Tachyarrhythmias Flashcards
Case 1
- 27 y.o. man with asthma
- 3 days runny nose, sore throat, headache, feverish
- Clenil and PRN salbutamol inhalers
- HR 112 reg/strong, BP 125/55, CRT<2s
- sats 98% (A), RR 18, chest clear
- temp 36.0 / abdo SNT / GCS 15
- throat little red, no exudate, no cervical lymphadenopathy
-
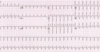
1a) This is his ECG. What is your dx?

sinus tachycardia
2b) what are the causes of sinus tachycardia?
- physiological: exercise, pregnancy
- infection
- dehydration
- pain
- hyperthyroidsm
- PE
- anxiety
- drugs: cocaine, speed, salbutamol
Case 2
- 35 y.o. man, smokes, no reg meds
- at work on building site
- 20 minute sudden onset palpitation with central chest tightness, light headness
- looks clammy
- HR 200 ?reg, BP 120/86, CRT=2
- chest clear, RR 26, sats 98% air
- temp 36.2 / abdo SNT / GCS 15
-
2a) This is his ECG. What is the dx?
AV node re-entrant tachycardia (AVNRT) = “paroxysmal SVT”
2b) In whom does AVNRT occur in?
- young adults
- female > men
- triggers: caffeine, drugs, fatigue
- rate >180bpm
2c) How is AVNRT managed?
- vasovagal manoeuvres
-
adenosine IV bolus 6mg / 12mg / 12mg → monitor ECG
- C/I in asthma! → profound bronchospasm → give CCB
- DC cardioversion if adverse features
2d) What are the adverse features?
- shock
- syncope
- myocardial ischaemia
- heart failure
what does supraventricular tachycardia mean?
- supraventricular = originates above ventricles
- tachycardia, HR>100bpm
- narrow complex <120ms / 3 small squares
what are the types of SVT?
-
Atrial
- sinus tachycardia
- AF
- atrial flutter +/- variable block
-
AV Node
- AVNRT - ‘paroxysmal SVT’
- Wolff-Parkinson-White
Case 3
- 78 y.o. man
- PMH: IHD, HTN, T2DM, CKD3, ex-smoker
- meds: aspirin, simvastatin, ramipril, metformin, GTN, NKDA
- 3 day productive cough + fever
- HR 130 irreg irreg, BP 135/65, CRT<2, no leg oedema, JVP normal
- left basal creps, no wheeze, sats 98%, RR 19
- temp 38.2 / abdo SNT / GCS 15 / BM 11.9
- PU this AM, slightly darker than usual
- bloods: urea 10.1, creatinine 148 (baseline for pt 90-100), CRP 78, WCC 13.4, lactact 2.1
- CXR: left basal consolidation, cardiomegaly
- urine dip: negative
-
3a) This is his ECG. What is the dx?

atrial fibrillation
- irregularly irregular
- no P waves
- narrow QRS (<120ms / 3 small boxes)
- normal target rate for AF ~90bpm
- ‘rapid ventricular rate’ >100bpm
3b) Name 2 scoring systems that could be used in this pt to assess how unwell he is.
- CURB-65
- SIRS
- qSOFA

3c) Why might he have AF?
- pneumonia
- dehydration / AKI
- structural heart disease: IHD + HTN
3d) What do you consider in the mx strategies for AF?
Consider:
- what is the BP?
- are there adverse features?
- is there a precipitating cause?
Mx:
- rate or rhythm control?
- add on anticoagulation?
3e) What is the aim for AF mx?
<110bpm
asymptomatic
3d) What are medications that can be used in rate control for AF?
- bisoprolol
- rate-limiting CCB e.g. verapamil
- digoxin
3e) What are medications that can be used for rhythm control in AF?
- amiodarone
- flecainide
3f) What are medications that can be used for anticoagulation in AF?
- warfarin
- DOAC e.g. edoxaban
3g) How would you manage this pt?
- treat underlying cause
- sepsis 6
- withhold nephrotoxics
- check electrolytes
- repeat ECG once underlying illness better
- if persistent AF: rate / rhythm / anticoagulate
what is atrial fibrillation?
- SA node overwhelmed by disorganised electrical activity in roots of pulmonary veins
- pulmonary veins fibrosed due to atrial dilatation
what causes atrial dilatation?
- HTN
- valvular disease
- heart failure
- cardiomyopathy
- MI
- cocaine
how do you decide whether to mx with rate / rhythm control for AF?

how do you decide when to anticoagulate the pt with AF?







