Spinal Cord Syndromes Flashcards
(50 cards)
What is a myelopathy?
Any disease that affects the spinal cord

The spinal cord ends at vertebral body L1-L2.
Spinal taps are done between L4 and S1, don’t worry, you are very far away from the cord!
Most back pain is lumbar. If the patient points to the thoracic area, be concerned!. Bad things happen in the thoracic cord!


Here are the CLINICALLY RELEVANT components of the spinal cord.
YES, you will see deficits in these areas in patients with spinal cord disease.
Note, that spinal thalamic tracts cross within the spinal cord, all other tracts stay ipsilateral within the spinal cord and then cross in the brain.

In addition to the spinal cord anatomy, you need to understand the relationship between the spinal cord and surrounding structures, because as these areas are damaged, they are so close to the spinal cord, the cord can easily be damaged. Note the following anatomy from the inside of the cord to the outside, in the following order:
- The spinal cord itself, also referred to as spinal cord parenchyma
- Next is pia mater
- Then subarachnoid space
- Then the subdural/intradural space
- Then the dura
- Followed by the epidural/extradural space (fat is in here)
- Finally bone (vertebral body)

Again, there are lots of synonyms and medical jargon you need to know:
EPIDURAL = EXTRDURAL
INTRADURAL = SUBDURAL
WITHIN THE SUBARACHNOID SPACE = LEPTOMENINGEAL (The pia and subarachnoid space are the ‘leptomeninges’).
WITHIN THE SPINAL CORD PARENCHYMA = INTRAMEDULLARY.
The cervical spinal cord.
CSF is white.
The spinal cord is gray/black.
Again, note the proximity of the cord to discs, vertebral bodies etc.
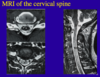
MRI of the thoracic spinal cord.
MRI of the lumbar spine. Note the end of the spinal cord and the roots as they leave the spinal cord

Patients with spinal cord syndrome commonly develop ‘sensory levels’. That is, they cannot feel sensation at or below this level.
T4 (nipple line) and T10 (umbilicus) are common sensory levels.

Bladder symptoms are common in spinal cord lesions. (Bladder control is mostly a CNS phenomena). How?
Long axons from the frontal lobe of the brain synapse in the thoracic and sacral areas of the spinal cord, thus these tracts are very vulnerable to injury in spinal cord lesions.

Two general kinds of bladder symptoms can occur in spinal cord lesions.

In acute lesions (left) there is urinary retention with some overflow incontinence.
In chronic lesions, there is a small spastic bladder that does not completely empty with spasms and urge incontinence.
Acute myelopathies are true NEUROLOGIC EMERGENCIES AND REQUIRE IMMEDIATE ATTENTION.
Your actions may determine whether or not the patient will ever walk again!
Knowing the spinal cord anatomy will help you recognize these syndromes, especially at two o’clock in the morning!



Never forget to do these things on the left of the slide.
The neurologic exam is critical and will help you to recognize and localize the lesion.

THE PACE OF SYMPTOMS IS CRITICAL AND UNPREDICTABLE.
Some patients can walk into the office, yet if not recognized, can become paralyzed in a matter of minutes as shown in this slide!

How does an epidural lesion progress?
First note the progression from A to B to C.
Let’s review ‘A’ first: Early symptoms include: At the level of the lesion, the dorsal root can be damaged or compressed which can lead to numbness or allodynia = hyper-sensitivity to touch, IPSILATERAL.
If the spinothalamic TRACT is injured at this point, very subtle changes in sensory symptoms can be seen in the CONTRALATERAL lower extremity.
The motor symptoms are extremely important and are due to compression of the corticospinal tract:
Early in the process the patient may NOT be weak, but there WILL BE NEUROLOGIC SIGNS including hyper-reflexia, positive Babinski signs and difficulty walking.
Urinary urgency is COMMON. DON”T FORGET TO ASK THE PATIENT. Many will be embarrassed and will not tell you.


B. Symptoms are worsening:
Motor: In addition to spasticity and hyper-reflexia, the legs are weak.
Sensory symptoms are worse, with numbness as shown.
Definite sphincter dysfunction – bladder and may include bowel dysfunction.
May appear as a Partial Brown Sequard syndrome = hemi-cord syndrome with weakness and numbness to touch and vibration on the ipsilateral side AND loss of pain sensation on the CONTRALATERAL side, due to the crossing of the spinothalamic tract within the spinal cord.

C. Full blown spinal cord compression – yes you will see this on the wards.
If slow and chronic, there will be spastic paraparesis with a definite sensory level to all modalities.
If acute or hyper-acute, there is so much damage to the spinal cord that ‘spinal cord shock’ occurs, which is FLACCID PARAPLEGIA WITH A COMPLETE SENSORY LEVEL TO ALL MODALITIES.

What are some extradural causes of myelopathy?
disc disease
tumor (mets, lymphoma, sarcoma, plasmacytoma)
scar
abscess
hemangioma
What are some intradural causes of myelopathy?
neurioma
meningioma
intracranial tumor seeding (ependymoma, medulloblastoma, glioma)
cauda equina lesions
What are some intramedullary causes of myelopathy?
syringomyelia
tumor (ependymoma, glioma, hemangioblastoma)
myelitis
edema
lipoma
Herniated disc and degenerative disc disease can result in cord compression.
The arrows shows multiple discs compressing the spinal cord.
The arrow heads show hyper-intense lesions within the spinal cord parenchyma.
This is edema associated with the compression.
Treatment is steroids and surgery.
This is a photo of a vertebral body fracture with acute spinal cord compression.
This patient may present with spinal cord ‘shock’, because of the acuity of the lesion.
This may result in spinal cord infarct or cord transection
What is the standard tx for spinal cord injruy?
–Methylprednisolone 30 mg/kg IV over 1 hour
–Followed by 5.4 mg/kg/hr over the next 23 hours
Cancer can affect the spinal cord at EVERY level we have discussed: intramedullary, leptomeningeal, epidural, subdural.
This slides lists many of the spinal cord problems patients with cancer can develop.
It depends on the primary cancer and the route of metastases.