The uterus and its abnormalities Flashcards
Anatomy and function of the uterus
blood supply and lymph
endometrium
uterosacral and cardinal ligaments support inferior end of uterus at the cervix
endometrium (glandular) -> myometrium (smooth muscle) -> serosa (peritoneum posteriorly)
uterine arteries cross over ureter lateral to servix and pass inferiorly and superiorly, supplying myometrium and endometrium
at cornu arterial anastomosis with the overian blood supply, inferiorly anasotmosis with vessels of upper vagina
lymph drainage of uterus mostly via internal and external iliac nodes
endometrium
- supplied by spiral (menstruation and nourishment of growing fetus) and basal arterioles
- responsive to P+O
- 14 days of menstrual cycle = proliferates, glands elongate and endometrium thickens under oestrogen influence (proliferative)
- after ovulation = glands swell and blood supply increases under progesterone influence (luteal/secretory phase)
- progesterone levels drop, secretory endometrium disintegrates as blood supply can no longer support it and menstruation occurs
- poor homronal control commonly causes errativc bleeding patterns
*

Fibroids (leiomyomata): definition and epidemiology
size and sites
benign tumours of myometrium
common with increasing age during reproductive years (more in black, asian, obese, early menarche, affected first degree relative women), less common in parous women and those taking COCP/injectable progestogens
single/mulitple, few millimetres/massive tumours filling abdomen, intramural/subserosal/submuscosal/intracavitu
‘whorled’ appearance in transverse section

Fibroids: aetiology
growth is P+O dependent
pregnancy = grow/shrink/no change
regress after menopause due to reduction in circulating sex hormones
monoclonal origin
fibroids: clinical features (hx and o/e)
hx:
- 50% asymptomatic + only discovered at phys/USS exam
- sx related to site than size
- submucosal fibroid -> abnormal menstrual bleeding
- subserosal fibroids -> asymptomatic
- menstrual problems: HMB in 30%, IMB if submucosal/polyploid
- common in perimenopausal women
- DYSMENORRHOEA RARE= seldom cause pain unless torsion, red degeneration (uterine leiomyeloma infarct), sarcomatous change
- large fibroid on bladder = urinayr frequency/retenion
- on ureters = hydronephrosis
- fertility impaitred if tubal ostia blocked/submucosal fibroids prevent implantation
sx:
- none 50%
- menorrhagia (30%)
- erratic/bleeding (IMB)
- pressure effects
- subfertility
o/e:
- solid mass may be palpable on pelvic/abdominal exam, arise from pelvis and continuous with uterus
- multiple small fibroids cause irregular ‘knobbly’ enlargement of the uterus
fibroids: natural history/complications
enlargement slow = stop growing and calcify after menopause
enlarge:
- oestrogen in HRT may stimualte further growth
- englarge mid-pregnancy
pain and degenerations:
- pedunculated fibroids -> torsion
- red degreneration = pain and uterine tenderness, haemorrhage and necrosis
- hyaline/cystic calcificaiton (postmenopausal/asymptomatic)
malignancy:
- 0.1% leiomyosarcomata = diagnosed only on histology
- consider when fibroid growth in postmenopausal women or rapidly enlarging fibroids or sudden onset of pain in women of any change
fibroids and pregnancy
premature labour, malpresentations, transeverse lie, obstructed labour and PPH can occur
red degeneration common in pregnnacy -> severe pain
should NOT be removed at C-section as bleeding can be heavy
pedunculated fibroids may tort postpartum
fibroids and HRT
cause continued fibroid growth after menopause
tx is as for premonopausal women or the HRT is withdrawn
fibroids ix
establishing diagnosis:
- examination
- USS = screening, number/size/position of fibroids (MRI is diagnosis unclear or greater accuracy is required e.g. fibroids vs adenomyosis)
- hysteroscopy, saline TV ultrasonography or HSG = assess distortion of uterine cavity, particularly if fertility is an issue
establishing fitness:
- Hb concentration may be low from HMB but also high as fibroids can secrete EPO

fibroids tx
medical
ONLY TX when cause symptoms/QoL affected/desire for fertility
Injectable GnRH agonist:
- bone density loss restrict use to only 6 months so used near menopause or to make surgery easier and safer
- concomitant use of ‘add-back’ hRT prevents these effects without enlargement allowing longer adminsitration
- fibroids return back to their normal size once stopped
SUMMARY:
- 1st line symptomatic: LNG-IUS
- Other options: tranexamic acid, COCP
- GnRH agonists may be used to reduce the size of the fibroid (usually only iN the short-term prior to surgery)
- Surgery:myomectomy, hysteroscopic endometrial ablation, hysterectomy
- Interventional Radiology: uterine artery embolisation

fibroids: surgical tx

fibroids: radiological tx

Fibroids: PACES tips

is the fibroid malignant?
uncommon, but more likely if there is:
- pain and rapid growth
- growth in postmenopausal woman not on HRT
- poor response to GnRH agonists or ulipristal acetate
Fibroids at a glance

Adenomyosis definition and epidemiology
aetiology
endometrium grows into myometrium
common around 40 years, associated with endometriosis and fibroids
sx subside after menopause
oestrogen dependent

adenomyosis clinical features
history = sx may be absent, but painful, regular, heavy menstruation is common
examination = the uterus is mildly enlarged and tender
adenomyosis ix and tx
ix = suspected on USS, clearly diagnosed on MRI
tx:
- progesterone IUS or
- COCP with or without NSAIDs cto contorl menorrhagia and dysmenorrhoea
- hysterectomy often required
other benign conditions of the uterus: endometritis
an inflammation or irritation of the lining of the uterus
2o to STIs, as a complication of surgery (C-section and intrauterine procedures), or because of foreign tissues (IUDs) and retained products of conception
infection in postmenopausal uterus is commonly due to malignancy = uterus tender and pelvic and systemic infection may be evident
pyometra = pus accumulates and unable to escape
tx = abx and ERPC
other benign conditions of the uterus = intrauterine polyps
small benign tumours that grow into uterine cavity
- occasionaly contain endometrial hyperplasia or carcinoma
most endoemtrial in origin but some drived from submucous fibroids
common women 40-50 years and when oes levels are high
in post-menopausal women = in pts on tamoxifen for breast carcinoma
occasionally prolapse through cervix, sometimes asymptomatic, often menorrhagia and IMB
Ix:
- USS or when hysteroscopy performed because of abnormal bleeding
Tx:
- resection of polyp with cutting diathermy or avulsion normally cures bleeding problems

other benign conditions of the uterus: haematometra
menstrual blood accumulte in uterus because of outflow tract obstruction, uncommon
cervical canal usually occluded by fibrosis after endometrial resection, cone biopsy or a carcinoma
imperforate hymen, blind rudimentary uterine horn, present in adolescence as primary amenorrhoea
other benign conditions of the uterus: congenital uterine malformations
abnormalities from differeing degrees of failure of fusion of the two Mullerian ducts at about 9 weeks
25% cause pregnancy-related problems that lead to their discovery
- transverse lie/malpresentations, preterm labour, recurrent miscarriage (<5%) or retained placenta
tx
- simple septa can be resected hysteroscopically
- rudimentary horns need removal at either open or laparaoscopic surgery
- bicornuate uteri are no longer treated surgically as the complication rates were too high

Endometrial carcinoma: epidemiology
most common GYN cancer, 1% risk developing it by 75
prevalence highest at 60 years, <15% occurs premenoapusally and <1% under 35 years of age

Endometrial carcinoma: pathology (2 types)
Type 1 (most): low-grade endometrioid cancers which are oestrogen sensitive, associated with obesity, and usually less aggressive, atypia as a precursor
Type 2: high-grade endometrioid, clear cell, serous or carcinosarcoma cancers which tend to be more aggressive and not oestrogen sensitivie, not related to obesigty
Endometrial carcinoma: risk factors
tamoxifen
protective factors
main RF = exposure to endogenous/exogenous oestrogens associated with obesity, diabetes, early age at menarche, nulliparity, late-onset menopause, older age >55 years, unopposed oestrogen HRT, and use of tamoxifen
tamoxifen
- although an oes antagonist in breast and used to tx breast cancer, it is an agonist in postmenopausal uterus
protective factors = COCP and pregnancy
endometrial carcinoma: premalignant disease (endometrial hyperplasia with atypia)
what happens after diagnosis
unopposed/erratic oestrogen -> hyperplasia of endometrium
menstrual abnormalitis or PMB = premalignant
hyperplasia with atypia often coexists (40%) with carcinoma elsewhere in the uterine cavity, uncommon in women of reproductive age
after diagnosis:
- hysterectomy discussed
- fertility is a concern, progestogens (IUS or continuous oral) and 3-6 monthly hysteroscopy and endometrial biopsy are used along with referral to a fertility specialist for consideration of treatment
premalignant disease (endometrial hyperplasia with atypia) mx

Endometrial carcinoma: clincial features
History: PMB (10% risk carcinoma) is the most common presentation, premenopausal patients have irregular bleeding or IMB
Examination: pelvis often appears normal, atrophic vaginitis may coexist
Endometrial carcinoma: spread and staging
Spread:
- spreads through myometrium to cervix and upper vagina, ovaries may be involved
- lymphatic spread to pelvic and then para-aortic lymph nodes
- blood-borne spread is late
Staging
- sugical and histological and includes lymph node involvement (cervical carcinoma does not)
Histological grade:
- G1-3 is also included for each stage, G1 being a well-differentiated tumour

Endometrial carcinoma: Ix
abnormal vaginal bleeding investigated
depending on age, menopausal status and sx (i.e. likelihood of underlying cancer) = USS and/or endometrial biopsy with Pipelle or hysteroscopy is performed
- endometrial buipsy required to make the diagnosis
- staging only possible following hysterectomy
MRI to estimate myometrial invasion and so guide appropriate referral to a cancer centre in cases with deep invasion
CXR to exclude rare pulmonary spread
Assess pt fitness:
- FBC, renal function, glcuose testing and ECG normally required as most patients are elderly
Endometrial carcinoma tx: surgery

General indications for radiotherapy in endometrial carcinoma
high risk for extrauterine disease: deep myometrial or cervical stromal spread, poor grade
proven extrauterine disease
inoperable and recurrent disease
palliation for symptoms e.g. bleeding
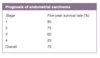
endometrial cancer prognosis
recurrent most common at vaginal vault, normally in the first 3 years
poor prognostic features are older age, advanced clinical stgae, deep myometrial invasion in stage 1 and 2 patients, high tumour grade and adenosquamous histology
Uterine sarcomas: 2 examples
rare
leiomyosarcomas are ‘malignant fibroids’ and present with rapid, painful uterine ‘fibroid’ enlargement
tx with hysterectomy but early recurrence is common due to haematogenous spread, radiotherapy or chemotherapy can be used following hysterectomy but overall survival only 30% at 5 years
endometrial stromal tumours are tumours of stroma beneath the endometrium (benign endometrial stromal nodule to highly malignant endometrial stromal sarcoma), most common in perimenopausal women
Endometrial carcinoma at a glance



