Session 9 Flashcards
Factors effecting STI transmission

Burden of STI/problems with having STIs

How can STIs present?

Give examples of bacteria, viruses, parasites, fungi & Protozoa causing STIs

What investigations can you perform for STI in men?
first pass urine (men only) – urethral GC/CT (can be sent in white universal pot)
vulvo-vaginal swab – vaginal/cervical GC/CT (use chlamydia swab pack and break pink swab tip into NAAT medium)
pharyngeal swab – GC/CT of the throat (use plain purple swab and break tip into NAAT medium)
rectal swab – GC/CT of the rectum (send as for pharyngeal swab)

What investigations would you perform in women?
All of these samples can be self-taken. Rectal swabs should be introduced approx. 2cm into the rectum, rotated against the rectal wall, and removed. Vulvo-vaginal swabs should be inserted as far into the vagina as possible, and swept along the vaginal walls and vulva as they are removed to maximise sample volume.
Additional tests for symptomatic patientsmay include the following:
urethral discharge – charcoal swab to microbiology requesting Gonococcal culture
vaginal discharge – charcoal swab from cervical os for Gonococcal culture; additional charcoal swab from posterior fornix for Trichomonas vaginalis and Candida culture
oral/genital ulceration – green viral swab for herpes simplex virus (HSV) 1 and 2 PCR
anal discharge – charcoal swab for Gonococcal culture, HSV swab if significant anorectal discomfort
conjunctivitis – GC/CT NAAT from conjunctiva; charcoal swab for Gonococcal culture if significant purulent discharge.

Chylamydia trachomatis

Niesseria gonorrhoea

Symphilis

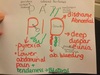
HSV presentation
Ulcer base specific type serology

Trichomonas vaginalis

How to treat scabies and pubic lice
- Features of scabies
- Management
- The BNF advises to apply the insecticide to all areas, including the face and scalp, contrary to the manufacturer’s recommendation. Patients should be given the following instructions:
Image below is Norwegian scabies

skin contact
scabies mite lays its eggs in the stratum corneum. The intense pruritus associated with scabies is due to a delayed type IV hypersensitivity reaction to mites/eggs which occurs about 30 days after the initial infection.
1.
- widespread pruritus
- linear burrows on the side of fingers, interdigital webs and flexor aspects of the wrist
- in infants the face and scalp may also be affected
- secondary features due to scratching: excoriation, infection
2.
permethrin 5% is first-line
malathion 0.5% is second-line
pruritus persists for up to 4-6 weeks post eradication
3.
- apply the insecticide cream or liquid to cool, dry skin
- between fingers and toes, under nails, armpit area, creases of the skin such as at the wrist and elbow
- allow to dry and leave on the skin for 8-12 hours for permethrin, or for 24 hours for malathion, before washing off
- reapply if insecticide is removed during the treatment period, e.g. If wash hands, change nappy, etc
- repeat treatment 7 days later

What is this image showing

HPV - anogential warts
6 11 non harmful
16 18 harmful - cervical cancer

Bacterial vaginosis

Vulvovaginal candidiasis