STI Pictures Flashcards

Pearly Penile Papules
– fibro-epithelial lumps, in rows, soft in texture – do not cryo-therapy

Vestibular papillae

Fordyce spots – small sebaceous cysts - normal

Tyson’s glands – small sebaceous glands

Lymphocoele

Fixed drug eruption – often antibiotics (esp tetracyclines)

Lichen Planus
- Dysparunia, maybe with a little bleeding after intercourse
- Moderate discharge, may be scanty
- No odour but some irritation
- Regular partner.
- O/E vaginal skin thin, red, maybe superficial haemorrhagic areas, cervix is ok

Diagnosis Atrophic Vaginitis
Significant Features post-menopausal, dysparunia, thin reddened vaginal skin
Aetiology It is due to a loss of oestrogens. The vagina loses the rugae, elasticity, and natural defences.
Treatment Easy. Give exogenous oestrogens. You can give them topically with creams or pessaries, or systemically with pills or transdermal patches.
- 2-3 days of dysuria
- 1 day heavy urethral discharge
- New female partner 2 weeks
- Not using condoms

Gonococcal Urethritis
Urethritis
- Gonococcal?-Chlamydia?
- Other (NSU)? -HSV, Trich.Vaginalis, Mycoplasma genitalium, Adenovirus, Ureaplasma Urealyticum, trauma,
- Reiters’ syn.
- yellowish discharge
- lower abdominal pain
- dysuria and dysparunia
- O/E purulent cervical and vaginal discharge, and pelvic tenderness.
- Casual male partner / 10d / no condom

Gonorrhoea cervicitis
Diagnosis Vaginal thrush Candida albicans
Management
Antifungal cream or pessary – Eg Clotrimazole
or
Fluconazole
- Married – no other contacts
- 2 weeks of profuse greyish-green discharge with offensive odour
- Pain with intercourse
- Bubbles in discharge and odour
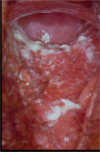
- Erythematous cervix with punctate appearance

Trichamonas vaginitis
Investigations
wet prep to see the Trichomonads. They are flagellated protozoae
Management
Usually use oral Metronidazole or Tinidazole, except you can’t use these in pregnancy (use Clotrimazole in pregnancy)
It is a genuine STD, so you must treat both partners
- 1 week of profuse smelly discharge
- No pain or itch
- O/E greyish watery discharge, no associated inflammation, odour present
- Has had it before
- Has regular male partner, no other contacts.

Bacterial vaginosis •Gardnerella vaginalis, •Mycoplasma hominis and •Mobiluncus
Investigations
- Cervical swab – MCS
- Wet prep – micro – “clue” cells
- Vaginal pH >4.5
- Other STI screen if appropriate
Management
•Metronidazole 400mg bd for 7 days.
or
•Clindamycin cream 2% PV nocte x7d.
Or
•Metronidazole gel 0.75% PV nocte x5d
- Recurring penile irritation
- Small itchy sores on penis last 12 hours
- Present on and off for years with the sores lasting 5-7 days and usually in roughly the same area.
- Has regular partner, no other contacts

Herpes Simplex - vesicular stage
- Painful? (YES –> HSV NO –> Syphilis)
- Recent medications (fixed drug reaction?)
- Recent topical applications?
- Trauma?
- Sexual contacts – overseas? (syphilis, chancroid, LGV, donavanosis)
- Same sex partners ? (syphilis)

Herpes Simplex – meatal ulcer
- Very painful external genitalia 2-3d
- Severe dysuria and dysparunia
- Ulceration visible
- New sexual partner last week

Herpes Simplex in the vulva

Herpes Simplex - outer vulva

Herpes simplex - oedema
- Gay male
- Recently noticed lesion on penis
- It is painless
- He practices “safe sex”

Syphilis – primary - chancre

Syphilis – secondary, but again a genital ulcer

Syphilis – secondary – generalised pleomorphic rash

Syphilis – secondary – always beware of rashes on palms or soles

Syphilis – secondary – soles of feet. In this case also HIV+
Tropical travel

•LGV (Lymphogranuloma Venereum)
Chlamydia trachomatis serovars L1-L3
Azithromycin 1gm if suspicious
Or
Doxycycline 100mg bd x21d. If confirmed








