STI & Eye Flashcards
which STI is usually asymptomatic?
chlamydia
If a male has uretheral disachrge, what should you test for?
Gohonorrhea
Chlamydia (even though usually symptomatic, is more common than gonorrhea)
how often should one be screened for chlamydia?
yearly from aged 15-30 if they are sexually active
how does chlamydia normally present?
normally asymptomatic
discharge from penis / vagina
pain during urination
pain during sex
What are the complications of chlamydia in men and women?
Men
- Epididymitis & Epidydimo-Orchitis; which can lead to
- Infertility
- Reactive Arthritis (more common in men)
Women
- Pelvic inflammatory disease; which can lead to
- Infertility
- Ectopic pregnancy
- Persistent pelvic pain
Which STI can cause a reactive arthritis and in which sex?
chlamydia
reactive arthritis caused by chlamydia is more common in men than in women
What is the management of chlamydia?
Basics
Place & Person
Investigate & Confirm Diagnosis
- NAAT: specimen collected by -
- first pass urine
- endocervical swab
- cultured urethral discharge (if present)
Definitive Management
- 1g azithromycin po as a single dose
- Abstain from unprotected sexual intercourse for at least 7 days during and after treatment
- A notifiable disease - must notify DHS within 5 days of diagnosis
Follow-Up
- Contact tracing - advise to dicuss with sexual partners so they can be screened
- Re-test for chlamydia 3-4 months post treatment
how do you investigate for chlamydia?
NAAT
Method of collection:
- first pass urine
- endocervical swab
- urethral discharge (if present)
what is the typical presentation of gohnorrhea in men?
and in women?
Man with copious urethral discharge 2-10 days after unprotected sex (although chlamydia is still more common than gonorrhea, so still more likely to be chlamydia).
Women are usually asymptomatic or present with vague symptoms mimicking a UTI.
What is required to investigate for gonorrhea?
NAAT. Specimen collected by
- Urine (mid stream)
- Endocervical swab
- Rectal swab
- Throat swab
- Culture of discharge
Also investigate for chlamydia if you suspect gonorrhea!
what is the definitive management of chlamydia?
what is the definitive management of gonorrhea?
how are these managements potentially related?
Chlamydia = 1g azithromycin po, single dose
Gonorrhea = Ceftriaxone 250mg IM, single dose
If you are treating for gonorrhea, but you haven’t ruled out chlamydia - treat for chlamydia as well
What is the management of gonorrhea?
Investigate and Confirm Diagnosis
- NAAT, collected by:
- MSU
- Rectal swab
- Pharyngeal swab
- Endocervical swab
- Cultured discharge (if present)
Definitive Management
- IM 250mg ceftriaxone
- Advise to abstain for sex for 7 days?
Follow Up
- Notifiable disease - notify DHS within 5 days
- Contact tracing - treat sexual partners empirically
- Offer eductaion RE safe sexual practises
- Re-investiage 3-4 months after treatment, to ensure complete treatment
- ALSO TEST / TREAT CHLAMYDIA
Which STI is described as “the great imitator”?
Syphillus
What is the name of the microorganism which causes syphillus?
Treponema pallidum
How does primary syphillus present?
A single painless ulcer in the genital area (chancre)
What is the pathophysiological progression of syphillus?
Remember Syphillus happens in Stages
- Primary = Chancre
- Secondary = Secondary erruption on skin and mucous membranes (rash) +/- systemic symptoms
- Then long periods of latency
- Teritiary (10-30 years after infection) = late lesions of skin, bone, viscera, cardiovascular and central nervous systems (this is why it’s called the great mimcker)
How do you investigate for syphillus?
Syphillis EIA (blood test)
what is the definitife management of syphilllis?
early (
late (>2 years or unknown) = IM benzthine penicillin, weekly for 3 weeks
tertiatry syphillis (>2 years and with skin, bone, CVS or neurological involement) = IV benzylpenicillin
What is the overall management of syphillis?
Investigate and Confirm Diagnosis
- Seroloigcal test - Syphillis EIA
Definitive Management
- Early - IM benzathine penicillin, once off
- Late or unknown - IM benzathine penicillin, once per week for 3 weeks
- Tertiary - IV benzylpenicillin for 15 days
- Abstain from sex until completion of treatment
Follow-Up / Other
- Test for other STIs
- Notifiable disease - contact DHS
- Contact tracing
- Retest 3-4 months after completion of treatment
what is a common presentation of bacteral vaginosis?
asymptomatic
fishy-smelling vaginal discharge
dysuria
vaginal pruritis
pyspareunia
how do you diagnose bacterial vaginosis?
- Clincially
- presence of mucous dishachrge
- fishy smell
- clue cells on micrscopy (culture not required)
- Vaginal pH >4.5
What is the defitive management of bacterial vaginosis?
metronidazole (orally or vaginal gel)
OR clindamycin (orally or vaginal gel)
What is the pathophysiology of bacterial vaginosis?
- Reduction in the acid-producing normal flora of the vagina [Lactobacillus]
- Leads to growth of anaerobes and other fastidious microorganisms
What is glaucoma and what are it’s types?
High intraoccular pressure causing death of optic nerve cells.
Open angle glaucoma = poor drainage of aqueous pressure due to dysfunctional drainge by the canal of schlemm
Closed angle glaucoma = poor drainage due to closure of the angle between the cornea and the iris
What is the typical presentation of open angle glaucoma?
It is asymptomatic!
Patient’s may have loss of peripheral vision, but usually won’t notice
What examination findings are typical of glaucoma?
- raised pressure
- cupping on ophthalmoscopy
- loss of peripheral vision (might have to be measured by a special machine called an automated perimetry)
What is the typical presentation of acute glaucoma?
An extremely red and painful eye
+/- N&V
Patients may reoprt seeing halos around lights
what are the examination findings of acute angle glaucoma?
Pupil is sluggish and mid-dilated
Slightly cloudy cornea
High pressures
Rock hard eye on palpation
What is the treatment of chronic glaucoma?
- Topical beta-blockers
- Also topical alpha-agonists, carbonic anhydrase inhibitor (Diamox), and prostaglandin analogues
- Trabeculectomy
What is a cataract?
Any opacity of the lens, regardless of aetiology
(they can occur in different parts of the lens)
What are the causes of visual loss?
Gradual Visual Loss [COAD]
- Cataracts
- Open angle glaucoma
- Age-related macular degeneration
- Diabetic retinopathy
Suddent Visual Loss [BRCO]
- Branch retinal vein occlusion
- Retinal detachment
- Central tretinal artery occlusion
- Optic neuritis
Non-eye related causes [TMG]
- TIA
- Migraine
- Giant cell arteritis
What is the typical presentation of cataracts?
Gradual loss of vision
Reduced night vision
Glare from oncoming traffic
What is a cotton wool spot and when do you see it?
ischaemic retina
diabetic retinopathy
What is seen on ophthalmoscopy in diabetic retinoathy?
dot and blot haemorrhaes
cotton wool spots (ischaemic retina)
neovascularisation (which occurs in large areas of ischaemia)
hard exudates (lipid accumulation from swelling)
What are the three types of retinal detachment?
Rhegmatogenous (the usual type)
Tractional (can happen in diabetics)
Exudative (tumor or something pushing from below)
What are the symptoms of retinal detachment? (And the DDx for each)
- Flashing lights
- DDx = migraine and posterior vistreous detachment
- Floaters (look like dark specks that obscure vision - like a swarm of flies)
- DDx = posterior vitreous detachment
- Curtain of darkness coming down
- DDX = TIA
what is the typical presentation of age-related macular degeneration?
Older patient
Progressive steady decline in central vision
Difficulty in reading (new glasses don’t help)
Elderly pt, sudden unilateral vision loss.
What are the DDx?
And what are the prognoses of each?
Branch retinal vein occlusion (will resolve spontaneously in 2 months)
Central retinal artery occlusion (requires urgent surgical referral)
What is the clinical presentation of optic neuritis?
Sudden vision loss (central scotoma is classic)
Decreased contrast and color sensitivity
Pain with eye movement
What is optic neuritis associated with?
MS
What is the management of optic neuritis
Specialist referral
IV steroids
What are the examination findings of optic neuritis?
Optic nerve head edema
Relative afferent pupillary defect
painful eye in the context of a foreign body?
corneal abrasion
which if infected may lead to corneal ulcer
What is the management of a dendritic ulcer on the cornea due to HSV?
antivirals prescribed by opthalmologist
DON’T prescribe steroids
What is another name for anterior uveitis?
iritis
What is another name for iritis?
anterior uveitis
What is the uvea?
iris, ciliary body, and the choroid
all
connected to each other and are histologically similar
What is the aetiology of anterior uveitis?
idiopathy
or associated with rheumatological conditions (HLA-B27)
What is a synechia?
A synechia is an eye condition where the iris adheres to either the cornea (i.e. anterior synechia) or lens (i.e. posterior synechia).
what is the aetiology of synechia?
Synechiae can be caused by ocular trauma, iritis or iridocyclitis and may lead to certain types of glaucoma.
what is the management of anterior uveitis?
requires urgent referral!
Topical steroid drops reduce the inflammation
Topical cyclopentolate (dilate the pupil and break down synechiae)
What is the episclera?
The episclera is a thin layer of tissue that lies between the conjunctiva and the connective tissue layer that forms the white of the eye (sclera)
what is episcleritis?
What is it’s prognosis?
Benign self-limiting condition
Resolves in two weeks without treatment
What is another name for pre-septal / post-septal cellulitis?
pre-septal = peri-orbital cellulitis
post-septal = orbital cellulitis
What is the management of periorbital / orbital cellultis?
periorbital cellulitis
often managed with oral antibiotics
orbital cellulitis
more serious condition requiring hospitalisation and parental antibiotics
complications such as intraorbital abscess formation may require surgical intervention
How do you DDx between episcleritis and scleritis?
instillation of phenylephrine 2.5%
the phenylephrine blanches the conjunctival and episcleral vessels but leaves the scleral vessels undisturbed. If a patient’s eye redness improves phenylephrine instillation, the diagnosis of episcleritis can be made.
What is the difference between a stye (external hordeolum) and a Chalazion (meibomian cyst)
Stye is an infection, red and tender
Chalazion is not tender, and is hard (due to sterile inflammation)
What is another name for stye?
external hordeolum
What is another name for a chalazion?
mebomiam cyst
What is blepharitis
Blepharitis is a chronic eye condition characterised by inflammation of the eyelids.
What is the name for inflammation of the eyelids?
Blepharitis is a chronic eye condition characterised by inflammation of the eyelids.
What is Trichiasis?
Abnormally positioned eyelashes that grow back toward the eye, touching the cornea or conjunctiva
what is photokeratitis?
photokeratitis is akin to a sunburn of the cornea and conjunctiva
How do you differentiate between viral and bacterial conjunctivities?
There are no specific clinical signs to differentiate bacterial and viral conjunctivitis.
What is the clinical picture fo conjunctivitis?>
Key features
- Gritty red eye
- Purulent discharge
- Clear cornea
History
- Purulent discharge which causes the eyelashes to stick together in the morning
- Starts on one eye and spreads to the other (usually)
- Hx of contact with a person that has similar symptoms
What is a risk factor for retinal detachment?
myopia
what is seen on opthalmoscopy in gluucoma?
Cupping
Measure the cup:disc ratio
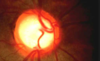
Which are arteries and which are veins?

Arteries - plaer, thinner
Veins - thicker, darker
What type of haemorrhages are seen in diabetic retinopathy?
dot and blot haemorrhages

what type of haemorrahes are seen on hypertensive retinopathy?
flame haemorrhages

What’s this?

Red cherry spot
Central retinal artery occlusion
What is conjunctival injection?

What is this and how is it treated?
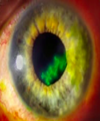
Dendritic ulcer of HSV
Treated with antivirals
What is this?

Anterior synechia
What’s this?
What is the epidemiology and typical clinical picture?

episcleritis
Affects young adults
Moderate ache
Milder symptoms than those experienced by patients with iritis
The conjunctival inflammation is usually localised to one sector
What is erysipelas?
Caused by group A strep
involving the upper dermis that characteristically extends into the superficial cutaneous lymphatics.
Tender, intensely erythematous, indurated plaque with a sharply demarcated border. Its well-defined margin can help differentiate it from other skin infections (eg, cellulitis)

What is the orbital septum?
describe the two types of cellulitis
pre-septal / peri-orbital cellulitis is anterior to the orbital septum
post-septal / orbital cellulits extends behind the septum

What is this?

stye
external hordeolum
What’s this?

Entropion
What’s this?
What is it’s clinical presentation?
What is it’s aetiology?
What is it’s prognosis?

Large bleed + Painless + Normal vision
May be associated with hypertension or heavy bouts of coughing or straining
Resolves spontaneously within 2-3 weeks
What’s this slight redness in the corner of my eye?
What treatment is required?

Pterygium
Common in hot climates
Benign fibrovascular growth from the conjunctiva
No treatment required unless growth reaches cornea à refer to ophthalmologist to be peeled back


