Thallasemia Flashcards
What is Thalessima?
Genetic inability to produce any of the A or B chains of haemoglobin
What is the inheritance pattern of thallasemia?
Autosomal recessive
Chromosome 11
What are the four types of alpha thallasemia?
Minina - one gene - carriers
Minor - 2 genes - mild microcytic anaemia
Haemoglobin h - 3 genes - symptoms
four - Fetal death
What do A and B thalessemia have in common biochemically and pathogensis wise
Reduced O2 carrying capability Haemolysis of damaged cells
Microcytic anaemia (keep dividing to find right haem concentration). Low MCV
What is the difference in pathophysiology of alpha and beta?
Alpha - Insufficient haemoglobin due to excessive B chain formation and abnormal dissociation curves. Can lead to hydrops foetalis if fetus cant make alpha or fetal haemoglobin
Beta - Decreased RBC and production and increased damage due to excessive Alpha chains binding to precursor membranes
Why doesnt hydrops foetalis occur in B thallasemia?
Fetal haemglobin is alpha and gamma
What is B thallesmia minor or major
Minor - one copy of faulty gene (mild anaemia and normal iron levels)
Major - both copies - Symptoms
Where are beta thallasemias common?
People of Italian or Greek descent
How many alpha genes are there and how many beta?
4 alpha. 2 beta
How many genes code for each A chain?
2, so four per haemoglobin
When is thalessemia fatal?
If all four A chains are mutated in pregnancy as A is needed for foetal haemoglobin
What are the symptoms of (mild) or moderate thalessemia (Five)
Mild Asymptomatic
Moderate - Anaemia
Microcytosis
Jaundice, hepatpsplenomegaly - Breakdown in RBC in organs
Frontal bossing and maxillary prominence
Shortened limbs and fingers due to ischameia and premature epiphyseal plate closing
Iron overload and cirrhosis

What is this?
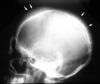
Hair on end sign for thallasemia or SCA
What are the investigations for thalessemia?
Genetic testing
X rays
Bloods - High reticulocytes and microcytic anaemia
What is the management for thalessemia
Transfusions
Genetic counselling
Iron chellation/desferroximine
What other chemical increases in Sickle cell and Thallasemia?
EPO
What is key in B thallesemia?
Increased RBC breakdown
What can be a long term consequence of poorly controlled thallasemia?
Liver cirrhosis
What is hydrops faetalis?
Fotel death due to alpha thallesemia and the inabilty to make alpha chains or fetal haemoglobin


