Vascular Flashcards
Post-phlebitic limb: chronic venous insuficiency
Examination
(Inspection, palpation, completion, special test)
Inspection
- Venous Infufficiency (HAS LEGS)
- Haemosiderosis; damages capillaries leak blood -> read brown patches
- Atrophie blanch
- Swelling, ankle (chronic v insuff/DVT/HF)
- Lipodermatosclerosis; inflammation of subcutaneous fat-> woody hard skin
- Eczema, venous
- Gaiter ulcers
- Stars, venous
- Varicose veins: Superficial venous dilation and tortuosity.
- Present as collaterals bypassing the obstruction
Palpation: pitting oedema
Completion
- Perthe’s test;
- Tests for deep venous occlusion
- High tourniquet around pts. leg + walking for 5min
- Deep obstruction → swelling and pain
- Abdominal exam + PR
- Pelvic exam in women
Post-phlebitic limb: chronic venous insuficiency
History
Hx
- Previous DVT; Orthopaedic surgery/Complicated obstetric
- Venous Claudication: “Bursting” pain in the leg after exercise, Relieved by rest and elevation of limb (cf. arterial)
Post-phlebitic limb: chronic venous insuficiency
causes
Reflux following DVT: 90%
Obstruction following DVT: 10%
Post-phlebitic limb: chronic venous insuficiency
venous gangerne
(What? 3 phase)
- Rare complication of DVT in the iliofemoral segment
- 3 phases
- Phlegmasia alba dolens: white leg
- Phlegmasia cerulea dolens: blue leg
- Gangrene 2O to acute ischaemia
Post-phlebitic limb: chronic venous insuficiency
Lipodermatosclerosis (viva)
Lipodermatosclerosis
- Panniculitis
- Venous HTN → extravasation of fibrin and red cells
- Poor tissue oxygenation → ulceration and fat necrosis
- Inverted champagne bottle appearance
- Chronic inflam → fibrosis → distal shrinkage
- Venous obstruction → proximal leg swelling
Post-phlebitic limb: chronic venous insuficiency
Ix of Deep Venous Disease
Ix of Deep Venous Disease
- Duplex: reflux and occlusion
- Venography
- Ascending: patency and perforator incompetence
- Descending: reflux
- Ambulatory venous pressures
Post-phlebitic limb: chronic venous insuficiency
Surgical options (reflu/obstruction)
Surgical Options
Reflux
- Trahere Transplantation
- Transplant segment of axillary vein c¯ valve into deep venous system of leg
- Wrap c¯ PTFE cuff
- Kistner Operation
- Valvuloplasty of damaged valves
Obstruction
- Palma operation
- Use contralateral GSV and anastomose to femoral vein to bypass iliofemoral obstruction
Venous
Examination
(inspect, palpate, ausculation, other)
Inspect;
- Scars; esp in groin creases
- skin colour changes
- Venous Infufficiency (HAS LEGS)
- Haemosiderosis; damages capillaries leak blood -> read brown patches
- Atrophie blanch
- Swelling, ankle (chronic v insuff/DVT/HF)
- Lipodermatosclerosis; inflammation of subcutaneous fat-> woody hard skin
- Eczema, venous
- Gaiter ulcers
- Stars, venous
- Varicose veins: Superficial venous dilation and tortuosity
- Distribution;
- medial and above the knee; great saphenous
- Posterior and below the knee; short saphenous
- Few varicosities and prominent skin changes; calf perforators
- Distribution;
- ?Inverted champagne bottle leg
Palpate
- Pitting oedema; if present establish how far oedema extends; also check JVP if oedema is found
- Palpate varicosities
- Tenderness/hardness: thrombophlebitis
- Induration: thrombosis
- Saphena varix @ SFJ
- Two finger breaths below and lateral to pubic tubercle
- Bluish tinge, disappears on lying flat
- May have cough impulse (Cruveihier’s Sign)
- Calf tenderness (DVT)
Percussion (wave of varicosities; tap distally and feel impulse proximally (normal) and tap proximally and feel impulse distally (incompetent valves))
- Tap test (Chevrier’s Test)
- Tap proximally and feel for impulse distally
- Distal pulses: PTA, DPA
Auscultation ; bruit over varicosity; AVM
Other
- Trendelenburg (/tourniquet) test if varicosities present; determines the position of venous regurgitation of varicosities in leg.
- Elevate limb to 15* and note rate of venous emptying
- Position patient supine, Lift pt leg as high as comfortable and milk leg to empty the veins. While elevated place tourniquet/press thumb over saphenofemoral junction (2-3cm below and 2-3cm lateral to pubic tubercle) ask pt to stand while pressure is maintained.
- Controlled: incompetence above tourniquet. Release tourniquet to confirm filling
- Uncontrolled: incompetence below tourniquet e.g. SPJ or calf perforators. Repeat test with tourniquet just below knee
- Examine the abdomen and perform a PR
- Pelvis examination in females
- Pulses (arterial)
- Doppler; Place probe @ SFJ/SPJ and squeeze calf. Normally hear only half second whoosh when pressure released. Long whoosh suggests valve incompetence.
Varicose veins
presentation
presentation: Abnormal, Tortuous, dilated veins of the superficial venous system. clearly in the distribution of the LSV in the medial side of the thigh and calve. These can be primary: which 99% are, which replies a failure of the valves and reflux down the superficial venous system. They can be secondary; as a result of blockage in the deep viens and increased pressure on the venous system higher up.
Varicose veins
symptoms and complications
Symptoms:
- Cosmetic defect
- Pain, cramping, heaviness
- Tingling
- Bleeding: may be severe
- Swelling
Complications;
- Swelling and oedema
- Thrombophlebitis
- Bleeding
- Varicose eczema
- Haemosidering deposition-> lipodermatosclerosis (woody, champagne bottle)-> venous ulceration
Varicose veins Investigations
Duplex US
- Indications
- Previous Hx of DVT
- Signs of chronic venous insufficiencyl Suggests deep venous disease for which the varicosity may be the collateral.
- Recurrent varicose veins
- Difficulty in deciding whether GSV or SSV is incompetent
Preparation for Surgery
- FBC, U+E, clotting, G+S
- CXR
- ECG
Varicose veins classifications
CEAP Classification, Classification of Chronic Venous Disease
- Clinical signs (1-6 + sympto or asympto)
- Etiology
- Anatomy
- Pathophysiology
Varicose veins management
Conservative
- Lose wt. and regular exercise
- Avoid prolonged standing
- Class II graduated Compression Stockings; 18-24mmHg
- Skin care: emollients
Minimally Invasive Therapies (Indications; Small below knee varicosities not involving GSV or SSV)
- Techniques
- Local or GA
- Injection sclerotherapy: 1% Na tetradecyl sulphate
- Endovenous laser or radiofrequency ablation
- Post-Operatively
- Compression bandage for 24hrs
- Compression stockings for 1mo
Surgery (Indications; SFJ incompetence//Major perforator incompetence// Symptomatic: ulceration, skin changes, pain)
- Procedures
- Trendelenberg: saphenofemoral ligation
- SSV ligation: in the popliteal fossa
- LSV stripping: no longer performed due to potential for saphenous nerve damage.
- Multiple Avulsions
- Cockett’s Operation: perforator ligation
- SEPS: Subfascial Endoscopic Perforator Surgery
- Post-op
- Bandage tightly and elevate for 24h
- D/C c¯ compression stockings and told to walk daily.
- Complications:
- Early
- Haematoma: esp. groin
- Wound sepsis
- Nerve damage: e.g. long saphenous
- Late
- Superficial thrombophlebitis
- DVT
- Recurrence: 10% @ 5yrs
Varicose veins
pathophysiology
- One-way flow from sup → deep maintained by valves
- Valve failure → ↑ pressure in sup veins → varicosity
- Fibrous tissue invades tunica intima and media, breaking up the SM
- Prevents maintenance of vascular tone → dilatation
- 3 main sites where valve incompetence occurs
- SFJ: 3cm below and 3cm lateral to pubic tubercle
- SPJ: popliteal fossa
- Perforators: draining GSV
- Chronic venous insufficiency is distinct and results from incompetency in the deep system itself.
- May co-exist c¯ varicose veins
Varicose veins
causes
- Primary / Idiopathic: 95%
- Prolonged standing
- Pregnancy
- Obesity
- OCP
- Secondary: 5%
- Valve destruction: DVT, thrombophlebitis
- Obstruction: pelvic mass, DVT
- AVM
- Syndromes
- Klippel-Trenaunay-Weber
- Abnormality of the deep venous system
- Varicose veins
- Port wine stain
- Bony and soft tissue hypertrophy of the limbs
- Parkes-Weber Syndrome
- Multiple AVMs c¯ limb hypertrophy
- AVMs can → high-output HF
- Klippel-Trenaunay-Weber
Lymphoedema
Examination
(inspect, palpate, complete)
Inspection
- Gross leg swelling
- Bilateral or unilateral
- Thick, indurated skin
- Lichenification
- Yellow nail discoloration
Palpation
- Initially: pitting
- Later: non-pitting
- Palpate for inguinal nodes
Completion
- Exclude RHF: ↑ JVP, Hepatomegaly
- Take a Hx: esp. re hereditary conditions
Lymphoedema
vival
DDiagnosis; bilateral and unilateral limb swelling
Bilateral
- ↑ Venous Pressure
- RHF
- Venous insufficiency
- Drugs: e.g. nifedipine
- ↓ Oncotic Pressure
- Nephrotic syndrome
- Hepatic failure
- Protein losing enteropathy
- Lymphoedema
- Myxoedema; Hyper- / hypo-thyroidism
Unilateral
- Venous insufficiency
- DVT
- Infection or inflammation
- Lymphoedema
Lymphodema
define
Pimary and secondary causes
Define: Collection of interstitial fluid due to blockage or absence of lymphatics.
Primary; Congenital absence of lymphatics. May or may not be familial. Presentation:
- Congenital: evident from birth.
- Praecox: after birth but < 35yrs
- Tarda>35 yrs
- Milroy’s Syndrome: 2% of primary lymphoedema. Familial AD subtype of congenital lymphoedema F>M
Secondary: FIIT
- Fibrosis: e.g. post-radiotherapy
- Infiltration
- Ca: prostate, lymphoma
- Filariasis: Wuchereria bancrofti
- Infection: TB
- Trauma: block dissection of lymphatics
Lymphoedema
Viva; Management
(conservative, physio, surgical)
Conservative
- Skin care
- Grade 3 compression stockings
- Treat or prevent cellulitis
Physio
- Raise leg as much as possible
Surgical
- Debulking operation
- Bypass procedures
Peripheral Ulcer Examination
Inspect, palpate, complete
Inspection: BEDS
- 3s: Site, Size, Shape
- Base:
- Granulation tissue
- Slough
- Floor: bone, tendon, fascia
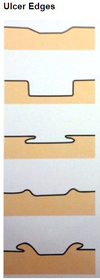
- Edge:
- Sloping: healing – usually venous
- Punched-out: ischaemic or neuropathic
- Undermined: pressure necrosis or TB
- Rolled: BCC
- Everted: SCC
- Discharge: Serous, Purulent, Sanguinous
- Surroundings: Cellulitis, Excoriations, Sensate, LNs
Palpation
- Limb pulses
- Sensation around the ulcer
Completion
- Examine contralateral side
- Distal neurovascular examination
- ABPI: must be >0.8 for compression bandaging
Causes of PEripheral ulcer
Causes;
Venous: 75% + Arterial: 2% + Mixed arteriovenous: 15% + Neuropathic
Other: Pressure, Vasculitis: e.g. PAN, Malignancy: SCC, Marjolin’s, Systemic: pyoderma gangrenosum
Venous ulcer
Findings on Examination
(inspect/palpate)
Inspection Site: medial malleolus, Size: variable, can be v. large, Base: Shallow and Pink granulation tissue, Edge: sloping edge, Discharge: seropurulent Surroundings: Signs of chronic venous insufficiency: HAS LEGS and Varicose veins
Palpation Painless, Warm surroundings, Sensate
Venous ulcer
viva causes
Valvular disease Varicose veins Deep vein reflux: e.g. post DVT Outflow obstruction (Often post DVT) Muscle pump failure Stroke Neuromuscular disease
Venous ulcer
Investigations
ABPI if possible
Duplex ultrasonography
Biopsy may be necessary: esp. if persistent ulcer
Look for malignant change: Marjolin’s ulcer
Venous Ulcer mangagement
(general, compression, other)
Refer to leg ulcer community clinic
General Measures
- Optimise risk factors: nutrition, smoking
- Analgesia
- Bed rest + elevate leg
4 layer compression bandaging if ABPI >0.8
- Construction
- Non-adherent dressing + wool bandage
- Crepe bandage
- Blue line bandage: light compression
- Cohesive compression bandage
- Change bandages 1-2 x/wk
- Once healed use grade 2 compression stockings for life
Other Options
- Pentoxyfylline PO: ↑ microcirculatory blood flow
- Desloughing c¯ larval therapy
- Topical antiseptics: Manuka honey
- Surgical: split-thickness skin grafts
Ischaemic Ulcer
Examination
Inspection/palpation
Inspection
- Site; Tips of and between toes, Base of 1st and 5th metatarsals, Heel
- Size: mm-cm
- Base; Deep: may be down to bone, May be slough but no granulation tissue
- Edge: punched-out
- Surroundings; Pale, Trophic changes
Palpation; Painful, Cold surroundings, Sensate, Reduced or absent distal pulses
Causes of Ischaemic ulcer
(large/small)
Large Vessel; Atherosclerosis, Thombangiitis obliterans (Buerger’s Disease)
Small Vessel; DM, PAN, RA
MAnagement of ischaemic ulcer
Analgesia, RF modification, medical
Analgesia:
- Can be extremely painful-> Combination of drugs administered regularly
- Based on the analgesic ladder: titrate to pain
- Paracetamol + NSAIDs
- Weak opioids: e.g. codeine
- Strong opioids: e.g. morphine
Risk Factor Modification; Stop smoking + Control DM and HTN + Optimise lipids
Medical
- Avoid drugs which may worsen symptoms: e.g. β-B
- Low-dose aspirin
- IV prostaglandins
- Chemical lumbar sympathectomy: Chemical ablation of L1-L4 paravertebral ganglia, Inhibit sympathetic-mediated vasoconstriction, Relief of pain, Often unsuccessful in DM: neuropathy
Neuropathic Ulcer Examination
Inspection, extras, palpation, completion
Inspection
- Site: pressure areas: Tips of and between toes, Base of 1st and 5th metatarsals, Heel
- Size: variable
- Shape: corresponds to shape of pressure point
- Base: may be deep c¯ bone exposure
- Edge: punched-out
- Surroundings; Skin looks normal, Charcot’s joints, May be signs of PVD if co-existent arterial disease
Extras
- Blood sugar testing marks on fingers
- Insulin injection marks on the abdomen
Palpation;
- Normal temperature
- Normal peripheral pulses
- Absent sensation around ulcer
- Absent ankle jerks
Completion
- Full peripheral vascular exam
- Cranial and peripheral neuro exam
NEuropathic ulcer causes
Any cause of peripheral neuropathy
DM Alcohol B12 CRF Drugs: e.g. isoniazid, vincristine Every vasculitis
Pathophysiology of neuropathic ulcer (sensory, motor, autonomic)
Sensory neuropathy: distal limb damage not felt by pt.
Motor neuropathy: wasting of intrinsic foot muscles and an altered foot shape e.g. Claw toes + prominent metatarsal heads
Autonomic neuropathy: ↓ sweating → cracked, dry foot
Thoracic Outlet Obstruction Examination
Inspection, palpation
Inspection
- Arm: ↓ venous outflow
- Oedema: pitting
- Cyanosis
- Pallor
- Hand: ↓ arterial inflow
- Raynaud’s
- Patchy gangrene
- Fingertip necrosis
- Hand and Arm: neurological complications
- Complete claw hand
- T1 sensory loss
- Radicular pain
Palpation
- Palpate for cervical rib above the supraclavicular fossa
- Disappearance of radial pulse on abduction and external rotation of arm
Differential of Thoracic Outlet Obstruction
- Arterial: Raynaud’s
- Venous: axillary vein thrombosis or trauma
- Neurological: cervical spondylosis, Pancoast’s tumour
Ix of TOS
- X-Ray: cervical rib
- Duplex in abduction
- Arteriograms of subclavian artery may show kinking
- Nerve conduction studies
Aetiology of thoracic outlet syndrome
- Congenital: cervical rib
- Acquired: clavicle #, pathological enlargement of 1st rib
Management of thoracic outlet syndrome
?first rib/cervical rib excision
Raynaud’s Phenomenon
Examination ( Key Questions, inspection, palpation, completion)
Key Questions
- What is the main problem you have c¯ your hands?
- When do symptoms occur?
- Is it precipitated by any specific weather conditions?
- Can you describe the colour changes your fingers go through?
Inspection
- Usually bilateral
- Dry, red skin
- Brittle nails
- Ulceration or gangrene on the pulps
Palpation; Normal radial pulse
Completion; Ask about symptoms and look for signs of secondary causes of Raynaud’s phenomenon
Raynaud’s phenomenon
definition, pathogenesis, 2ndary causes
Definitions
Phenomenon: characteristic cold-induced changes assoc. c¯ vasospasm
Disease: primary Raynaud’s phenomenon occurring in isolation
Syndrome: secondary Raynaud’s phenomenon assoc. ¯c other disease
Colour Changes (Cold- or emotion-induced) = White → Blue → Crimson
Pathogenesis; Overactive α sympathetic receptors Or, fixed obstruction in vessel wall
Secondary Causes: BADCAT Blood: polycythaemia, cryoglobulinemia, cold agglutinin Arterial: atherosclerosis, thrombangiitis obliterans Drugs: β-B, OCP, ergotamine Cervical rib: → thoracic outlet obstruction Autoimmune: SLE, RA, SS Trauma: vibration injury
Raynaud’s syndrome
Management
(conservative, medical, surgical)
Mx
- Conservative; wear gloves and avoid cold + Stop smoking
- Medical; CCBs: e.g. nifedipine + IV prostacyclin
- Surgical ; Cervical sympathectomy + amputate gangrenous digits
Gangrene
Examination (Inspection , palpatation)
Inspection
Wet; Putrefaction + Ill-defined, spreading edge
Dry; Dry and shrunken + Well demarcated + Features of PVD
Palpation = Temperature + Distal pulses
Gangrene
Definition, classification, causes, management
Definition; Irreversible tissue death from poor vascular supply.
Classification
- Wet: tissue death + infection
- Dry: tissue death only
- Pregangrene: tissue on the brink of gangrene
Causes of Gangrene
- DM: commonest
- Embolism and thrombosis E.g. foot trash in AAA repair
- Raynaud’s
- Thrombangiitis obliterans
- Injury: extreme cold, heat, trauma or pressure
Mx
- Take cultures
- Debridement (including amputation)
- Benzylpenicillin ± clindamycin
Synergistic Gangrene
- Involves aerobes + anaerobes
- Fournier’s: perineum
- Meleney’s: post-op ulceration
- Both progress rapidly to necrotizing fasciitis and myositis
Gas Gangrene
What?/RF/Presentation/treatment
Clostridium perfringes myositis
RFs: DM, trauma, malignancy
Presentation
- Toxaemia
- Crepitus from surgical emphysema
- Bubbly brown pus
Rx
- Debridement (may need amputation)
- Benzylpenicillin + metronidazole
- Hyperbaric O2
Vascular Effects of the Diabetic Foot
Examination
(inspection, palpatation, completion)
Inspection
- Bilateral signs of chronic arterial disease
- Amputations: esp. digits
- Charcot joints
- Ulceration
Palpation
- Pulses may be preserved due to calcification
- ↓ sensation in stocking distribution
Completion
- Examine the peripheral nervous system
- Urinalysis: proteinuria
- Fundoscopy: retinopathy
Vascular Effects of the Diabetic Foot
viva History, diabetic foot syndrome, aetiology of diabetic ulcer
Hx; Control, Complications, Claudication, Previous operations, Other vascular disease, Other vascular risk factors
Diabetic Foot Syndrome
- Microvascular disease
- Macrovascular disease; Predominantly below knee cf. non-DM occlusive disease.
- Neuropathy
- Infection and osteomyelitis
Aetiology of Diabetic Ulcers; Neuropathic: 45-60% + Ischaemic: 10% + Mixed neuroischaemic: 25-45%
- Preservation of Pulses;* Calcification in the walls of the vessels: mediasclerosis -> Preserves the pulses until late → abnormally high ABPI –> Use toe pressure instead: <30mmHg Similar effect is seen in CRF
- Problems c¯ Diabetics Undergoing Angiography ;* Often have a degree of renal impairment which can be dramatically worsened c¯ contrast agents. + Metformin must be stopped prior to the procedure to prevent lactic acidosis
Carotid artery disease
either
C endartectomy scar
or
Carotid buits (+completion)
Carotid Endarterectomy Scar: Beneath the angle of the mandible + Parallel to SCM
Carotid Bruit : Along course of common carotid: medial to SCM in the anterior triangle + Best heard in expiration
Completion;
- If heard bilaterally, listen over precordium to exclude AS
- Full peripheral vascular examination
- Neurological examination: cerebrovascular event
Carotid artery disease
History
Investigations (bedside, blood, imaging)
Hx; Previous TIA: esp. amaurosis fugax (Amaurosis fugax will be ipsilateral to stenosis), Previous stroke, Other CV and PV disease, CV risk factors
Ix
Bedside:
- Urine dip: proteinuria in renovascular disease
- ECG: ischaemic changes, AF
Blood
- FBC: anaemia may worsen symptoms
- U+E: renovascular disease
- Glucose: DM
- Lipids: hypercholesterolaemia
Imaging
- Carotid Duplex US: site and size of stenosis
- MRA: more detailed carotid anatomy
- Echo: CVD
- CT or MRI brain: infarcts
Carotid atery disease
Complications
TIA; Sudden neurological deficit of vascular origin lasting <24h (usually lasts <1h) c¯ complete recovery. Microemboli from the plaque
Stroke: Sudden neuro deficit of vascular origin lasting >24h. 3rd leading cause of death in the West. Carotid atheroembolism is the commonest cause
Carotid artery disease
management
(conservative, surgical+compl)
Mx
Pts c¯ severe symptomatic stenosis should have CE ASAP after the neurological event.
Conservative
- Aspirin or clopidogrel
- Control risk factors
Surgical: Endarterectomy
- Symptomatic (ECST, NASCET)
- ≥70% (5% stroke risk per yr)
- ≥50% if low risk (<3%, typically <75yrs)
- 6 fold reduction in stroke rate @ 3yrs
- Asymptomatic (ACAS, ACST)
- ≥60% benefit if low risk
Complications:
- 3% risk of stroke or death
- Haematoma
- MI
- Nerve injury; Hypoglossal: ipsilateral tongue deviation, Great auricular: numb ear lobe, Recurrent laryngeal: hoarse voice, bovine cough
Amputations Examination
Inspection
Palpatation
move
completion
Inspection
- Stump anatomical level
- Stump health
- Evidence of chronic vascular disease
Palpation
- Soft tissue under skin should move freely over the bone
- Proximal pulses
Move
- Ask pt. to actively flex and extend the knee joint above the amputation
- Many pts. have a fixed flexion deformity after BKA
- Ask to look @ prosthesis and see pt. walk c¯ it.
Completion
- Examine other limb for signs of PVD
Amputations Viva Indications
4D’s
Dead: PVD (90%), thrombangiitis obliterans Dangerous: sepsis, malignancy Damaged: trauma, burns, frostbite Damned nuisance: pain, neurological damage
Amputations viva considerations and procedures (+ comp)
Consideration
- Psychosocial implications
- Future mobility: 200% more effort to walk after AKA
- OT involvement
- Level of amputation must be high enough to ensure healing of the stump.
- But ↑ mortality c¯ AKA vs. BKA
Procedures
- Toe: with the metatarsal head
- Ray Amputation
- Incision on either side of affected digit to the base of the metatarsal
- Creates a V shape and narrows foot
- Heals by 2 intention
- Used if necrosis of digit and muscles of the foot.
- Forefoot: transmetatarsal
- Below knee: aids rehabilitation
- Above knee
- Hindquarter / hemipelvicotomy
Complications
- Pts. often have co-morbidities → ↑ risk
- Esp. CVD
- Early
- Mortality: ~20% for AK
- Haemorrhage
- Infection: cellulitis, gangrene, osteomyelitis
- Scar contractures → fixed flexion
- Phantom limb pain: try gabapentin
- Poor stump shape inhibiting prosthesis
False Aneurysm Examination
(inspection, palpation, ausculation)
Inspection
- Pulsatile mass in the groin
- Surgical scars or puncture sites
Palpation
- Pulsatile, expansile swelling
- Define the anatomical location
- Usually mid-inguinal point
- Palpate distal pulses
Auscultate for a Bruit
False aneurysm viva
True vs. False Aneurysm
Aneurysm is an abnormal dilatation of a blood vessel
True: involves all layers of arterial wall
False: Collection of blood around a vessel wall that communicates c¯ the lumen - i.e. a pulsating haematoma. Fibrous tissue forms around haematoma → false sac which communicated c¯ vessel lumen
False aneurysm viva aetiology
Aetiology:
- Occurs after vessel a laceration / puncture
- Traumatic or iatrogenic
- Usually in the common femoral A. following puncture for a radiological procedure.
False aneurysm viva Management
- Ultrasound compression
- Thrombin injection
- Surgical repair
Aneurysms: Key Facts
Definition and classification
Definition; Abnormal dilatation of a blood vessel > 50% of its normal diameter.
Classification
-
True Aneurysm: Dilatation of a blood vessel involving all layers of the wall and is >50% of its normal diameter.
- Two different morphologies
- Fusiform: e.g AAA
- Saccular: e.g Berry aneurysm
- Two different morphologies
-
False Aneurysm: Collection of blood around a vessel wall that communicates c¯ the vessel lumen.
- Usually iatrogenic: puncture, cannulation
- Dissection : Vessel dilatation caused by blood splaying apart the media to form a channel w/i the vessel wall. Used to be classified as “dissecting aneurysms” but not technically correct as represents a different pathology
Aneurysm viva
causes
Causes
Congenital:
- ADPKD → Berry aneurysms
- Marfan’s, Ehlers Danlos
Acquired
- Atherosclerosis
- Trauma: e.g penetrating trauma
- Inflammatory: Takayasu’s aortitis, HSP
- Infection
- Mycotic: SBE
- Tertiary syphilis (esp. thoracic)
- Salmonella typhi: assoc. c¯ AAA
Aneurysm complications
- Rupture
- Thrombosis
- Distal embolisation
- Pressure: DVT, oesophagus, nutcracker syndrome
- Fistula: IVC, intestine
Aneurysm viva trial and screening
UK Small Aneurysms Trial Powell, Greenhalgh et al., Lancet 1996
- Asymptomatic aneurysms between 4-5.5cm should be monitored.
- Aneurysms ≥ 5.5cm should undergo repair.
- Risk of rupture
- <5.5cm: 1% /yr
- ≥5.5cm: 10% /yr
Screening
- MASS trial revealed 50% ↓ aneurysm-related mortality in males aged 65-74 screened c¯ US.
- UK men offered one-time US screen @ 65yrs
Popliteal Aneurysm Examination
(inspection, palpation, completion)
Inspection
- Pulsatile popliteal swelling
- Ischaemic patches on foot: emboli
Palpation
- If asked just to examine the pulses, start c¯ femorals
- Comment on presence and character
- Aneurysmal popliteals are very easily palpable
- Popliteal aneurysm ≥2cm in diameter
- 50% bilateral: examine the other knee
- Distal pulses may not be palpable
Completion
- Complete peripheral vascular examination
- Abdominal examination for AAA
- Present in 50%
Popliteal aneurysm
Viva Presentation
- Popliteal aneurysms represent 80% of all non-aortic aneurysms
- Lump behind the knee
- 50% present c¯ distal limb ischaemia: thromboembolism
- <10% rupture
Popliteal aneurysm
management
surgical indications, acute, stable
Surgical Indications
- Symptomatic aneurysms
- Aneurysms containing thrombus
- Aneurysms >2cm
- *Mx**
- Acute*: embolectomy or fem-distal bypass
- Stable*: excision bypass
Abdominal Aortic Aneurysm Examination
(inseection, palpation, auscultation, completion)
Inspection
- Midline pulsating mass: esp. on deep inspiration
- Abdominal scars
Palpation
- Pulsatile and expasile mass on deep palpation in theepigastrium.
- Expansile: moves fingers laterally c¯ each pulse
- Estimate size using lateral margins of index fingers
- Palpate for other aneurysms
- Course of common iliacs
- Femorals
- Popliteals
Auscultation for Bruits
- Aortic
- Renal
- Iliac
Completion
- Cardiovascular system
- Peripheral vascular system
AAA viva History
- Presentation: usually incidental finding
- Symptoms
- Abdominal or back pain
- Tenderness over aneurysm
- complications
- Distal embolic events
- Leak
- Risk
- Other peripheral or cardio-vascular disease
- CV risk factors
AAA
definition and RF
Definition
Abnormal dilatation of the abdominal aorta to >50% of its normal diameter = ≥3cm
Risk Factors
- Male
- Age >60yrs (prevalence: ~5%)
- Smoking
- HTN
- FHx
AAA
investigations
- Abdo US: used for surveillance and screening
- CT/MRI: Ix of choice
- Angio: useful to delineate relationship of renal arteries
AAA operation
Indications, complications, operative mortality, EVAR
When to Operate
Repair aims to avoid complications
Operate when risk of complications, esp. rupture, > risk of surgery.
Indications
- Symptomatic aneurysms
- Asymptomatic
- ≥5.5cm
- Expanding >1cm/yr
Complications
- Death
- MI
- Renal failure
- Spinal or mesenteric ischaemia
- Distal trash from thromboembolism
- Anastomotic leak
- Graft infection
- Aortoenteric fistula
Operative Mortality
- Open
- Emergency: 50%
- But only 50% reach hospital alive
- Elective: 5% (lower in specialist centres)
- ↑ if IHD, LVF, CRF, COPD
- EVAR: 1%
EVAR
- ↓ perioperative mortality (1% vs. 5%)
- No mortality benefit after 5yrs
- Significant late complications: e.g. endoleaks
- EVAR not better cf. medical care in unfit pts.
Chronic Limb Ischaemia
Intermittent claudication, critical limb ischaemia, leriche syndrome
Intermittent Claudication
- Cramping pain after walking a fixed distance
- Pain rapidly relieved by rest
- Calf pain = superficial femoral disease (commonest)
- Buttock pain = iliac disease: internal or common
Critical Limb Ischaemia: Fontaine 3 or 4
- Ankle artery pressure <50mmHg (toe <30mmHg)
- And either:
- Persistent rest pain requiring analgesia for ≥2wks
- Especially @ night
- Usually felt in the foot
- Pt. hangs foot out of bed
- Due to ↓ CO and loss of gravity help
- Tissue loss: ulceration, gangrene
- Persistent rest pain requiring analgesia for ≥2wks
Leriche’s Syndrome: Aortoiliac Occlusive Disease
Atherosclerotic occlusion of abdominal aorta and iliacs
Triad of:
- Buttock claudication and wasting
- Erectile dysfunction
- Absent femoral pulses
Differentiate Intermittent Claudication vs. Spinal Claudication

Chronic limb ischaemia
RF
Modifiable
- Smoking
- BP
- DM control
- Hyperlipidaemia
- ↓ exercise
Non-modifiable
- FHx
- PMH
- Male
- ↑ age
- Ethnicity
Chronic limb ischaemia classification

Chronic limb iachaemia investigation
Bedside
- ABPI ± exercise ABPI (↓ by 0.2 in PVD)
- ECG
Blood
- FBC: anaemia may worsen symptoms
- U+E: renovascular disease
- Glucose: DM
- Lipids: hypercholesterolaemia
Imaging: assess site, extent and distal run-off
- Colour duplex US
- CT / MR angiogram: gadolinium contrast
- Digital subtraction angiography
- Invasive -> not commonly used for Dx only.
- Used for therapeutic angioplasty or stenting
Chronic Limb ischaemia Management
Non-surgical / surgical
Non-Surgical Mx
- Walk through pain: may use exercise programs
- Optimise risk factor profile
- Smoking cessation
- Control HTN, lipids and BP
- Lose wt.
- Antiplatelet and statin for all pts.
- Foot care
Prognosis
- ~80% improve or stay the same
- 20% deteriorate, 1% lose their limb
- 60% mortality @ 5yrs: cardiovascular disease
Interventional
- Angioplasty ± stenting
- Chemical sympathectomy
Surgical Mx
- Endarterectomy
- Bypass grafting
- Amputation
- *Bypass Grafting**
- *Indications**
- V. short claudication distance (e.g. <100m)
- Symptoms greatly affecting pts. QoL
- Development of rest pain
- *Pre-op Assessment** Need good optimisation as likely to have cardiorespiratory co-morbidities.
- *Practicalities**
- Need good proximal supply and distal run-off
- Saphenous vein grafts preferred below the IL
- More distal grafts have ↑ rates of thrombosis
Classification
- Anatomical: fem-pop, fem-distal, aortobifemoral
- Extra-anatomical: axillo-fem / -bifem, fem-fem crossover
Upper Limb
Inspection, palpation, auscultation, completion

Lower Limb
inspection, palpation, auscultation,buergers,completion

LL superficial venous drainage anatomy

Lower limb deep and superficial venous anatomy

Present

presentation: Abnormal, Tortuous, dilated veins of the superficial venous system. clearly in the distribution of the LSV in the medial side of the thigh and calve. These can be primary: which 99% are, which replies a failure of the valves and reflux down the superficial venous system. They can be secondary; as a result of blockage in the deep viens and increased pressure on the venous system higher up.









palpate graft across pubic symphysis (reinforcement rings?) ?bilateral femoral pulses distal to the graft=working




LEFT: Long saphenous vein harvest; (+ stenotomy scar=CABG), arteria graft in the leg (+ scar over femoral artery=Femer-O-popliteal bypass/distal) pulse over scar=in situ graft // RIGHT: PTFE prosthetic material, scar at access site/terminal site. Access popliteal artery from medial above the knee or below the knee (NOT THE BACK)

extra anatomically tunnelling (fem-anterior tivia)
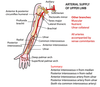
arterial supply of the upper limb (anatomy)
Thoracic aorta anatomy

External iliac artery anatomy (coeliac trunk to ext iliac)

Lower limb arterial supply anatomy

position of anterior tibial pulse

Arterial anomalies
- Dominant peroneal artery; Reported to be present in 5% of the population, there is absent dorsalis pedis pulse on examination and a pulse just anterior to the lateral malleolus as the foot is supplied by branches of the peroneal vessel
- Persistent sciatic artery; Rare condition , characterised by a persistent sciatic arterial supply to the lower limb and absence of femoral vessels. May present with claudication

transmetatarsal amputation

- Charcot joints; painless but hugely deformed joint abnormality

raynaud’s phenomenon

Venous malformations:
- Bluish
- Often raised
- Painful sometimes
- By far the most common
- Not pulsatile
- No Bruit
- No signal with hand held Doppler
- No cardiac compromise

Arteriovenous malformations; like a fistula
- Rare
- Pulsatile dilated veins
- Bruit
- Obvious signal on hand held Doppler
- May be overgrowth of limb (or steal and no growth)
- May be significant shunt and Cardiac failure; high output cardiac failure due to shunt

lymphoedema
- PRIMARY
- SECONDARY
- COMMONEST WORLDWIDE IS FILARIASIS
- COMMONEST IN UK IS IATROGENIC
- CANCER
- OTHER INFECTIOUS CAUSES