Session 8: Functional Anatomy of the Eye Flashcards
(99 cards)
Describe the bones forming the walls of the orbit, particularly in relation to those most vulnerable to fracture in orbital injuries i.e. orbital blow out fracture, & the clinical manifestations of such an injury. LO
- What shape is the orbit? Contains?
- The orbit can be thought of as a pyramidal structure, with the apex pointing posteriorly & the base situated anteriorly. The boundaries of the orbit are formed by how many bones?
- It is also important to consider the anatomical relations of the orbital cavity – this is clinically relevant in the ?
- pyramidal
eyeball, its muscles, nerves, vessels and most of the lacrimal apparatus - seven bones
- spread of infection, and in cases of trauma
Q. The borders and anatomical relations of the bony orbit are as follows: ( roof, floor, medial and lateral wall, apex, base)
A. Roof (superior wall) –frontal bone & the lesser wing of the sphenoid. The frontal bone separates the orbit from the anterior cranial fossa.
Floor (inferior wall) –maxilla, palatine and zygomatic bones. The maxilla separates the orbit from the underlying maxillary sinus.
Medial wall – ethmoid, maxilla, lacrimal and sphenoid bones. The ethmoid bone separates the orbit from the ethmoid sinus.
Lateral wall –zygomatic bone & greater wing of the sphenoid.
Apex – Located at the opening to the optic canal, the optic foramen.
Base – Opens out into the face, and is bounded by the eyelids. It is also known as the orbital rim

Q. What are the three bony openings arising from/towards the apex of the orbit?
A. Superior orbital fissure
Inferior orbital fissure
Orbital canal
Q. 1. Which bones (and therefore walls) of the orbit are the weakest and thus most vulnerable to fracture in orbital trauma?
- Why are the bones/walls you have listed in 1.3 the most easily fractured?
- What structure is found within the lacrimal fossa (see image above), in the anteromedial part of the orbit?

A.1. Maxilla (floor)
Maxillary, ethmoid, lacrimal (medial)
2.air filled sinuses thus are thin
3.

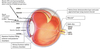
Q. Cornea: this is the main refractor of the eye; why do you think it is avascular?
Does the cornea have a conjunctival membrane?
A.transoarent
Yes
Q. What are the two muscles of the iris ?
A. Iris sphincter/constrictor, iris dilator, ciliary
- What are the two muscles of the iris ?
- What structure delineates the anterior chamber from the posterior chamber?
- What is found in these chambers?
- Iris sphincter/constrictor, iris dilator, ciliary
- Iris
- Aqueous humour (then where is vitreous?)
Q. How does it exit the eye?
A. • Drains through iridocorneal angle (between iris & cornea)
• Via trabecular meshwork into canal of Schlemm (circumferential venous channel draining into venous circulation)
Muscle:
Levator palpebrae superioris
Palpebral part of orbicularis oculi
Superior tarsal muscle
State their: Nerve supply Action Consequence of damage



Q. The bony orbit contains the eyeballs and their associated structures: (5) (i.e. what else does the orbit contain?
A. Extra-ocular muscles – These muscles are separate from the eye. They are responsible for the movement of the eyeball and superior eyelid.
Eyelids – These cover the orbits anteriorly.
Nerves: Several cranial nerves supply the eye and its structures; optic, oculomotor, trochlear, trigeminal and abducens nerves.
Blood vessels: ophthalmic artery (primarily). Venous drainage is via the superior & inferior ophthalmic veins.
Any space within the orbit that is not occupied is filled with orbital fat. This tissue cushions the eye, and stabilises the extraocular muscles.


- What do the eyelids (palpebrae) contain
- There are three main pathways by which structures can enter and leave the orbit: (3) strate what these structures transmit
- – Protect the eye when palpebral fissure is closed (Contain fibrous structures)
– Tarsal plates and muscles
– Glands at the edges of the eyelids (Can block) - Optic canal: optic nerve & ophthalmic artery
Superior orbital fissure: lacrimal, frontal, trochlear (CN IV), oculomotor (CN III), nasociliary and abducens (CN VI) nerves. It also carries the superior ophthalmic vein.
Inferior orbital fissure: maxillary nerve (a branch of CN V), the inferior ophthalmic vein, and sympathetic nerves.
Q. 1. Main arterial supply is ?
- Venous drainage?
- State the nerve for General sensory from the eye (including conjunctiva, cornea)
- State the nerve for Special sensory vision from retina
- State the nerve for Motor nerves to muscles
A. 1. ophthalmic artery and its branches
- Ophthalmic veins drain venous blood into cavernous sinus, pterygoid plexus and facial vein
- Optic
- Oculomotor, sensory and abducens


- There are other minor openings into the orbital cavity:
- What bones are most vulnerable to fracture in orbital injuries
- Nasolacrimal canal, which drains tears from the eye to the nasal cavity, is located on the medial wall of the orbit.
supraorbital foramen and infraorbital canal – they carry small neurovascular structures. - maxillary and ethmoid
Q. Clinical Relevance: Fractures of the Bony Orbit. There are two major types of orbital fractures:
A. Orbital rim fracture & ‘Blowout’ fracture
Q. What is an orbital rim fracture?
A. This is a fracture of the bones forming the outer rim of the bony orbit. It usually occurs at the sutures joining the three bones of the orbital rim – the maxilla, zygomatic and frontal.
Q. What is a blow out fracture?
A. partial herniation of the orbital contents through one of its walls. This usually occurs via blunt force trauma to the eye. The medial and inferior walls are the weakest, with the contents herniating into the ethmoid and maxillary sinuses respectively.
Q. Which bones are susceptible in an orbital blowout fracture
A.

Trying to look up
Can’t due to anchoring of the inferior contents
Not due o the muscl e
Eye can’t physically look up
Bottom of orbital contents is trapped
Orbital contents and blood can prolapse into maxillary sinus; the fracture site can ‘trap’ structures e.g. soft tissue, extra orbital muscle located near floor or orbit
Q. Signs of blowout fracture
A. • Periorbital swelling, painful
• Double vision (especially on vertical gaze)
• Impaired vision
• Anaesthesia over affected cheek (upper teeth & gums) on affected side
(Numbness over the cheek
Cutaneous branches of the maxillary division
Infraorbital nerve runs through the floor of the orbit
Comes out through the infraorbital foramen to innervate the check)
- Cause of blowout fracture
- Investigations for blowout fractures
- Sudden increase in intra-orbital pressure (e.g. from retropulsion of eye ball [globe] by fist or ball) fractures floor of orbit
Orbital contents and blood can prolapse into maxillary sinus; the fracture site can ‘trap’ structures e.g. soft tissue, extra orbital muscle located near floor or orbit
- Plain Radiography & Coronal View (CT)

- What clinical sign will you witness in both of these fractures and why.
Any fracture of the orbit will result in intraorbital pressure, raising the pressure in the orbit, causing exophthalmos (protrusion of the eye). There may also be involvement of surrounding structures, – e.g haemorrhage into one of the neighbouring sinuses.