The Aetiology and Treatment of Type 2 Diabetes Mellitus Flashcards
What is the definition of diabetes mellitus?
A state of chronic hyperglycaemia sufficient to cause long-term damage to specific tissues, notably the retina, kidney, nerves, and arteries
State 3 characteristics of T2DM
- Not ketosis prone
- Not mild
- Often involves weight, lipids and blood pressure
What tests are performed to diagnose diabetes and what are the defining values?
Fasting blood glucose test:
- Normal: < 6 mmol/L
- Impaired fasting glucose: 6-7 mmol/L
- Diabetes: > 7 mmol/L
Glucose Tolerance Test (2 hour measurement):
- Normal: < 7.8 mmol/L
- Impaired glucose tolerance: 7.8-11.1 mmol/L
- Diabetes: > 11.1 mmol/L
NOTE:
Glucose tolerance test:
- The patient is asked to take a glucose drink
- Their blood glucose level is measured before and at intervals after the glucose drink is taken
- After 2 hours the blood glucose level will be higher in a diabetic individual than a healthy person due to lack of insulin effect
Describe the epidemiology of T2DM.
- Diabetes is prevalent (10% at 60 years)
T2DM:
- Has the highest prevalence out of all the diabetes subtypes
- Occurs with increasing age, but now in children
- Prevalence varies enormously from country to country
- Increasing in prevalence with time
- Occurring and being diagnosed younger
- Greatest in ethnic groups that move from rural to urban lifestyle
- i.e. precipitated by change in environment
- Influenced by both genetics and environmental factors
- T2DM has a bigger genetic influence than T1DM
- Mainly genetic condition but can be accelerated by poor lifestyle choices
What is the pathophysiology of T2DM in general?
Insulin resistance and insulin secretion defects - this mechanism leads to T2DM
- Lack of insulin is present in T2DM patients but is not absolute
- Ther patient still has enough insulin to switch of ketone production (therefore DKA is rare) but not enough to switch off HGO
Fatty acids important in pathogenesis and complications
- Pathogenesis: some FAs can damage beta cells and lead to insulin resistance
- Complications e.g. CVD
State three factors that influence the pathophysiology of T2DM.
- Genetics
- Intrauterine environment
- Adult environment
What is MODY?
MODY = Mature onset diabetes of the young
- 8 types: MODY 1-8
- Relatively uncommon but gives useful metabolic insights
- You know which genes are affected resulting in the diabetes
- This helps you identify the processes involved in blood glucose control
- Therefore gives useful insight into what could go wrong to result in T2DM - i.e. the pathophysiology
- Autosomal dominant
- Ineffective pancreatic beta cell insulin production
- Mutations of transcription factor genes, esp glucokinase gene
- Glucokinase required for ATP production inside beta cell and ATP required for insulin release
- TFs influence beta cell activity so a mutuation can alter beta cell activity
- Positive family history, no obesity present
- Specific treatment is given for MODY type
Explain the pathophysiology of T2DM in detail.
Genes result in insulin resistance
- T2DM has a bigger genetic influence than T1DM
- Inheritance pattern behaves like that of an autosomal dominant disease
- This means that target cells are less sensitive to insulin so you need more insulin to have the same effect (compensatory hyperinsulaemia)
- Insulin resistance probably operates through adipocytokines
- i.e. Cytokines released by fat cells contribute to the development of insulin resistance
Intrauterine growth restriction (IUGR) = lack of calories (nutrients) in utero
- This can modulate gene expression of the foetus for the rest of the foetus’ life
- Protein restriction in utero seems to have a significant impact on pancreatic development leading to impaired glucose tolerance
Obesity progresses insulin resistance - i.e. makes it worse
Some fatty acids can lead to insulin resistance - if you are obese you have higher levels of FAs anyway
Insulin resistance has metabolic effects and leads to dyslipidaemia (abnormal amount of lipids in the blood)
Insulin affects two pathways: metabolic and mitogenic
- Compensatory hyperinsulaemia allows control of blood glucose levels but it means the mitogenic pathway is activated in excess
These factors can then lead to macrovascular disease - build up of fat in the circulation and progression of atheroma
This could all be happening for years before someone actually becomes hyperglycaemic
Over time the insulin resistance leads to beta cell dysfunction - the consequences of beta cell dysfunction trigger beta cel dysfunction
Therefore they can no longer make enough insulin to compensate for their insulin resistance
- This results in hyperglycaemia → leads to microvascular disease
- This is also why eventually T2DM patients may end up needing insulin replacement
- Beta cell failure also worsens the dislipidaemia

What happens as we age?
- We become progressively more insulin resistant during adulthood
- Not quite sure what happens during childhood
- Our ability to produce insulin (insulin secretion capacity) also progressively declines
- This is a natural process of ageing
- After the two lines meet, meaning that you no longer have enough insulin production to compensate for the level of insulin resistance, then it is a problem
- For people with no problem this would happen beyond the normal life expectancy
- However, for people with T2DM, this crossover happens earlier on in their lifetime

Describe the presentation of a typical patient with T2DM.
- Heterogeneous
- The way that it presents is very variable
- Obesity
- Very common in T2DM patients
- Insulin resistance and insulin secretion deficit
- Hyperglycaemia and dyslipidaemia
- Acute and chronic complications
Describe the metabolic pathways which lead to hyperglycaemia and dyslipidaemia.
- Fat stores (adipocytes - stores eneergy in the form of triglycerides (TG)
- TG can be broken down into glycerol and non-esterified fatty acids (NEFA)
- These can drain into liver
- Mostly the omental fat cells drain into liver (compared to fat cells in limbs)
- Fatty acids cannot directly be used to produce glucose
- Glycerol can be used in gluconeogenesis to form glucose
- You need 2 molecules of glycerol (3C) to form one molecule of glucose (6C)
- Glycogen can also be broken down to produce glucose -glycogenolysis
- Both gluconeogensis and glycogenolysis lead to HGO to maintain adequate blood glucose levels (approx 5 mmol/L)
- Thi is to allow sufficient glucose for the brain
- FAs in liver packaged ito lipoproteins → VLDL
- VLDL carries triglycerides from the liver to other body tissues in the circulation
- NOTE: VLDL - composed of a higher percentage of TG than other lipoproteins (e.g. LDL)
Insulin resistance:
- HGO continues but there reduced glucose uptake into muscle to be stored as glycogen → hyperglycaemia
- TG continues to be broken down so too much fat comes to liver → too much VLDL production → atherogenic lipid profile
- Normally after a meal, insulin would inhibit TG breakdown as it is not necessary
- Insulin resistance - lipid profile is more the problem due to hyperinsulaemia to compensate for the hyperglycaemia
- Insulin deficit - hyperglycaemia becomes more of a problem

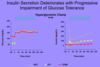
Describe the deterioration of insulin secretion in T2DM.
Normally in response to IV glucose - 2 phases of insulin secretion:
- 1st Phase - stored insulin that is ready to be released
- 2nd Phase - over a period of time, more insulin is produced and released
In T2DM:
- People who are developing diabetes will still have some insulin production but this is reduced
- The biggest drop observed is in the first phase response but they also produce less insulin over time
- Due to decline in beta-cell sensitivity and responsiveness to glucose
- As insulin secretion progressively decreases, it eventually becomes chronically insufficient
- Therefore, insulin needs to be replaced
Describe how insulin resistance is demonstrated in T2DM.
Insulin lowers blood glucose by reducing HGO
- When we have not eaten, our hepatic glucose output maintains our blood glucose level
- After we’ve eaten, insulin stops HGO
- Does this because you don’t need this output from the liver once you’ve just eaten
- Therefore, HGO not being switched off after a meal demonstrates insulin resistance
Other effects of insulin:
- Once we’ve eaten and the glucose from the meal has entered our blood, insulin drives the glucose into muscle and adipose tissue for energy storage or use
- The lack of glucose clearance from the plasma also demonstrates insulin resistance

Describe the difference in age-related changes of insulin sensitivity and secretion between a normal person and T2DM patient.
- As age increases by your insulin sensitivity decreases
- So your insulin secretion should increase to compensate for the reduced sensitivity and maintain normal blood glucose levels
- Red dot moves left along this path
- People developing diabetes will not increase their insulin secretion sufficiently to balance the decrease in insulin sensitivity
- So, they will fail to make enough insulin for their given insulin sensitivity
- This leads to hyperglycaemia and therefore diagnosis of diabetes

What is an important characteristic of adipocytes?
- Adipocytes are a major endocrine organ
- Not just inert energy stores
- They produce a whole range of hormones which are released in response to a certain stimulus
- Different hormones shown in the picture - don’t need to memorise them
- These hormones don’t seem important in the cause of diabetes
- However, all of them seem important in the mechanism of diabetes
- These hormones are means by which the changes in metabolism observed during T2DM development comes about
- There is particular interest in the role of adipocytokines (e.g. adiponectin) in the mechanism of insulin resistance
Describe the link between obesity and T2DM.
- More than a precipitant
- i.e. More than just a cause but also important in the mechanism
- Fatty acids and adipocytokines important
- Central or omental obesity
- This is more risky compared to just being overweight overall
- 80% T2DM are obese
- Weight reduction useful treatment
Describe how gut microbiota is implicated in T2DM.
- The gut microbiome appears to be associated with obesity, insulin resistance and T2DM
- So far studies have found association rather than causation
- This may be important through signalling to the host
- i.e. Communication between gut microbiota and the host cells
- Various lipopolysaccharides are fermented by the gut bacteria to short chain fatty acids
- These short chain fatty acids enter the circulation and modulate bile acids
- Could drain into liver and alter liver metabolism
- They are important in inflammation and metabolic pathways
- Can modulate these pathways
NO
What is a very common side effect of diabetes treatment?
Weight gain
- Although weight loss is important in the treatment of diabetes, most treatements tend to cause weight gain
- EXAMPLE:
- One of the ways insulin leads to weight gain is by preventing loss of glucose in the urine (glucosuria)
- This glucose has to be stored somewhere so is stored as fat
Which diabetes treatment does not cause this problem?
Metformin
- Therefore it is very important as a first line treatment of T2DM
How does T2DM present?
- Osmotic symptoms
- Infections
- High levels of glucose in the body allows microorganisms to grow more quickly
- High levels of glucose especially in urine → bladder, kidney infections common
- High levels of glucose in the body allows microorganisms to grow more quickly
- Screening test
- To test for diabetes before it presents with a complication - i.e. identify asymptomatic individuals who are likely to have diabetes
- Patients often identified as having T2DM at presentation of complication
- Acute: hyperosmolar coma
- Severe hyperglycemia, extreme dehydration, hyperosmolar plasma
- Chronic: ischaemic heart disease, retinopathy
- Acute: hyperosmolar coma
What are the potential complications of T2DM?
Microvascular
- Retinopathy
- Nephropathy
- Neuropathy
NOTE: -pathy = damage
Macrovascular
- Ishcaemic heart disease
- Cerebrovascular
- Renal artery stenosis
- Peripheral vascular disease (PVD)
Metabolic
- Lactic acidosis
- Hyperosmolar crisis
NOTE: Metabolic complications in T2DM is a lot less common compared to ketoacidosis in T1DM
Complications of treatment
- Hyperglycaemia
hypoglycaemia
What are the basics in managing diabetes?
- Education
- Diet
- Pharmacological treatment
- Complication screening
Why should we treat T2DM?
- It can help the symptoms of T2DM
- Reduces the chance of acute metabolic complications
- Though these are unlikely in T2DM
- Reduce the chance of long-term complications
- Good evidence base (UK prospective diabetes study or UKPDS)
- EDUCATION
- People generally only treat things if they have symptoms
- So it’s important to educate them about the consequences of poor treatment
What dietary measures are recommended for someone with T2DM?
- Control total calories/increase exercise
- Helps with weight loss
- Prevents weight gain
- Reduce refined carbohydrate
- So eat less sugar
- Raises blood glucose levels quickly
- Increase complex carbohydrate
- So eat more rice etc.
- Raises blood glucose levels for slowly
- Reduce fat as proportion of calories
- Less insulin resistance - as some fatty acids can lead to insulin resistance
- Increase unsaturated fat as proportion of fat
- To reduce risk of ischaemic heart disease (IHD)
- Increase soluble fibre
- Takes longer to absorb carbohydrates so raises blood glucose levels more slowly
- Address salt
- To reduce risk of hypertension
- Hypertension increases risk of cardiovascular complications which is higher anyway due to the diabetes


