Treatment of Infections Flashcards
Superficial fungal infections usually give rise to what infections?
Tineas infections
Such as athletes foot (tinea pedis) and ringworm of the scalp (tinea capitis)
What is a carbapenem?
An inhibitor of cell wall synthesis
These are highly resistant to B-lactamases, and have a very broad spectrum of activity, including anaerobes
These are last resort!!

How do Azoles and Triazole (like Fluconazole and Itraconazole) work?
Block lanosterol 14(a)-demethylase
Which prevents ergosterol biosynthesis
What are the 2 major proteins that are in HIVs envelope?
gp120
gp41
What is the HAART therapy?
Highly Active Anti-Retroviral Therapy
Taking 3 different anti-retroviral drugs, with at least 2 different classes
This decreases the chance of resistance build up

What type of drug can be depositied into the teeth and bone of growing children/foetus?
Tetracyclines such as doxycycline
How do Polyenes (Nystatin and Amphotericin B) work?
Target ergosterol –> increasing membrane permeability
Are fungi eukaryotic or prokaryotic?
Eukaryotic
How do tetracyclines like doxycycline work?
How does resistance occur?
Bind reversibly to the A site on the 16rRNA unit. This interferes with translocation in the tRNA (A –> P)
Their effects are bacteristatic, and they have a great level of selective
The induction of efflux pumps…..
Intrinsic - The basal activity of the pumps
Acquired - The upregulation in the presence of the antibiotic

How do Allyamines and Thiocarbamates (like Terbinafine) work?
They block squalene epoxidase
And so prevents ergosterol biosynthesis
Explain the differences between a isomotic, hyper/hypo osmotic solutions
Isomotic - Where the osmolality of the solution is equal to that of the intracellular fluid
Hyper-osmotic - When the osmolality of the solution if greater than that of the intracellular fluid (so movement out)
Hypo-osmotic - When the osmolality of the solution if less than that of the intracellular fluid (so movement in)

What are NNRTIs, and how do they work?
Non-Nucleoside Reverse Transcriptase Inhibitors
These inhibit DNA replication by binding to the allosteric site of reverse transcriptase, causing a conformational change

How does the Varicella-Zoster Virus (VZV) work?
It gains entry via the respiratory tract, and moves through the lymph to the skin (its target organ) after 14 days incubation
This can stay latent after the initial infection in the cerebral/posterior root ganglia. Later on it can then move down a sensroy nerve and back to the skin
What is the difference with Endotoxin, and exotoxins?
Endotoxin - A structual feature of lipopolysaccharides
Exotoxins - These are toxins that are actively secreted during normal growth
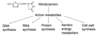
How do Echinocandins (Caspofungin and Micafungin) work?
Block 1,3-(B)-D-glucan synthase
Which in turn prevents cell-wall biosynthesis
How does Nitrofuratonin work?
It is broken down into many different active metabolites
Broad spectrum of activity
Cannot be used on people with urinary cathaters, due to drug accumulation in the bladder
How do glycopeptides such as Vancomycin work?
And how does resistance build up?
These bind to the d-ala - d-ala on the peptide side chain of the peptidoglycan monomer, preventing this from being added to the peptidoglycan chain
Only work against gram positive bacteria
There is an alteration in the terminal AA of the peptide chain, reducing hydrogen bonding, and so prevents stable binding of vancomycin

What is the difference between osmolarity and osmolality?
Osmolarity - The number of osmoles (particles) per litre of solution
Osmolality - The number of osmoles (particles) per Kg of solvent (eg, water)
How does HIV enter the cell?
HIV approaches a CD4(+) T-cell
Their gp41 and gp120 proteins vind to the CD4 and chemokine receptors
Binding of co-receptors causes a conformational change in gp120, exposing gp41 which has two domains (HR1 and HR2)
Zipping occurs, which is where HR2 coils into the grooves that have been exposed on HR1
This punches a hole in the membrane, allowing the HIV capsid to pass through the cell membrane

Explain the 2 different types of acquired resistance with respect to antibiotics
Genetic - This is irreversible, and comes about due to mutations or plasmids
Phenotypic - This is reversible, eg, E.coli is more resistant to antibiotics in a biofilm than on its own
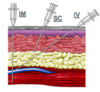
What are the 3 routes of parenteal administration?
Intravenous - Into a large proximal vein
Intramuscular - Small amount of liquid into the muscle
Subcutaneous - Liquid added to the subcutaneous tissue
Describe the different herpes viruses
HSV1 - Oropharyngeal Sores in children, usually spread from kissing
HSV2 - Genital infections that are common in young adults, which can increase the chance of HIV infection
Both are part of the alpha sub-family of herpes, are enveloped, and have DS DNA

How do macrolides, like erythromycin and clarithromycin, work?
Bind to the 23S rRNA in the 50S subunit, inhibiting translocation
Mainly used in the treatment of gram-positive bacteria
Used for strep infections when penicillin allergies are present

Explain Vapour Point Depression
Boiling point elevation and Freezing point depression
Vapour Point Depression - Where the addition of a non-volatile solute to the solvent will decrease the vapour pressure…..so less moleucle will evaporate
Boiling Point Elevation - The dissolution of a non-volatile solute in a solvent will increase the boiling point
Freezing Point Depresson - The dossolution of a non-volatile solute in a solvent will decrease the freezing point