Sex Hormone Therapies Flashcards
(14 cards)
Outline the intermediate steps present in the formation of estrogens and androgens

In what conditions are oestrogen hormone replacement therapy indicated?
_Children _
- Hypogonadism
- Development of secondary sex characteristics and accelerates growth
_Adult _
- Primary amenorrhoea + progestin
- Contraceptive + progestin
- Menopause
- Oestrogen (Hormone) replacement
- progestin
- Oestrogen (Hormone) replacement
What are the benefits of post menopausal hormone therapy?
- **Improved bone density **
- Decreases bone resorption
-
Relief from flushes, fatigue & vaginal dryness
- Re-establishes feed-back control
- **Reverses atrophy of vulva, vagina, urethra **
- Improved sleep
- Reduced incidence of colorectal cancers
- **Cardiovascular **
- Reduced incidence coronary heart disease?
- Depends on trial
- Reduced incidence coronary heart disease?
-
Reduced incidence / delay onset of Alzheimer’s?
- Observational
What are the risks of postmenopausal hormone therapy?
_Breast tenderness, nausea & fluid retention _
_Increased risk of breast / uterine cancer _
- progestin (+/-)
_Cardiovascular _
- Increased risk of thromboembolism / stroke
Note: Controversy remains but benefits believed to outweigh risks.
- Risk assessment
- Timing post menopause
- Drugs with tissue specific effects.
Characterise Estrogen mechanisms of action
There are 3 different endogenous estrogen steroids:
Oestriol <-> Oestrone <-> Oestradiol
These different estrogen steroids have different affinities to the different subtypes of estrogen receptors -> get tissue specific effects
ER-alpha and ER-beta
These receptors are present in the nucleus of cells -> leads to the formation of homo- or heterodimers that associate with transcription factors -> gene expression or repression
ALSO:
Estrogens capable of acting at ER at the cell surface and GPCRs to produce more rapid effects (particularly to intracellular calcium)
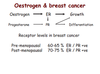
What is the hormonal association between oestrogen and breast cancer?
Estrogen receptor activation leads to cellular growth + upregulation of progesterone receptor
The progesterone receptor itself is stimulated to result in cellular growth and differentiation
Thus, estrogen was implicated as an important regulator of breast cancers. Breast tumours were:
Pre-menopausal 60-65 % ER & PR positive
Post-menopausal 70-75 % ER & PR positive
What are selective receptor modulators (SERMs)?
Drugs that selectively react with oestrogen receptors (not other steroid or GPCR receptors)
There are two classes used as a hormone therapy in sex-specific female cancers:
partial agonists and antagonists

Characterise the actions of tamoxifen
Tamoxifen is a partial agonist of estrogen receptors in tissue-specific sites throughout the human body
Palliative treatment of metastatic breast cancer &
adjuvant after lumpectomy
Antagonist in breast but partial agonist in bone and
endometrium
Adverse Effects:
- Endometrial hyperplasia, polyps & cancer
- Thromboembolic events
- Thrombocytopenia
- Ocular toxicity
- Menopausal symptoms
- Hot flushes, atrophic vaginitis
- Resistance to hormone therapy may develop
– Tumours may recur

What is the rationale of aromatase inhibitor therapy in breast cancer?
Aromatase enzymes demonstrate increased activity in breast adipose mesenchymal cells -> elevating oestrogen levels
These elevated levels of oestradiol may occur locally as a paracrine hormone and thus not contribute to serum detectable oestradiol in the women’s circulation -> particularly post menopausal women and men
Aromatase inhibitors improve disease free survival after tamoxifen treatment. It reduces:
- incidence of contralateral breast cancer
- number of thromboembolic events
- incidence of endometrial cancer
But adversely results in:
- Increased bone loss & fracture risk
- Increased arthralgia
- Potential poorer lipid profile, hepatic steatosis & metabolic syndrome with long-term use
- Menopausal signs
What androgens are present within the human body?
Androgens testosterone and dihydrotestosterone are synthesised and have anabolic and masculinising effects in both males and females
The cytoplasmic enzyme 5α-reductase synthesizes DHT in the prostate, testes, hair follicles, and adrenal glands from testoseterone
They activate specific nuclear androgen receptors to alter gene transcription via GRE elements.
Synthetic forms of the adrogens have modified solubility and metabolism; as well as being synthesised to have specific anabolic or androgenic effects
What are the uses of androgens as therapeutic treatments?
Androgenic treatment:
- Hypogonadism
Anabolic treatment:
- Senile osteoporosis
- Spedy recovery from surgery / chronic debilitating diseases
Growth
- Pituitary Dwarfism
Non-therapeutic:
- Increase lean body mass, muscle strength and aggressiveness
What are the adverse effects of androgens in the body?
_Increase LDL & decrease HDL _
Increase risk of coronary heart disease
_Females _
Acne, facial hair, deepening of voice, male pattern baldness, excessive muscle development & menstrual irregularities
_Males _
Priapism, impotence, decrease spermatogenesis &
gynaecomastia
_Children _
Premature closure of epiphyseal plates, abnormal sexual
maturation
Athletes
Liver damage, increased aggression and psychotic episodes
Discuss three common anti-androgen treatments and their indications
Androgen Receptor Antagonists
_Cyproterone (steriodal antagonist) _
Used in prostate cancer and androgenisation in females
Adverse effects include:
- Cognitive changes, fatigue, oedema
- Reduced spermatogenesis
Flutimide (non-steroidal antagonist)
Used in metastatic prostate cancer
Adverse effects include:
- Diarrhoea, anemia, hepatic injury
- Oedema, dizziness, blurred vision
Finasteride (5a-reductase inhibitors)
Used in benign prostatic hypertrophy and hair loss
Adverse effects include:
- Impotence, decreased libido and ejaculation disorders
- Breast enlargement, tenderness
- Breast cancer has been reported


