Soft Tissue Infection Flashcards
A 30-year-old Florida fisherman comes to the emergency department 24 hours after cutting his palm with a fish-scaling knife. Blood pressure is 90/50 mmHg and heart rate is 120 bpm. Physical examination shows severe swelling of the hand, hemorrhagic bullae of the hand, and erythema to the mid forearm. X-ray study shows no gas within the soft tissues. A Gram stain of drainage from a bulla reveals gram-negative bacilli. Which of the following infectious agents is the most likely cause of the patient’s symptoms?
A) Clostridium perfringens
B) Mycobacterium marinum
C) Pseudomonas aeruginosa
D) Staphylococcus aureus
E) Vibrio vulnificus
The correct response is Option E.
The patient described has necrotizing fasciitis and sepsis. Vibrio vulnificus is a gram-negative bacillus, a cause of necrotizing fasciitis, and is commonly associated with warm saltwater environments (Florida). It also tends to present with hemorrhagic bullae. Staphylococcus aureus is a gram-positive coccus, is not associated with watery environments, and is more commonly associated with pustules rather than hemorrhagic bullae. Clostridium perfringens is a gas-forming, gram-positive bacillus, and is associated with marine sediment. Pseudomonas aeruginosa, also a gram-negative bacillus, although associated with moist environments, is more typically associated with less aggressive soft-tissue infections. Mycobacterium marinum is also associated with watery environments, but tends to affect aquarium owners with an indolent granulomatous process.
2018
A 53-year-old woman undergoes bilateral mastectomy and autologous breast reconstruction. Four days postoperatively, the patient reports moderate abdominal discomfort and multiple episodes of diarrhea. Vital signs are within normal range. Physical examination shows a mildly distended abdomen. Stool sample is positive for Clostridium difficile toxin. Treatment with which of the following drugs is most appropriate first-line treatment in this patient?
A) Fidaxomicin
B) Metronidazole
C) Rifaximin
D) Teicoplanin
E) Vancomycin
The correct response is Option B.
Oral metronidazole is the most appropriate treatment for this patient with a mild/moderate form of Clostridium difficile infection.
Oral vancomycin is recommended for treatment of those with severe disease, or with mild/moderate disease who did not respond to metronidazole.
Patients who cannot tolerate oral medications (eg, postoperative ileus) or who have an intestinal diversion (eg, ileostomy) can be treated with intravenous metronidazole or with vancomycin enemas. Vancomycin is not excreted into the colon and therefore should not be given intravenously to treat C. difficile infection.
Oral fidaxomicin has been shown to be as effective as oral vancomycin in the treatment of C. difficile infections. Although further clinical experience is still needed, this drug has been associated with increased cure rate in patients receiving concomitant antibiotics and decreased infection recurrence when compared to vancomycin.
Teicoplanin and rifaximin are not generally recommended for treatment of C. difficile, although isolated reports of successful therapy can be found in the literature.
2018
Which of the following time frames for onset most accurately reflects the CDC’s definition of surgical site infection?
A) Within 3 days of surgery or within 30 days of prosthetic implant placement
B) Within 7 days of surgery or within 3 months of prosthetic implant placement
C) Within 14 days of surgery or within 6 months of prosthetic implant placement
D) Within 21 days of surgery or within 9 months of prosthetic implant placement
E) Within 30 days of surgery or within 1 year of prosthetic implant placement
The correct response is Option E.
The CDC defines a surgical site infection as an infection that occurs at the incision site or within the organ or space operated on within 30 days after surgery or within 1 year if a prosthetic implant is placed. Infection requires at least one of the following:
Purulent drainage from the surgical site
Organisms isolated from an aseptically obtained culture of fluid or tissue at the surgical site
Spontaneous dehiscence of a deep incision or deliberate opening of the incision by a surgeon when the patient has at least one of the following signs or symptoms: fever (greater than 100.4°F [38.0°C]), localized pain or tenderness, localized swelling, redness, or heat, unless site is culture-negative
An abscess or other evidence of infection involving the incision or operative site that is found on direct examination, during reoperation, or by histopathologic or radiologic examination
Diagnosis of a surgical site infection by a surgeon or attending physician
2018
A 30-year-old man with AIDS is evaluated for a 6-week history of painless but increasing swelling of the flexor surfaces of the right wrist. Physical examination shows limited motion of the wrist and positive Phalen and Tinel signs. At the time of surgical exploration, rice bodies are present in the flexor tenosynovium. Which of the following is the most likely diagnosis in this patient?
A) Aspergillus fumigatus
B) Mycobacterium tuberculosis
C) Nocardia asteroides
D) Sporothrix schenckii
E) Vibrio vulnificus
The correct response is Option B.
Rice bodies are pathognomonic for tuberculosis.
Ziehl-Neelsen staining confirms the presence of acid-fast bacilli. All Mycobacterium and Nocardia species are potentially acid-fast. Many of these organisms are fastidious, so false-negative results are common. Surgeons should obtain multiple tissue samples and alert the laboratory that a diagnosis of tuberculosis is suspected. M. tuberculosis is traditionally cultured in Löwenstein-Jensen culture medium under specific temperature conditions 37.0°C (98.6°F). Histologic examination of specimens shows a granulomatous inflammatory process with the central portion of the granulomas appearing caseated.
If a mycobacterial infection is suspected, a Mantoux test should be performed. The test involves purified protein derivative injection into the dermis and evaluation of the cutaneous site after 48 to 72 hours.
M. tuberculosis should be considered in all immunocompromised patients. The other organisms can all be seen in hand infections in immunocompromised patients but do not produce rice bodies.
2017
A 28-year-old, right-hand–dominant woman is brought to the emergency department 18 hours after sustaining a cat bite to the dorsum of the hand proximal to the fifth metacarpophalangeal (MCP) joint. Which of the following organisms is most likely to be cultured from this abscess?
A) Eikenella corrodens
B) Group A Streptococcus
C) Methicillin-resistant Staphylococcus aureus
D) Pasteurella multocida
E) Pseudomonas aeruginosa
The correct response is Option D.
Pasteurella multocida is a small, gram-negative coccobacillus that is frequently associated with infections caused by dog and/or cat bites. Local findings are consistent with infection including erythema, warmth, pain and tenderness, and fluctuance or purulent discharge. Delayed treatment may result in chronic deep-space infection and/or osteomyelitis. Treatment involves starting penicillin combined with local wound care as well as surgical incision and debridement if needed.
Methicillin-resistant Staphylococcus aureus (MRSA) is becoming more common in community-acquired hand infections, but is not typically associated with dog or cat bites. Eikenella corrodens is more commonly associated with infections occurring after human bites. Pseudomonas infection is often seen as a nosocomial infection that is very resistant to antibiotics. Group A Streptococcus is a common bacterial infection associated with strep throat.
2017
A healthy 5-year-old boy is evaluated after he is bitten on the hand by a dog. He has an allergy to penicillin. Which of the following prophylactic antibiotic regimens is most appropriate to prescribe?
A) Amoxicillin and clindamycin
B) Ciprofloxacin and metronidazole
C) Clindamycin only
D) Doxycycline and metronidazole
E) Trimethoprim-sulfamethoxazole and clindamycin
The correct response is Option E.
The most appropriate prophylactic regimen to prescribe in this clinical scenario is trimethoprim-sulfamethoxazole and clindamycin.
Dog bites to the hand are potentially dangerous bites that could lead to serious hand infections. The common microorganisms that cause infections in such bites are Pasteurella species, anaerobes, Staphylococcus aureus, and Streptococcus. The ideal antibiotic would have been amoxicillin-clavulanic acid, which covers most of these microorganisms. However, the child is allergic to penicillin, and, therefore, this drug is contraindicated. Another good option would have been amoxicillin and clindamycin (for the anaerobic coverage). However, for the same reason described above, it too cannot be used. Tetracyclines are contraindicated in children under 8 years of age owing to the ill effects on growing teeth and bones. Quinolones are also contraindicated in children under 18 years of age owing to their harmful effects on cartilage and joints. Although this is debatable, currently the use of quinolones in children is restricted by the Food and Drug Administration to certain specific conditions (cystic fibrosis, multidrug-resistant urinary tract infection, and inhalational anthrax). Clindamycin alone does not adequately cover most of the organisms involved, including Pasteurella, which is gram-negative.
2016
A 34-year-old woman comes to the emergency department 5 days after sustaining a cat bite to the left index finger. A photograph is shown. Medical history includes diabetes mellitus type 1. Physical examination shows punctures to the dorsum and volar surfaces of the proximal phalanx, mild fusiform swelling of the digit with tenderness over the flexor tendon sheath, pain with passive extension, and partially flexed posture of the digit. The symptoms have worsened over the past 3 days. Temperature is 99°F (37.2°C). Which of the following is the most appropriate next step in management?
A) Incision and drainage of the puncture sites
B) Inpatient intravenous antibiotics
C) Irrigation of the flexor sheath
D) Outpatient oral antibiotics
E) Splinting immobilization and elevation

The correct response is Option C.
The most appropriate option for this patient is to proceed to the operating room for decompression/drainage of the flexor tendon sheath. This patient has all four of Kanavel’s signs, specifically pain on passive extension, fusiform swelling, flexor tendon sheath tenderness, and flexion of the affected digit. These point towards a diagnosis of flexor tenosynovitis, with the cause being the cat bite she sustained several days prior. Although cat bites only reflect 5% of all animal bites, they represent 76% of all infected bites, thought to be because of the morphology of their long teeth, which simulate a deep puncture wound.
Outcomes studies demonstrate that because of this patient’s diabetes, she is at risk for a poor outcome, specifically the need for amputation and/or decreased total active motion. Other risk factors that can lead to these outcomes include age greater than 43 years, presence of subcutaneous purulence, digital ischemia, and polymicrobial infection. Given that she is at risk and that she has all four Kanavel’s signs, any intervention that is more conservative than operative decompression and drainage may lead to suboptimal outcomes.
Administration of antibiotics (orally or intravenously) is not a substitute for drainage of the flexor sheath, especially in a case that presents more than 48 hours out from initiation of symptoms. Drainage in the emergency department is not as optimal as in the operating room given that the infection may limit efficacy of local anesthesia as well as the need for possible conversion to an open drainage procedure if closed catheter irrigation is insufficient.
2016

A 60-year-old woman who works as a nurse in the intensive care unit (ICU) is scheduled for cardiac bypass surgery. Because she has taken care of many patients with methicillin-resistant Staphylococcus aureus infection, she is interested in topical agents for decolonization. Which of the following regimens is most appropriate for this patient?
A) Clindamycin
B) Linezolid
C) Mupirocin and chlorhexidine
D) Trimethoprim-sulfamethoxazole
E) Vancomycin
The correct response is Option C.
The currently accepted decolonization protocol from the Infectious Diseases Society of America is a combination of topical nasal mupirocin ointment and a chlorhexidine body wash for 5 days. The most robust data for decolonization are in the cardiac surgery literature; the Society of Thoracic Surgeons guidelines recommend routine prophylaxis for all patients undergoing cardiac surgery. These guidelines are based on studies that show a decreased rate of sternal wound infections.
The carriage rate of methicillin-resistant Staphylococcus aureus for health care workers is approximately 5% based on large review studies. As a substantial portion of cases originate from nasal colonization, routine screening and decolonization are recommended in areas where the carriage rate exceeds 10% (Centers for Disease Control and Prevention recommendation).
The other antibiotics listed are reserved for the treatment of infection rather than as part of a decontamination protocol.
2016
Which of the following antibiotics is most effective in decreasing Staphylococcus aureus infections in irradiated wounds?
A) Cefazolin
B) Doxycycline
C) Nafcillin
D) Trimethoprim-sulfamethoxazole
The correct response is Option D.
The prophylactic use of trimethoprim/sufamethoxazole (TMP/SMZ) in irradiated wounds, primarily in the setting of implant-based breast reconstruction, has been shown to reduce the rate of skin-derived infections. Mirzabeigi et al1 reported a 28% reduction in infection rates with the use of TMP/SMZ when compared with cephalosporins, in an irradiated chest wall wound. Based on their data, the authors advocate a monthlong prophylactic course of TMP/SMZ to reduce infection rates in this high-risk population. This is likely due to the ability of TMP/SMZ to treat both methicillin-resistant Staphylococcus aureus (MRSA) and Staphylococcus epidermidis. This has been supported by other published reports.2,3
Cefazolin and nafcillin do not effectively treat MRSA, reducing their clinical ability to prevent skin-related infections in this high-risk population. Doxycyline has some efficacy in treating most skin flora, including MRSA, but there is no clinical evidence to suggest it outperforms TMP/SMZ.
2016
A 15-year-old girl has two draining nodules of axillary hidradenitis suppurativa. Each lesion is approximately 10 mm in diameter. The remaining axillary skin shows no abnormalities. After a 6-week course of oral doxycycline and topical mupirocin, the lesions drain less but are still present. Which of the following is the most appropriate treatment for this patient?
A) Complete axillary excision and skin grafting
B) Excision and closure
C) Incision and drainage
D) Intravenous antibiotics
E) Kenalog injection
The correct response is Option B.
This young patient has limited, focal disease that has failed medical management. Local excision is useful for isolated, scattered individual, or linear lesions. More extensive disease that occupies a significant portion of the skin area may be better treated by complete axillary excision. In this younger patient with limited disease, direct excision of the affected areas is a less morbid approach. Negative pressure wound therapy and skin grafts may be optimal coverage treatments for extensive disease, and some local flaps have been described as well. This stubborn disease originates from the apocrine glands and can often be chronic and disabling. The axillae, groin, perineum, and submammary areas can all be affected. Initial treatments include local care, antibiotics, hygiene, and weight loss. Steroid injections may help in early, small lesions, but have limited effectiveness and are painful. After a 6-week course of antibiotics, this patient is not likely to benefit from more treatment. Only excision of the diseased apocrine glands is likely to be effective. Incision and drainage is a suitable treatment for a closed abscess associated with hidradenitis, but incising this patient’s lesions would not improve her situation.
2016
An otherwise healthy 10-year-old girl is brought for evaluation because of a chronic ulcer of the right leg. The ulcer first appeared 6 months ago when she scraped her leg on a boat dock at her family’s lake house. The wound has increased in size despite treatment with a course of oral antibiotic therapy prescribed by her primary care physician. A photograph is shown. On evaluation today, the patient is afebrile and has no systemic signs of infection. Which of the following organisms is the most likely cause of these findings?
A) Candida tropicalis
B) Group A beta-hemolytic Streptococcus
C) Methicillin-resistant Staphylococcus aureus
D) Mycobacterium marinum
E) Vibrio vulnificus

The correct response is Option D.
The history and presentation are classic for an atypical mycobacterial infection. Unlike bacterial infections, atypical mycobacteria rarely produce systemic signs of infection and often manifest as a nonhealing (sometimes progressive) wound. Given the history of injury on a boat dock, the most likely causative organism is Mycobacterium marinum, an acid-fast bacillus that lives in water environments. This pathogen results in localized granulomas such as the one seen in this patient. Staphylococcus aureus is the most common source of skin infections but typically results in a more pronounced and acute immune reaction with localized redness and purulence. These findings are not present in this patient. Cutaneous infections with Group A beta-hemolytic Streptococcus and Vibrio vulnificus tend to increase rapidly and are often accompanied by severe systemic response (i.e., necrotizing fasciitis). Candida tropicalis is a fungus that is often part of normal skin flora. It is related to Candida albicans and can produce opportunistic internal infections in susceptible individuals.
2016
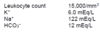
A 46-year-old woman comes to the emergency department because of a 5-day history of profound physical deterioration, nausea, and vomiting. She underwent breast reconstruction 3 weeks ago. Medical history includes delayed right latissimus dorsi tissue expansion breast reconstruction 1 year after completing radiation therapy. She has no other comorbidities. Physical examination shows erythematous rash involving and extending beyond the surgical sites. There are no notable fluid collections and the surgical wounds are not draining. Temperature is 103.5°F (39.7°C) and blood pressure is 90/50 mmHg. Laboratory studies show:
Intraoperative cultures of the explored surgical sites are most likely to grow which of the following organisms?
A) Bacteroides
B) Clostridium
C) Enterobacter
D) Pseudomonas
E) Streptococcus
The correct response is Option E.
The Centers for Disease Control and Prevention support criteria indicate that toxic shock syndrome may be diagnosed when patients present with a temperature exceeding 102°F (38.9°C), multisystems organ failure, rash, and/or multiple constitution symptoms.
Exotoxin1 and exfoliative toxin-producing Staphylococcus aureus are the most common pathogen, but enterotoxin A, B, and C, producing Streptococcus pyogenes infections, yield a worse prognosis. Blood cultures may be negative for the causitive organism.
Although Clostridium, Enterobactor, Pseudomonas, and Bacteroides species are polymicrobial species associated with necrotozing fasciitis, the description of this otherwise healthy patient is not consistent with its typical presentation of discolored blistered skin and crepitus.
2016
A 45-year-old man is brought to the emergency department with a Gustilo IIIB tibial fracture that he sustained falling off a tractor in a pasture. Medical history shows no drug allergies. Administration of which of the following antibiotics is most appropriate in this patient?
A) Amoxicillin
B) Ceftriaxone
C) Ciprofloxacin
D) Clindamycin
E) Vancomycin
The correct response is Option B.
The most appropriate antibiotic prophylaxis for this patient with a Gustilo grade III fracture is a third generation cephalosporin. Although much debate exists regarding antibiotic prophylaxis in open tibial fractures, it is generally accepted that antibiotic prophylaxis reduces the rate of infection. When antibiotic prophylaxis is not used, infection occurs in approximately 24% of open fractures. Thus, selecting the appropriate antibiotic, as well as duration, is of utmost importance. Antibiotic prophylaxis should be administered as soon as possible after injury and should be limited to a 72-hour course. In general, broad-spectrum antibiotics and multiple antibiotics should be avoided because they have been shown to increase the risk of nosocomial infections, including pneumonia. Of the antibiotics listed, the most appropriate choice for a patient with no drug allergies is ceftriaxone. Clindamycin and vancomycin should be reserved for cases of true penicillin allergy. Ciprofloxacin alone has been shown to be inferior to prevent infection after open tibial fractures.
2016
A 29-year-old woman is evaluated because of a 2.5-year history of painful, draining lesions from the axillae and groin. Physical examination shows multiple nodules and abscesses. Conservative treatment with loose clothing, topical antibiotics, and antibacterial washes is unsuccessful. These findings are most consistent with which of the following disease processes?
A) Candidal infection of the intertriginous areas
B) Follicular occlusion of the apocrine sweat gland areas
C) Follicular occlusion of the eccrine sweat glands areas
D) Inflammatory and ulcerative skin condition mediated by neutrophils
E) Sexually transmitted infection caused by Klebsiella granulomatis
The correct response is Option B.
Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic inflammatory disease of the skin and subcutaneous structures. Initially presenting as tender, subcutaneous nodules, the disease can advance to cause abscesses and large areas of subcutaneous scarring and draining sinus tracts.
Historically, HS has been thought to originate from the apocrine sweat glands. However, research in recent years has demonstrated that the mechanism is one of follicular occlusion: hair follicles become occluded due to an overproliferation of ductal keratinocytes, rupture, and subsequently re-epithelialize. As this cycle continues, sinus tracts form that house bacteria and cause chronic, painful infections and inflammation that can involve the skin and subcutaneous structures including muscle, fascia, and lymph nodes.
HS lesions typically occur predominately in the apocrine-gland bearing areas of the axillary, inguinal, perianal, and perineal areas. Lesions typically correspond with the “milk-line” pattern of apocrine-related mammary tissue in mammals.
Eccrine, or merocrine, sweat glands are found throughout the body, but their highest concentrations are in the palms and soles. These areas are typically spared by HS.
Follicular pyodermas, including folliculitis, furuncles, and carbuncles, arise primarily from the infection of hair follicles. They do not cause the sinus tracts, comedones, and scarring caused by HS.
Granuloma inguinale is a sexually transmitted infection of the genitalia, perineum, and/or perineal area caused by Klebsiella granulomatis.
Pyoderma gangrenosum is a dermatologic condition mediated by neutrophils that causes skin ulceration and breakdown.
2016
A 5-year-old boy is brought to the emergency department after sustaining a traumatic amputation of the right thumb. Medical history includes an allergy to sulfa drugs. The thumb is successfully replanted, and the patient is admitted for observation. Twenty-four hours postoperatively, venous congestion of the replanted thumb is noted. Leeches are placed to improve congestion. It is suspected that the leeches will be required for several days until venous outflow is reestablished. Administration of which of the following antibiotics is most appropriate?
A) Cefotaxime
B) Ciprofloxacin
C) Clindamycin
D) Tetracycline
E) Trimethoprim-sulfamethoxazole
The correct response is Option A.
Medicinal leeches are still commonly used as an adjunct in the treatment of venous congestion. They secrete a powerful anticoagulant called hirudin that promotes bleeding in the congested tissues until venous outflow can be reestablished. Leeches are also known to harbor the gram-negative bacterium Aeromonas. Because leeches can be exposed to open wounds on the patient for several days during treatment, antibiotic prophylaxis against Aeromonas is recommended.
Ciprofloxacin, tetracycline, trimethoprim-sulfamethoxazole (Bactrim), and third-generation cephalosporins have all been shown to be effective against Aeromonas. However, in the scenario above, all of these antibiotics have a contraindication except cefotaxime, a third-generation cephalosporin.
Ciprofloxacin is contraindicated in children when a suitable alternative exists secondary to the risk of arthropathy and arthrotoxicity. Similarly, the use of tetracycline is relatively contraindicated in children owing to the potential for abnormalities with the teeth, including permanent staining and growth retardation. While Bactrim is often used in children to treat various infections, this child has an allergy to sulfa drugs and should not be given this antibiotic.
Clindamycin does not provide effective antibiotic coverage against Aeromonas.
2016









