): LRS, unbalanced: 0.9% NaCl, 2.5% dextrose in 0.45% NaCl
* hypotonic- water for injection, 0.45% NaCl
* hypertonic- 7.5% dextrose in LRS, 50% dextrose
Why should haemorrhage be controlled?
* Severe haemorrhage–> hypotensive shock
* Blood obscures visualization in the operative field, irritates tissue, prevents tissue apposition, delays healing, potentiates infection
* Blood on instruments, drapes and tissues is an ideal medium for bacterial growth
What physiological differences make anaesthesia so difficult in horses?
* Neuro: opioid are more widely distributed: brain and spinal cord, autonomic NS, opioids= release of dopamine therefore changes in behavior and locomotor, inhalation anaesthetics cause a dramatic prolonged excitement phase during recovery from anaesthesia
* Resp: obligate nasal breathers, prolonged recumbency and nasal oedema can cause significant airway obstruction, dead space/ tidal volume ratio is relatively large, small changes in tidal volume can cause dramatic changes in alveolar ventilation and gas exchange, susceptible to compression atelectasis of the lungs when placed in dorsal recumbency
* CV system: horses very sensitive to the CV effects, alpha 2 agonists produce dramatic decrease in HR and CO, decreases in CO and BP associated with inhalant anaesthesia (2x other species), size and weight predisposed to poor muscle perfusion, ischemia, myopathy
What are enzymes that reflect liver damage (leakage)? Of those, what are also reflective of muscle? RBC haemolysis?
What enzymes reflect cholestasis?

When should you induce emesis? With what?
* Within 3-4 hours of ingestion
* Only if animal is stable
* only if animal is ambulatory
* not if poison is corrosive or volatile
*Washing soda- NaCO3, apomorphine, xylazine
When does fresh semen need to be inseminated after d0? chilled semen? frozen semen?

Preferred sutures of the skin?
Monofilament nylon and polypropylene
Indications for Intravenous Lipid Emulsion (ILE)?
*Local anaesthetic and other lipophilic drug toxicoses
* Bupivicaine, mepivacaine, ropivacaine, lidocaine, haloperidol, clomipramine, verapamil, carvedilol, amlodipine, propanolol, moxidectin, thiopentone
* Anecdotal reports in vet medicine: baclofen, permethrin, loperamide, bupropion, sertraline
Why doesn’t chemo work well on solid tumours detected later in their progression?
The number of actively dividing cells is decreased, sensitivity to chemotherapy and radiation therapy is reduced. Primary treatment is usually surgery and chemotherapy can be adjunctive
Evaluation of a pulse in an animal

When are straight needles used? Curved? Eyed needles?
Straight- placed by hand in skin
Curved- used in deep or small surgical fields with needle holders where working space is limited
* Eyed needles- reusable
When can suture coating be used?
* Reduce tissue drag, improve pliability and improve tying characteristics, reduce risk of infection (triclosan inhibits bacterial fatty acid synthesis)

Campylobacter abortion placentitis
What is metronomic chemotherapy? What drugs typically used? When are they used?
* Repetitive, low dose chemotherapy
* Higher frequency doses than standard protocols
* Drugs target stroma/blood supply and perhaps act immunologically against the tumour itself
* Usually low dose cyclophosphamide + piroxicam
* post operative management of sarcomas, inoperative tumours, following multi agent protocols
What is the clinical diagnostic portion of the pre-anaesthetic patient evaluation?
* CBC/ biochemistry (minimum PCV, TS, BUN, BG)
* Heartworm
* Thyroid function
* Coagulation
* Radiology
* Echo
Where do opioid analgesics and anxiolysis work?

Induction protocol small ruminant
* Lignocaine over 2 minutes (decreases laryngeal reflex- IV or spray over larynx)
* Thiopental IV OR propofol or Alfaxan IV

Why campylobacter is transmitted through ewe or doe mob
How is isoflurane metabolized?
* More than 99% eliminated unchanged by lungs
* Less than 1% metabolized by liver and eliminated in urine
* No hepatic or renal toxicity associated with metabolites
* Hepatic blood flow and oxygen delivery are better maintained than with halothane
What are you looking for in regards to storage of surgical instruments/ equipment?
* controlled air conditioning with low turbulence
* minimal traffic
* dry, with low humidity 35-70%
* temp < 23 degrees
* free from direct sunlight, dust, dampness, insects, vermin, and constant handling
* smooth washable surfaces
* positive pressure airflow with four air exchanges/hr
* storage in cabinets ideal- away from floor, wall, and ceiling
* no food, drink, non sterile goods
* kept away from water pipes
* Cardboard boxes not recommended- wire racks ideal
Causes of post- renal azotaemia
* Urinary obstruction/ uroabdomen
* Hyperkalaemia
* Variable USG depending on hydration status
Systemic diagnostic approach to any suspected cancer
- What is it? Neoplastic or non-neoplastic, tumor type/ cell of origin (round cell, epithelial, or mesenchymal)
- How bad is it? B or M. Grade?
- Where is it? Clinical stage (spread/extent of cancer), TNM system
What is complete remission, partial remission, stable disease, and progressive disease when it comes to cancer?

Pre-operative evaluation and preparation small ruminants?
* history, PE esp cardiac, pulmonary function, temp, hydration status, food witholding, body weight obtained, blood work performed, jugular catheter placed and secured to allow for admin of anaesthetic drugs and IV fluids
What is regenerative anaemia? Non-regenerative?
Regenerative- elevated reticulocyte count. Increased RBC loss- haemorrhage or haemolysis
Non-regenerative- normal or low reticulocyte count. Reduced rbc production- chronic disease/ inflammation, marrow disease, iron deficiency (** remember, is it pre-regenerative or true non-regenerative)
Signs of severe dyspnoea
* Extended neck
* abducted elbows
* open mouth breathing
* anxious facial expression
* increased abdominal movement
* paradoxical abdominal movement
* cyanosis
* lateral recumbency
* beware of rapidly changing body position and pupillary dilation in cats
What do you assess with neurological system?
* gait–> recumbency, single or multiple limb lameness, ataxia, paresis or paralysis
* mentation–> depressed, stuporous, comatose, hyperexcitable, dysphoric, hyesterical
What are the agents suitable for TIVA?
* Alfaxan CD- rapid clearance and minimal cumulation
* Propofol: rapid clearance, predictable metabolism, minimal cumulation
Animal factors that influence how effective chemotherapy can be
* Absorption- if there is primary GI disease, absorption of oral cytotoxic drugs may be affected
* Distribution- when drugs are highly protein bound, hypoalbuminaemia– issue with distribution
* Excretion- chronic kidney disease affecting renal clearance, more side effects
* Metabolism- decreased hepatic clearance of drugs

Balfour self-retaining abdominal retractor
What are immediately life threatening situations?
* collapse/ loss of consciousness
* seizures
* bleeding
* large or penetrating wounds
* choking or difficulty breathing
* protracted or severe vomiting
* difficulty urinating
* toxin ingestion
* previous life-threatening problems
How do I minimize bacterial resistance?
* By only treating with AMs when necessary
* By treating with appropriate AM regimes
* By ensuring owner compliance with treatment
* By performing C&S testing
* By not over-prescribing
* By preventing bacterial disease
When is there routine pregnancy diagnosis in mares, cows, and sheep?
* Mare: day 14
* Cow: day 28
* Sheep: day 75
Since alcohol is so good and so broad spectrum, why is it not used stand alone? What is the mechanism of action?
No residual action
Acts by denaturing proteins
All of the following are common reasons for inactivity of disinfectants. Which one is the most likely cause of failure for the majority of disinfectants?
A. Exposure to sunlight
B. Presence of organic matter
C. Incorrect dilution
D. Limited pH range
Presence of organic matter
What are the side effects of alpha 2 adrenoceptor agonists?
* respiratory depression (mild)
* initial period of hypertension resulting in reflex bradycardia–> decrease in blood pressure back to normal or below due to centrally mediated decreased sympathetic tone
* bradycardia
* cardiac arrythmias (A-V blocks 1 and 2)
* hyperglycaemia
* diuresis (problem in horses)
* decreased intestinal motility
* vomiting (mainly Xylazine in SA)
How do we start to define the problem list?
History
Clinical examination
Clinical pathology
Producton analysis
Clinical consequences of cancer
* expansile growth
* Destruction of host tissues & function
* Infiltration and metastasis
* Necrosis, ulceration and haemorrhage
* Cachexia
* hormone production (e.g. hyperCa)
* Reduced quality of life and reduced life span
How long does Limb IV regional anaesthesia last? What drug do you give?
60-90 minutes for lower limb surgery
Lignocaine 2 mg/kg only
Two common diagnostic techniques for cancer
** look at the cells by either. Using BOTH is the best interpretation:
- FNA for cytology (aspirational or non-aspirational technique)
* splattered onto a slide so lose the architecture
* looks at the individual cell detail
- Surgical biopsy for histopathology (incisional or excisional)
* patterns and structure of the tissue
Are “deep margins” qualitative or quantitative when resecting cancer?
* Qualitative– quality of the tissue e.g. fascia is an effective barrier to neoplastic cells while fat is a poor barrier

What are the types of margins of resection for tumours?

How do you interpret failure of fertilization in a ewe who returns to service? Who doesn’t return to service?
* Returns to service: something impairs sperm fertilizing egg but doesn’t disrupt normal oestrus cycle e.g. oestrogenic clover, mating young ewes
* Does not return to service: Pregnancy loss after maternal recognition of pregnancy, mating period coincides with beginning or end of normal breeding season, oestrus may cease if ewes are under severe nutritional stress
How do you safely correct hypertonic fluid loss?
* DO NOT increase Na+ by > 0.5-1 mmol/hr or > 12 mmol/24 hours
How do you calculate CO? What happens to CO when SV changes?
* CO = SV x HR
* When SV increases, CO increases

How long should tags be? Catgut? How many throws for multifilament? Monofilament?
3mm and 6mm in catgut
* 3 throws for multifilament, 4 for monofilament
Signs consistent with acute haemorrhage (hypovolaemic shock)?
* Tachycardia, hypotension, poor peripheral perfusion/ peripheral vasoconstriction– weak pulses (reduced pulse amplitude), pale mucous membranes, slow CRT, mental depression/ delayed recovery from anaesthesia
What happens when inhalation anaesthetic agents are less soluble in blood and tissues? Example?
Nitrous oxide
* Induction of anaesthesia is faster
* Changes in depth are faster during maintenance of anaesthesia (more control of depth)
* Recovery from anaesthesia is faster
Preferred sutures in blood vessel?
Polypropylene- least thrombogenic suture
Polytetrafluoroethylene, nylon, coated polyester, polydioxanone
How does hydromorphone compare to morphine?
* either times stronger than morphine
* better sedation than morphine
* emesis less likely
* no histamine release
What increases MAC?
* Hyperthermia, ephedrine, opioids (horse)
What are two common reasons to postpone elective surgery in horses?
Febrile with abnormal WBC count
* at least 3 weeks in horses with a recent history of respiratory disease
What does hypothermia cause?
* Causes vasoconstriction
* Helps reduce swelling and has analgesic properties
* e.g. cold packing nose for epistaxis or stifle following cruciate surgery
What is the difference between crystalloids and colloids?
* Crystalloids- solutions of water and solutes capable of entering all body fluid compartments
* Colloids- large molecular weight fluids restricted to the plasma compartment in patients with an intact endothelium
Tachypnoeic?
More than 1 breath per second
Definition for chronic pain
Pain that extends beyond the expected time of healing… no useful protective function, debilitating, poor QOL
Isoflurane MAC in a cat, dog, horse? Partition coefficient at 37C?
* Cat: 1.6
Dog: 1.4
Horse: 1.4
* Partition coefficient:
- blood/gas: 1.4
In an exploratory laparotomy what will you find in the caudal left quadrant?
* Spleen
* Rectum, colon, caecum
* Mesenteric root and LN
* Ileum
* Jejunum
*Mesocolon to retract viscera to expose left kidney and adrenal ( can see aorta)
What is surgical mesh used for? Complications?
Close defects e.g. chest wall reconstruction, perineal hernia
* augment/ buttress primary repairs of slow healing tissue e.g. tendon
* prosthetic replacement for tendons
Complications: infection, viscercal adhesions, failure
What is a buller steer? What are the predisposing factors?
* A steer that is mounted by other steers
* Predisposing factors: - implanted with stilboestrol or oestrogen, high stocking density, mixed groups of steers, crowded conditions (especially in warm weather)
When is electrosurgery useful? Disadvantages?
Effective for arteries up to 1 mm and vessels up to 2 mm
* Disadvantages: tissue damage and charring (do not use close to vital structures), can lead to longer healing times, rebleeding can occur due to the probe sticking to affected tissue, fire risk if used near flammable materials
When is propofol a really useful tool, what kind of surgery? When should you never use propofol?
* Decreases cerebral metabolic requirements for oxygen, cerebral perfusion prssures and causes a corresponding decrease in ICP and intraocular pressure
* Do not use in maintenance of anaesthesia for caesarian sections because it crosses the placenta and may affecte neurological and cardiorespiratory variables in puppies and kittens
Glucose levels depend on?
* Carbohydrate intake
* Hormone balance- insulin, cortisol, glucagon
* Utilisation- exercise, sepsis
Common causes of embryonic or foetal loss in small ruminants and when in gestation

When might ewes be in anoestrus?
* Haven’t reach puberty yet either due to being too young or too lightweight
* Have reach puberty but too low bodyweight/CS
* Wrong time of year- short-day breeders (less seasonal breeders can be induced with ram effect)
* Some toxins affect reproductive hormones and suppress oestrus (e.g. coumestans from lucerne/ white clover)
What do you assess with the cardiovascular system?
* Mucous membranes
* Capillary refill time
* Pulses
* Heart rate
* Cardiac auscultation
What are the disadvantages to TIVA?
* Expensive (Alfaxalone > Propofol)
* Varying response to standard dose- age, sex, obesity, haemodynamic states
* no “self-regulation” of anaesthetic depth


Parameters when you see cyanosis?

What are the advantages to using inhalation anaesthetics?
* Administered in oxygen
* Secure airway (endotracheal tube)
* Rapid induction of anaesthesia
* Better control of depth during maintenance of anaesthesia
* Rapid complete recovery from anaesthesia
* Rapid elimination with very little metabolism
What are the different margins of resection with cancer?

What are the 3 Ms in behavior treatment plans?
Management, Modification, Medication
FNA Cytology Advantages and Disadvantages

Anaesthesia of the maxilla what nerve? How much?
(Anatomy- sensory (V))
*Infraorbital: Lidocaine 2-3 mL

What happens in regards to induction speed, depth control, and recovery with slow deep breaths vs. rapid shallow breaths?
* Slow deep breaths– patients have good alveolar ventilation and a fast rise in alveolar anaesthetic concentration (partial pressure), depth is easier to control, and recovery is faster
* Patients that take rapid shallow breaths– have poor alveolar ventilation and a slow rise in alveolar anaesthetic concentration (partial pressure), depth is harder to control, and recovery is slower
Considerations for laparotomy closure
* Lavage abdomen with warmed 0.9% NaCl (warm to help correct hypothermia)
* Volume 20-50 ml/kg
* should be clear after repeated lavage otherwise may need to explore to bleeding, contamination
What are some signs of oestrogenic clover disease? Cause? Diagnosis?
* Signs: more older dry ewes, increased teat length, precocious lactation, enlarged genitalia in wethers and dry ewes, vaginal or uterine prolapse
* Caused by phytoestrogens– impaired sperm transport or chronic uterine change
* Diagnosis: identify clover, wether teat length assay, uterine histopathology
* Treatment: avoid risk pastures near joining, cull at younger age, graze cattle, reduce stocking rate to increase grass and decrease clover, pasture renovation

What is metastasis?
Dissemination of neoplastic cells to discontinuous other sites to form a detectable (macroscopic) tumour

What is in the critical category of risk according to Spaulding’s risk classification of surgery related items? Examples?
* entry or penetration into sterile tissue, cavity or bloodstream
* Surgical instruments, surgical implants
* all items must be sterile
What are the gram negative oxidase negative, oxidase positive, gram negatives that behave like gram positives, and acid fast?
* Acid fast- Mycobacteria (Nocardia)– acid fast don’t really matter because we don’t treat them anyway

What kind of animal is MAC for isoflurane the lowest?
Cow- 1.4%
What are the risks of mechanical ventilation?
* Oxygen toxicity (decreases pulmonary function, pulmonary oedema, species-specific)
* Barotrauma, cardiovascular depression, infection
What is the endotracheal tube cuff for? How do you check for a leak?
* Allows sealing of the airway to prevent aspiration and to provide positive-pressure ventilation without air leaking– but over inflation can cause necrosis and stenosis of the tracheal mucosa
* Turn off O2 and pop off valve, and listen for a leak at the same time than someone else is giving a breath to your patient. If a leak is present, inject air into the cuff while listening until the leak has disappeared.
What are tumours where radiation treatment is used?
* Nasal carcinomas, brain tumours, thyroid cancer, oral tumours (SCC, MM), incompletely excised MCT and STS
Where do you give a cranial epidural in a small ruminant? When is dose backed off?
Lumbosacral space, approx 3 cm caudal to the line joining the anterior borders of the ilium
*Dose is 2/3 in pregnant or obese animal because epidural space volume is reduced either by vessel engorgement or fat deposition respectively
With circuit volume– what is the difference between large and small animals?
* SA circuits have relatively small volumes and the anaesthetic concentration can be changed quickly
* LA circuits have relatively large volumes and the anaesthetic concentration cannot be changed quickly
Required equipment for exploratory laparotomy
* General surgery packs and instruments
* Balfour self-retaining retractors
* Laparotomy sponges
* Suction (Poole, Yankauer, Frazier)
* Culture tubes or swabs
* Formalin and containers for biopsy samples
* Appropriate selection of suture material
Side effects of cyclophosphamide?
Haemorrhagic cystitis (Diuresis with frusemide at time of treatment)
How long after haemorrhage will a dog develop reticulocytosis?
3-5 days
In an exploratory laparotomy what will you find in the cranial right quadrant?
* Duodenum
* Pancreas
* Portal vein and caudal vena cava
* Right kidney and adrenal
Preferred suture material in Hollow viscus (viscera)? What should you NEVER use in the bladder?
* Synthetic absorbable sutures, surgical gut, monofilament non-absorbable
* do not use polyglycolic acid in the bladder may be absorbed in urine

Currettes- scraping tissue or material from cavity walls, obtain cancellous bone grafts, to debride and sample bone, remove nucleus pulposus during intervertebral disc fenestration
Volkmann- double ended
Spratt bone currette- round cup
What is cryosurgery and when is it used?
* Controlled use of freeze/thaw cycles to destroy tissues (-22C); 2-3 freeze/thaw cycles per treatment using Nitrous Oxide or Liquid Nitrogen… cheap can use with sedation, disadvantages: no tissue diagnosis if no pre treatment biopsy, lack of ability to assess tissue margins
* Small masses, eyelid/ear/nose tumours, SCC/histocytoma, animals not suited for anaesthesia/surgery
GI Toxicity that occurs during chemotherapy?
* Nausea, vomiting, inappetance, diarrhoea
What is used for pressure/ tamponade?
* gauze swab with digital pressure ( definitive haemostasis– 4 minutes)
* counterpressure bandage post abdominal surgery– do not include ribcage
* packing the nasal cavity
What are the major benefits to using Propofol?
* “To effect” at induction
* Smooth, rapid recovery
* Lack of excitement at induction
* Lack of hangover in recovery
* Non-cumulative nature
* Ability to use as CRI
* Hepatic disease
When should certain AMs be avoided or contraindicated?
* Major organ disease- especially kidney disease (aminoglycosides, oxytetracycline)
- liver disease- (rifampin)
- neuromuscular disease (aminoglycosides)
* age of patient: adult horses (macrolides- due to AM associated colitis)
- foals (enrofloxacin)
* Physiological state e.g. pregnancy
* Previous hypersensitivity reaction
* no good rationale for use
What happens to the anaesthetic concentration when the volume of the breathing circuit is large and the oxygen flow rate is low?
* The anaesthetic concentration changes very slowly
What are some special considerations for diabetic patients pre-anaesthesia?
* schedule for first procedure of morning
* evening meal and insulin the night before
* ideally small meal in the middle of the night and 1/2 insulin
* no morning meal
* check glucose pre-op– if normal and < 500 g/dL- no AM insulin, if >500 g/dL- 1/2 dose AM insulin (hyperosmolar concerns), if low- provide supplemental glucose

Thenar grip- no change in grip when releasing and re-grasping needle
Tripod- allows precision when releasing needle, although slower
Palmed- suturing tough tissue, less precise

Where is short acting absorbable suture used? Long acting? Where should you avoid using braided sutures?
Rapidly healing tissue like stomach or bladder, slow healing like fascia with poor blood supply long acting
** braided sutures should NOT be used in the GIT due to capillarity
What is performed in the pre-breeding exam of a bitch?
* Signalement, history
* General exam, esp. hereditary diseases
* special repro exam
- digital palpation of vulva and vagina
- vaginoscopy
- cytology
- microbiology?? waste of time and money
* B. canis test
What does aseptic technique refer to?
* Scrubbing, gowning, gloving, skin preparation of the patient, theatre etiquette/ protocols, standard precautions
What are Tetracyclines?

What is tensile strength? Capillarity? Mechanical creep/ stress relaxation?
Tensile strength- load at which the suture fails
Capillarity- wicking of fluid along a suture
Mechanical creep/ stress relaxation- tendency of suture to slowly and permanently deform under constant stress

Olsen-hegar needle holder (with scissors– allow suture to be tied and cut)
Why do we suggest fasting and minimal water deprivation in pre-anaesthetic patients? What is the one exception to this?
Anaesthetics relax the lower oesophagus sphincter and decrease GI motility
* risk of regurgitation and aspiration
* risk of bloat
* risk of ileus (obstruction)–> very uncomfortable post op
** emergency–> exception!!!
What happens to PaCO2 when minute volume changes?
Blood carbon dioxide levels (PaCO2) generally vary inversely with the minute volume, an animal with an increased minute volume e.g. due to hyperventilation should demonstrate a lower blood CO2 level

Onion grass poisoning can cause early abortion
* toxin from fungus growing on grass
* Can cause neurological signs as well (staggers) in adults
Numerical Rating Scales for pain
1-10
* Better than SDS but not as sensitive as VAS (inter-observer reliability)
what decreases MAC?
* Sedatives, analgesics, injectable anaesthetics, hypothermia, pregnancy, extremes of age, severe hypercapnia, severe hypoxemia, severe anaemia
What happens with hypotonic fluid loss? What can cause this? CNS effects?
* Water is lost in excess of solutes
* Results in hypertonicity of the ECF (hypertonic dehydration)
* Hypernatraemia, hyperosmolality ** important because neurons do not like to be dehdrated
* e.g. heat stroke, water deprivation, exercise (panting), vomiting, diarrhoea, polyuria, iatrogenic
* chronic hypernatraemia–> increase in neuron idiogenic osmoles to match ECF tonicity (neurons make extra molecules– amino acids to cause their intracellular osmolality to go up to bring more water in)…. rapid correction of ECF hyperosmolality–> cerebral oedema.
What are some signs a bitch is in heat?
* Flagging- lateral deviation of the tail
* winking- upward tipping of the vulva
* lordosis- standing firmly and arching her back
* note vaginal discharge
What are side effects of doxorubicin?
Cardiac toxicity
Which is most likely to attack a person: entire male, entire female, neutered male, or neutered female?
Entire female

What are some fluids that are acidifying? When would you give them?
* 0.9% NaCl
* no buffer, relatively high chloride= acidifying effect
* ideal for hypochloremic metabolic alkalosis seen with high gastrointestinal obstruction OR perhaps a patient with lots of vomiting (losing HCl)
What is the most common scalpel blade used? What is a No. 11 used for? What is a smaller version of the most common scalpel blade? What are the different grips?
No. 10
* No. 11 ideal for stab incisions into fluid- filled structures such as organs
* No. 15 smaller No. 10
Grips: fingertip grip, pencil grip (more precise movements) or palmed grip
Why does the anaesthetic move from the breathing circuit into the alveoli, blood, brain, and other tissues?
* during the induction period, the anaesthetic concentration (partial pressure) in the breathing circuit is higher than in the alveoli, blood, brain, and other tissues
* Anaesthetic moves down the concentration gradient (into the patient), and distributes between the alveoli, blood, brain, and other tissues until equilibrium is reached
What is the difference in the progesterone profile in the pregnant vs. non pregnant bitch?
* in the pregnant bitch sharp drop off of progesterone about 62 days after LH peak

Common side effects of chemotherapeutic drugs?
anaphylaxis, perivascular sloughing, slow regrowth of shaved areas, loss of whiskers, myelosuppression
What is tumour grading? How do pathologists grade tumours?
* provides info on the potential behaviour of tumours
* Degree of cellular differentiation (pleomorphism)
* number of mitotic figures (growth rate)
* degree of necrosis/ haemorrhage
* evidence of local invasion
* presence of metastasis (vascular and lymphatic)
* varies with type of tumour– low v. high grade or numerical 1-3
When we have azotaemia, what question do we ask?
Is it prerenal, renal or post renal?

What is an ideal induction agent in animals with low cardiac reserve and hypovolaemia?
Etomidate because it produces minimal cardiovascular changes
What are some common sedative-analgesic combinations in horses?

Unique facts about bitch repro? When is first oestrus cycle? When is puberty? How long is the IEI?
* Non-seasonal breeders
* Spontaneous ovulation
* Puberty at time of first oestrus cycle 3.5 to 24 months (breed dependent)
* Interoestrus interval (IEI): average 7 months, range 5-12 months
Tests to run if suspecting toxin
* PCV/TP
* Glucose & Calcium
* Electrolytes
* Urine
MAC of sevoflurane
Cat: 2.6
Dog: 2.3
Horse: 2.3
* Partition coefficient at 37C- blood/gas: 0.7
What is the mechanism of action of ILE? Potential side effects?
* Lipid sink effect
- lipid emulsion provides separate plasma compartment for lipophilic agents to partition into results in less free drug available to other tissues
* Side effects: allergic reaction, rare, anaphylactoid-like signs, fever, nausea, vomiting, dyspnoea, tachypnoea, cyanosis, arrhythmias, hypotension, CVS collapse, fat overload syndrome (when endogenous lipid clearance mechanisms overwhelmed), fat embolism, hyperlipidaemia, hepatomegaly, icterus, splenomegaly, thrombocytopenia, prolonged clotting times, haemolysis, hypertriglyceridaemia, mild increase in HR, transient decrease in pH, altered pulmonary function, hypercoagulability, fluid overload, interfere with lab tests, interaction with other drugs (e.g. anticonvulsants)

Listeria abortion


Senn-Miller and Mathieu retractors– two kinds– similar– Retract skin and superficial muscle layers (no good for large muscle mass)
Special considerations for anaesthetizing ruminants
What are the isoflurane and sevoflurance vaporizer settings and MACs for induction and maintenance?
* Isoflurane:
- induction: 3% (2 MAC)
- Maintenance: 1-2% (1 MAC)
* Sevoflurane:
- Induction: 5% (2 MAC)
- Maintenance: 2-3% (1 MAC)
Why do we look at the pancreas and the liver together?
The ducts open really close to each other– if you have something going on with the liver or pancreas there can be damage to the duct…. especially if cholestasis always consider both the liver and the pancreas

What else do you monitor other than cardiovascular function?
* Renal function: BP and urine output
* Temperature: hypothermia and rewarming or hyperthermia
What are ongoing losses?
* Any losses in addition to usual metabolic losses e.g. vomiting, diarrhoea, polyuria, pleural or peritoneal effusion, blood loss, excess panting, wound effusion, haemorrhage
* difficult to quantify but should be estimated

Pyometra
Where do NMSA receptor antagonists work? Example?
Ketamine

NSAIDs anti-inflammatory
* Phenylbutazone, Flunixin, Ketoprofen
* reduces inflammation
* significant side effects: platelet function, renal blood flow, GI ulcers
* Long duration of action (12-24 hour)
What order do you biopsy organs?
* Clean organs before clean-contaminated organs
* Liver/pancrease/spleen first
* GIT order: stomach, duodenum, jejunum, ileum
*adrenal: FNA preferred over biopsy due to significant bleeding and catecholamine release
* Kidney and colon not routinely biopsied
What are the stages of anaesthesia?
I. Disordered consciousness, voluntary movement
II. Excitement (may be unnoticeable with heavy premedication or narcosis)
III. Surgical anaesthesia (resembles natural sleep)
IV. Overdose
What happens to induction, depth, and recovery in patients with high blood flow vs. low blood flow?
* High blood flow– good alveolar perfusion and a slow rise in alveolar anaesthetic concentration (partial pressure), induction is slower, recovery is slower
* low blood flow– poor alveolar perfusion and a fast rise in alveolar concentration (partial pressure), induction is fast, and recovery is faster
Local Anaesthetics used in horses
* Lidocaine: few systemic side- effects, short duration of action (1-2 hours)
* Mepivacaine: few systemic side effects short duration of action (2-3 hours)
* Ropivacaine: few systemic side- effects, long duration of action (3-4 hours)
* Bupivacaine: few systemic side- effects, long duration of action (4-6 hours)
Name some absorbable and non-absorbable suture material?

What are important things you need to know when using Alfaxalone as an IV anaesthetic agent?
* Twitching/ paddling in recovery is possible in cats
* Usually stop if stimulation ceases
* Dramatically reduced by premedication
* Respiratory depression at induction – same with propofol
* Decrease in arterial BP (< propofol)
Tumour cell resistance
* Major mechanism of chemotherapy failure
* Failure at any point responsible for chemosensitivity
* Multidrug resistance- tumour cell express transporters that actively express drug from the cell
What do you require to monitor when you suspect a poisoned patient?
* Maintain renal perfusion
- IV fluids
- urinary catheter
- monitor urine output
- monitor: urea, creatinine, electrolytes, PCV, TP
Where do Spinal and systemic anaesthesia/analgesics, and anti-inflammatories work?

What are some examples of colloids?
* Starches, gelatins, albumin/ plasma, 20% mannitol
Is this anaemia regenerative or non regenerative? What is the most likely cause?
* Regenerative
* Haemolysis


Toxoplasma focal cotyledon lesions
What is d0? What is days 1-7? What is D1?
* d0= day of the LH surge- first day serum progesterone doubles/ rises > 2ng/ml
* days 1-7 = days of oestrus- in relation to LH surgey
* D1= first day of dioestrus- based on cytology (decrease of keratinised cells to < 50%)
What are the the clinical groups of shock?
* Hypovolaemia: decreased blood volume
* Maldistributive: inappropriate vasodilation
* Obstructive: block to cardiac filling
* Cardiogenic: pump failure
What are Aminoglycosides?

What are the factors that determin the rate and speed of onset of anaesthesia?
* anaesthetic used: lipid solubility, molecular size, protein binding, ionization
* dose
* rate of administration
* route of administration
* animals level of consciousness
* acid-base, electrolyte, and serum protein status
* animal cardiac output
What can be used for corrosive ingested agents at home?
Milk
How does methadone hydrochloride compare to morphine?
* similar analgesic profile to morphine
* no vomiting
* NMDA (not morphine)
* long half-life in humans, so many cumulate with repeat doses
* duration - 4 hours in dogs and 6-8 hours in cats
How do you treat hypotension during surgery?
* Check anaesthetic depth
* Check HR
* Rapid fluid administration
* IV dobutamine administered to effect, dopamine administered to effect
What does Campvax protect against?
Campylobacter fetus subsp fetus and C. jejuni
What happens when the concentration in the breathing circuit is changed during the maintenance period?
* anaesthetic redistributes until a new equilibrium is reached
* Equilibrium is reached when the inspired anaesthetic concentration is equal to the alveolar or end-tidal concentration
What does cyanotic mucous membranes mean? Icteric? Brown? Cherry red?
* Cyanosis: hypoxaemia, paracetamol, polycythaemia
* Icterus: blue to gree eyes
* Brown: paracetamol
* Cherry red: carbon monoxide poisoning


When do you start breeding the bitch (2 options)? How do you accurately determine oestrous?
* fixed day breeding- e.g. breed day 12 and 14 after onset of prooestrus
*based on behaviour- start breeding every other day during time when bitch stands for the male
** Accurately detect oestrus:
** start in prooestrus, sampling every 2 to 3 days (M, W, F)
- serum progesterone levels (10-25 ng/ml at time of fertile period but variable… aim for breeding 15-20 ng/ml)
- test for “breeding reflexes”
- vaginoscopy
- exfoliative cytology
What are classifications of antibiotics?
* Class of antibiotic e.g. penicillin, aminoglycoside
* Spectrum of activity: broad or narrow
* Effect on bacteria: bacteriostatic or bactericidal
* Mode of action: inhibit cell wall synthesis, membrane function protein synthesis, etc
Behavior is impacted by?
Genetics, environment (internal and external), experience
What are the side effects of Acepromazine (Phenothiazine)?
* hypotension- care with hypovolaemic patients
* collapse in some families of boxers
* decreased seizure threshold
* hypothermia
How is hair clipped for exploratory laparotomy?
* from caudal thorax to perineum and laterally 5-10 cm (xiphoid to pubis)

What is the most likely cause of azotaemia?

* Acute renal insufficiency because bladder was small and soft (vs. if we couldn’t detect it or if it was hard- obstruction), collected urine, poorly concentrated and hyperkalaemic (this cat actually ingested lilies)

Rochester- Carmalt forceps have longitudinal serrations– larger crushing forceps used primarily for large tissue bundles such as ligation of vascular or tissue stumps and pedicles such as during an ovariohysterectomy. (a few cross striations to prevent tissue slippage)
What are the best two things about monofilament suture material?
Increased memory, less tissue drag
* but less pliable, poorer handling
What is selection pressure in regards to chemotherapy?
* If we don’t kill a particular cell line with chemotherapy, we will engender them to resistance
* Survival of the fittest
What are the main sources of contamination?
* the patient- skin or haematogenous
* surgical equipment and implanted biomaterials (sutures, plates, screws)
* surgical personnel
* operating environment- including airborne particles
How do you calculate minute volume (ventilation)?
volume of gas inhaled or exhaled per minute
minute volum = tidal volume x respiratory rate
How do you calculate BP? Is BP a reliable measure of CO?
BP = peripheral vascular resistance (PVR)/ CO
* BP and HR are not reliable for CO sudden severe hypovolemic hypotension
What are the foundations of reptile husbandry?
* heat (and light)
* hide
* humidity
* health
* hygiene
* healthy appetite
* habitat
* handling
When do you choose palliative care?
* Concurrent disease that contradicts chemotherapy options (GI disease)
* Systemic health
* Unable to cure or long-term remission
* Owners unable to afford or consider chemotherapy
* Age alone is not a reason
What treats osteosarcoma? Side effect?
Carboplatin, renal toxicity (diuresis)
When are blunt points of needles used? Taper fine point? Cutting?
* Blunt- friable tissue e.g. liver
* Taper fine point- delicate tissue e.g. GI tract, bladder, muscle
* Cutting- tough tissue skin, peritoneum, fascia
Approximately how much blood is contained in a blood-soaked surgical swab?
10 mL- hence counting the number of blood-soaked swabs and measuring the volume of blood collected in the suction bottle will give an indication of the amount of blood loss
The most effective way to control diffuse capillary bleeding from the surface of a parenchymatous organ is:
oxidised regenerated cellulose or gelatin to cover the bleeding surface
* local compression can produce the same effect but is time consuming. Suction can disrupt clot formation
How are stainless steel instruments normally sterilised? Flexible endoscopes? Packaged suture materials?
Stainless steel instruments: steam under pressure
Flexible endoscopes: peracetic acidor high level disinfection OPA Cidex
Packaged suture materials: gamma irradiation
Metzenbaum scissors are recommended for dissection tissues because:
Gross movement of the shank is translated to fine movement of the blades

Electrosurgery involves the use of an electrical current which is passed between two electrodes, producing heat within the tissues. The heat is produced as a result of the tissues:
Resistance
What type of steam is required for correct sterilisation?
Dry saturated steam
Which of the following instruments may be used to safely hold the small intestinal wall without causing excessive trauma?
Babcock tissue forceps

Povidone Iodine is sometimes used instead of Chlorhexidine for the following reasons
Antifungal property
What property of nylon makes it difficult to handle?
High memory– difficulty in handling and decreased knot security
PDS (Polydioxanone) loses 50% of its tensile strength in how many days?
28 days
What is the order you would apply solutions in preparing a patient for surgery?
- Chlorhexidine scrub solution
- 70% alcohol spray
- Chlorhexidine in 70% ethyl alcohol
Which of the following cannot be considered a sterile surgical barrier?
* Scrub suits, scrub gown, face mask, surgical gloves
* Scrub suits and face mask
What is the best technique to prepare the patients skin before surgery?
Gentle scurbbing in a circular motion from the incision site towards the periphery– vigorous scrubbing has two disadvantages: create abrasions on the skin and bring follicular bacteria to the surface which then infect the abrasions.
Which material is traditionally used to tie ligatures around large blood vessels?
Silk
What type of knot would be used to tie a secure surgical knot?
Square knot
What is the minimum number of throws which should be applied when tying a suture knot?
3
What percentage of alcohol optimizes its antiseptic activity?
70%
What are the sterile barriers in surgery?
What are the non-sterile barriers?
Surgical gowns and surgical gloves are the sterile barriers
Non-sterile: scrub suits, surgical head covers, face masks, shoe covers, skin scrub
What is surgical etiquette?
There is a correlation between the number of people and their movements, and the number of airborne bacteria in the operating theatre. Therefore it is important to reduce the number and movement of people in and out, and within the surgical theatre.
Only the front of the gown, from mid chest to waist, the sleeves and gloved hands are considered “sterile”.
The surgeon and assistant should always be conscious of the “sterile field” and take all precautions to prevent a breakdown in aseptic technique.
Non-sterile personnel should not walk in front or in-between an open sterile trolley.
The first rule of conversation in the operating room is silence! Noise, whether it is conversation, music or phones ringing are a distraction that interrupts patient care and potentially increases the risk of error.
Any conversation should be kept to the task at hand unless the surgeon initiates conversation however this is not a green light to continue casual conversations.
Personal mobile phones or other devices should not be taken into theatre.
What is the preoperative assessment and management?
- History
- Physical Examination
- Diagnostic Techniques
- Collecting and Organising Information
- Surgical Planning
Allows comparison of the patient prior to and following surgery, risk profile, etc.
What are the steps to surgery preparation??
** Reducing SSI
- Hair removal
- Skin preparation
- Patient Draping
- The Sterile Field
Why is clipping preferred to shaving?
General recommendations for clipping?
Shaving produces small lacerations which has been shown to increase post-operative infection rate up to ten fold
No. 40 clipper blade with a minimum of 15 cm on each side of the incision
* Clipping:
- replace blunt clipper blade
- clean clipper blade before each use or preferably after each use
- use a coarser blade for denser coats (No. 10 vs. No. 40)
- clip initially along hair growth pattern; against hair for a closer clip
- replace blades with missing teeth– apply flat on skin to reduce clipper lacerations
- avoid excess heat production from continuous heavy usage to reduce clipper burns
- skin over irregular areas can be effectively clipped by applying tension to the skin or sliding it over to an adjacent flat area
- ensure edges are straight for owner acceptance and easier drape application
What the difference in concentration of chlorhexidine in skin antisepsis vs. open wounds?
skin antisepsis: 0.5% Chlorhexidine + 70% alcohol
open wounds: 0.05% Chlorhexidine solution using sterile water is recommended
What is the problem with povidone iodine?
inactivated in the presence of organic material, especially blood and has poor residual activity… inactivated by alcohol
* High incidence of skin reactions
What is the order of placement of drapes?
Near, top, tail, and far
How can you diminish blood supply during surgery?
* Rough tissue handling
* improper use of instruments
* Prolonged exposure
What factors influence the degree of tissue injury?
- A knowledge of surgical anatomy
- Careful dissection
- Dissection under gentle traction
- Tissue must be kept moist during dissection- dry tissues result in an inflammatory response and potentiates adhesions between tissues such as the intestine-warm sterile saline
- Avoid transection of muscle bellies
- Keep operative time to minimum
- Close dead space
- Reduce the amount of foreign bodies within the wound
What are allis tissue forceps used for? Babock tissue forceps? Doyen intestinal forceps?
* Allis tissue forceps- hold the linea alba during an ovariohysterectomy or laparatomy
* Babcock tissue forceps- urinary bladder during cystotomy
* Doyen intesinal forceps- for intestinal anastamosis
What is the most common bacterial contaminant of orthopaedic procedures? What about lower GIT surgeries?
** What is the prophylactic antibiotic of choice for most vet surgeons?
* S. aureus in orthopaedic procedures ( from the skin)
* Coliforms and anaerobes in lower GIT surgery
** Cephazolin, a first generation cephalosporin which has efficacy against coagulase positive staphylococci and E. coli,
** low toxicity, cost effective and prolonged duration of activity
Why is haemostasis important during surgery?
* excess bleeding obscures the operative field
* blood on cloth drapes allows passage of bacteria through the drapes into the surgical field
* Post operative haemorrhage or haematoma formation delays healing and encourages infection
* Protracted haemorrhage may result in anaemia, poor healing and haemorrhagic shock
Methods to control haemorrhage
* Compression (digital pressure 2-3 minutes)
* Crushing- haemostatic forceps on severed blood vessels will stimulate vasoconstriction and clot formation (by the exposure of sub-endothelial collagen, a potent platelet activator)
* Torsion- also creates further damage to the vessel wall and exposes sub-endothelial collagen
* Ligation with SILK OR metal ligation clips
* Suturing with polypropylene
* Tourniquets e.g. lower limb surgery- esmarch’s bandage used in the distal limb of horses
* Stypics: open wounds– adrenaline, ferric chloride, silver nitrate
* Absorbable haemostatic agents– sheet of material or powder– e.g. liver– gelatin sponge, oxidised cellulose, calcium alginate fibres, fibrin sealants and glues, topical thrombin, bone wax
* Systemic haemostatic agents (Tranexamic acid, delta aminocaproic acid)- delay fibrinolytic activity– vitamin K for warfarin
* Surgical diathermy or electro-surgery- high frequency alternating current traveling between two electrodes to produce local heat in tissues because the electric current attempts to travel through the tissues, they act as a resistor and produce heat, which achieves tissue injury and protein coagulation (excess use of electrocautery has been shown to double infection rates)
What are the steps to wound healing?
- Traumatic inflammation- 1st vasoconstriction for 5-10 minutes, then dehydration of fibrin strands and other blood proteins to form scab which allows epithelial cells to migrate and wound contraction
- Destruction or debridement- about 6 hours in– leukocytes migrate into the wound by diapedesis and breakdown cellular debris, bacteria and foreign material. Then nethrophils to remove extracellular material. Then macrophages– which remove most of the debris and attract fibroblasts by releasing cytokines
- Proliferation (repair)- fibroblast proliferation (after debris has been removed; 4-6 days after injury) and migration, capillary infiltration (4-6 days after injury) ** fibroblasts, glycoproteins, protein polysaccharides, and capillary loops form granulation tissue (more type III collagen– eventually becomes type I– which aids in increasing tensile strength of wound)
- after 3 weeks there is no further increase in the amount of collagen in the wound– in the maturation stage the collagen forms re-organize along lines of stress (strength of the wound remains 15-20% weaker than original tissue)…
Examples of common systemic diseases, conditions, other that would delay wound healing? Why?
* Cushing’s disease, uraemia, disseminated cancer, diabetes, old patients, chronic anaemia (hypoxic tissues), protein deficiency from parasitism, malnutrition, malabsorption, liver disease, drugs (anti-inflammatory drugs, cytotoxic drugs), trauma (surgical), motion, seroma (free fluid in the wound), infection, low temperatures, foreign bodies (can wall off inert materials such as carbon, lead shot but not organic materials such as grass seeds– inflammatory ongoing reaction)
* decreased capacity for fibroplasia and an increased risk of infection, release of endogenous ACTH and cortisol from disease/stress (inhibit early and late phases of wound healing- inflamm, neovascularisation, fibroplasia, collagen formation, wound contraction)
* Heart failure– or other diseases that interfere with peripheral circulation
What are the main types of surgical scissors? What would you never use a blunt-sharp scissor for?
Mayo scissors: Straight or curved, blunt-blunt scissors. Heavy duty scissors used for dissecting and cutting strong tissues such as fascia.
Metzembaum scissors: Usually curved. Similar to mayo scissors but these scissors have shorter blades relative to the handles and a much more delicate action for dissection around delicate tissues.
Iris scissors: Sharp-sharp scissors
Blunt-Sharp scissors : These scissors are robust instruments designed for cutting materials such as excess suture material following suture placement. They are not a tissue scissor.
Wire scissors: These are very strong scissor designed to cut surgical wire with a shearing action.
Bandage scissors: These scissors usually have a protected end on the lower blade to protect the skin during bandage removal.
Suture scissors: alternatively a #12 sterile disposable hook blade may be used.
Curved scissors offer greater mobility and visibility while straight scissors provide greater mechanical advantage
Which causes more trauma- smooth-tipped forceps or forceps like Adson with small teeth or Debakey with fine serrations?
* The greater pressure required to hold smooth-tipped tissue forceps is more traumatic than using tissue forceps with small teeth (Adson) or fine serrations (Debakey)?
What are bonney forceps used for? Potts Smith? Adson forceps or Brown Adson? Russian? Debakey? Dressing forceps?
* Bonney forceps: heavy robust instrument for tissues such as skin or the linea alba (1:2 or 2:3 teeth)
* Potts Smith forceps: Longer, more delicate for delicate tissues such as gut
* Adson forceps (1:2 teeth) or Brown Adson: multiple intermeshed fine teeth– delicate tissue
* Russian forceps: wide tip and deep grooved gripping surface– lung or atrial appendage
* Debakey- cardiovascular or urogenital surgery– adventitia around a blood vessel to aid in dissection– fine serrations or teeth that intermesh
* Dressing forceps: stronger and more robust than tissue forceps– used to hold spnges or gauze – not for tissue as causes injury due to using more pressure to attempt to hold the tissues
What are allis tissue forceps used for? Babcock? Noyes alligator? Doyen?
* Allis tissue forceps- may crush tissue and should be used on connective tissue and fascial planes only; linea alba during an ovariohysterectomy or laparotomy
* Babcock intestinal forceps- less traumatic to the tissues than allis. Fine longitudinal striations. Urinary bladder during cystotomy.
* Noyes alligator forceps: long thin shaft- can enter small openings and are excellent for removing foreign bodies from structures such as the ear canal
* Doyen intestinal forceps: designed to hold intestines without crushing– long thin bowed jaws with tips of the jaws meeting at the same time as the ratchets first teeth engage

What are the different types of haemostatic forceps?
* Halsted mosquito haemostats
* Kelly and crile- more robust

What are these used for?

Rochester Carmalt forceps- clamping vascular pedicles. The grooves run parallel with the long axis of the jaws. They are particularly useful in ligating ovarian and uterine pedicles.
What is the mathieau and gillies pattern?
* Mathieu- needle holder operated by the palm of the hand and therefore suffers in precision and feel for the tissues
* Gillies pattern- large thumb grip set at an angle to the other for use over the thumb. Also has a scissor incorporated into the jaws but does not have a ratchet.

What can be steam sterilized (autoclaved)?
* stainless steel instruments, drapes, gowns, swabs, most rubber articles, glassware and some heat stable plastics
NO endoscopes, lenses and some plastics can be damaged
What is gamma irradiation used for?
* synthetic suture materials, plastic catheters and syringes
** NOT on endoscopes
What do you use Cidex OPA for?
* medium to high level disinfection
* endoscopes– or other lensed instruments
Which are rapidly absorbable suture materials? Medium-term? Longer-term?
* Rapidly absorbable:
- Catgut (chromic catgut 30 days, catgut 15 days), Monocryl (Polyglecaprone) 7-10 days, Vicryl Rapide 5 days, Caprosyn (Polyglytone)
* Medium term:
- Dexon (Polyglycolic acid 14 loss of 35% tensile strength, 21 days 65%), Vicryl (Polyglactin)- similar to Dexon, Polysorb (Braided Lactomer, similar to Vicryl and Dexon), Biosyn (monofilament Glycomer) similar to all of the above
* Longer-term:
- PDS (50% loss of tensile strength in 28 days and 75% in 75 days), Maxon (Polyglyconate- 50% of tensile strength at 28 days, 75% in 42 days)
Non-absorbable suture materials
* Silk (ligating large blood vessels)
* Linen (braided– causes tissue reaction, GIT surgery)
* Polyester (multifilament braided… extremely strong, durable, pliable and easy to handle. Huge tissue reaction)
* Nylon (Polyamide)- monofilament– significant memory makes handling and knot tying difficult
* Caprolactum- twisted multifilament coated material with good handling. Only used in skin.
* Polypropylene- monofilament, vascular surgery
* Polybutester- monofilament, not as stiff as nylon. Good knot security, little packet memory
* Stainless steel- multi or mono, highest tensile strength andg greatest knot security. Essentially inert but poor durability to repeated flexing and may break.
Problems with cyanoacrylates?
Tissue adhesives, cyanoacrylates, not as strong as sutures if used alone. Tissue toxicity and delayed wound healing. They polymerise in the moisture present in a wound with the release of heat.
When is a surgeons knot used? Which has better knot security: multifilamentous or mono, caveat?
* Surgeons knot is used to place a suture in tissues in which the wound edges are under some tension and the first throw wants to slip
* Multifilamentous materials have better know security when compared with monofilaments. But this is significantly reduced by coating and 4-5 throws are frequently required to secure them. Also premature locking is also a problem associated with these sutures.
What should be considered when selecting suture material?
* Initial strength- cannot be stronger than the tissue holding as will tear as well
* Durability- loss of suture strength of absorbable sutures should lag behind the gain of strength of a healing wound
* Tissue reaction
* Biomechanical properties

What is an important consideration to check when seizuring for any amount of time? What control measures?
Temperature! Fans, soak in water, alcohol if not much hair, cool water enema
What is a problem with inducing emesis in a toxicity case?
Increase BP and ICP–> Could exacerbate CNS system issues SO DO NOT DO IF ANIMAL IS not ambulatory or unstable
What will tell you about acute renal failure the fastest?
Urine casts


