Session 5: The Female Reproductive System Flashcards
Describe the ovaries and their capsule
[*] The paired human ovaries are slightly flattened, almond-shaped and sized organs attached to the posterior surface of the broad ligament of the uterus by the mesovarium.
- The mesovarium is a short peritoneal fold or mesentery.
- Medially within the mesovarium, a short ovarian ligament tethers the ovary to the uterus.
- The ovarian ligament is a remnant of the superior part of the ovarian gubernaculum.
[*] The connective tissue capsule of the ovary, the Tunica Albuginea of the Ovary, is covered with a smooth layer of ovarian mesothelium that has a dull grayish appearance. This epithelium becomes progressively scarred and distorted because of the repeated rupture of ovarian follicles and discharge of oocytes during ovulation.
What do the ovaries contain?
[*] The outer cortex contains many follicles, each containing an oocyte (the female gamete) surrounded by stromal cells called the follicular cells.
- The oocytes originate outside the ovary from the primordial germ cells that colonize the ovary during early embryonic development.
[*] The gonads develop within the mesonephric ridge and descend through the abdomen before stopping in the pelvis. They become stuck because the newly forming uterus is a mechanical barrier, stopping the ovary’s progress through inguinal canal. The inferior pole of the ovary is connected by gubernaculum to the labioscrotal folds and the mesonephric ducts fuse to form the uterus, which is responsible for stopping the ovaries descent.
[*] In the ovary, the oocytes divide by mitosis to form oogonia, which develop into oocytes by undergoing meiosis. Although meiosis commences during fetal life, it is not totally completed until fertilization.
[*] During development, the fetal ovary contains several millions of oogonia which commence meiosis but not all of which complete it to form primary oocytes. The cell division does not progress beyond the diplotene stage of the 1st meiotic prophase until just before ovulation. At ovulation, the 1st meiotic division occurs to produce a haploid secondary oocyte and the 1st polar body.
The oocytes are surrounded by a layer of flattened stromal cells – the follicular cells; this structure is called a primordial follicle. Many follicles undergo degeneration (atresia) in the fetal and postnatal ovary, however up to 400,000 persist at puberty.
[*] The bulk of the human ovary consists of primordial follicles, each consisting of a large round primary oocyte with an eccentrically placed pale-staining nucleus, surrounded by a single layer of follicular cells. About 400 of these will develop fully and shed their ova periodically until menopause.
What 2 types of follicle populations do the ovaries contain from puberty up until menopause?
[*] After puberty and up to menopause, the human ovary contains two populations of follicles.
- By far the larger of the two is a reserve pool of non-growing follicles and a smaller pool of growing follicles derived periodically from the former groups.
It is thus obvious that the reserve pool is constantly depleted and is normally exhausted about the age of 50-55.
The reserve pool contains mainly primordial follicles and follicles that have a layer of follicular cells (granulosa) which are becoming cuboidal.
- Folliculogenesis: entry of follicles into the growth phase and their subsequent development
- Of the growing follicles, only one is normally destined to mature fully during each menstrual cycle to release its gamete (ovum) at ovulation; others undergo degeneration
How are growing and mature follicles classified?
[*] Growing and mature follicles are classified as primary, secondary (or Graafian) or tertiary (or pre-ovulatory) the latter being the largest.
- A primordial follicle slowly transforms into a primary follicle by transformation of the single layer of flattened follicular cells into a layer of cuboidal granulosa cells.
- Glycoproteins that contribute to the formation of the zona pellucida surrounding the oocyte, appear at this time and form a thick amorphous layer as the follicle grows.
- Further follicular growth involves the granulosa cells forming a layer of multiple layers and transformation of the surrounding stromal cells into theca folliculi, which comprises of a cellular theca interna and a fibrous theca externa. These follicles are called secondary pre-antral follicles.
- Appearance of a fluid-filled cavity (antrum), signals the formation of a tertiary or antral follicle. These follicles enlarge by an increase in the fluid volume and proliferation of the granulosa and thecal cells; Graafian follicles are large antral follicles and only one of the most advanced of these will become the ovulatory follicle.
How does the Corpus Luteum form?
Corpus Luteum: when the follicle ruptures to release the ovum at ovulation, the granulosa and theca interna cells show structural (and functional) transformation.
[*] The entire mass of the tissue becomes highly vascularised via the growth and infiltration of blood vessels from the surrounding tissue.
[*] Granulosa cells of the follicle have undergone hypertrophy and form a thick and folded layer of granulosa lutein cells which have a spherical nucleus and pale-stained vacuolated cytoplasm containing numerous lipid droplets.
[*] The theca interna cells have become transformed into theca lutein cells and occupy the depressions formed by the granulosa lutein cells, accompanied by blood vessels.
[*] The central cavity of the corpus luteum contains mainly undifferentiated connective tissue.
Describe the arterial supply, venous drainage and lymphatic drainage of the ovaries
Arterial Supply of the Ovaries
[*] The ovarian arteries come directly off the abdominal aorta, just below the renal arteries. They travel through retroperitoneum.
Venous Drainage of the Ovaries
[*] Venous drainage of the ovaries is asymmetrical, by the left and right ovarian veins
- Right ovarian vein => inferior vena cava
- Left ovarian vein => left renal vein => inferior vena cava
Lymphatic Drainage of the ovaries: lymphatic drainage of the ovaries is to the Para-aortic nodes.

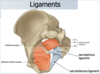
What ligaments are associated with ovaries?
[*] The ovarian ligament (ligament of ovary) is attached to the ovary inferiorly and connects the ovary to the side of the uterus.
- Structurally, it is a fibrous band of tissue that lies within the broad ligament.
- It joins the uterus just below the origin of the fallopian tubes.
[*] The suspensory ligament of ovary extends outwards from the ovary to the lateral abdominal wall. It consists of a fold of peritoneum, thus some sources consider it to be part of the broad ligament. The function of this ligament is to contain the ovarian vessels and nerves (ovarian artery, ovarian vein, ovarian nerve plexus and lymphatic vessels)

Describe the common pathology relevant to the ovaries
[*] The ovary may develop ovarian cysts, which are usually derived from follicles. Polycystic ovaries (with >10 cysts) are usually associated with infertility.
[*] The tumours of the ovary arise most commonly from epithelial components or from germ cells
What are the parts and function of the uterine tubes?
The Uterine Tubes (Fallopian tubes, oviducts)
[*] The uterine tube is a muscular tube that is narrow medially and has a funnel-shaped abdominal opening (near the ovary), the ostium. The margins of the ostium are drawn into finger-like projections called the fimbria, an extension of the infundibulum.
[*] The infundibulum, continues medially into an expanded intermediate segment, the ampulla.
[*] The tube continues into the narrow isthmus and opens into the uterine cavity. The function of the tube is to assist in the transfer and transport the ovum from the ovary to the uterine tube and then to the uterus.

How does the uterine job perform its function?
[*] Histologically, at low magnification the wall of the tube is seen to consist of a mucous membrane, a muscular layer and a serous coat
- The mucous membrane is thrown into complex folds and thus the lumen, in cross-section, appears as a labyrinthine system of narrow spaces.
- The epithelium lining the mucous membrane is of a simple columnar type and consists of ciliated and non-ciliated (secretory ) cells. The secretory cells provide the nutrients to the early conceptus following fertilization. As it is not the same as the endometrium of the uterus, there are consequences in ectopic pregnancies.
[*] The movement of the fimbria over the surface of the ovary and the ciliated cells (lining the tube) are thought to assist in the transfer of the ovum from the surface of the ovary into the uterine tube. Normally the site of fertilisation is in the ampulla.
[*] The contractions of the smooth muscle layer assists in the **transport of sperm to the site of fertilization and the transport of the conceptus to the uterus. **
What is salpingitis and describe its possible consequences
Clinical Correlation: inflammation of the uterine tube, caused by microorganisms, is called salpingitis.
[*] It causes fusions or adhesions of the mucosa, and thus can partially or completely block its lumen leading to infertility.
[*] Blocked or dysfunctional tubes may result in ectopic pregnancy (tubal) or implantation outside the uterus.
Describe the parts of the uterus, locaiton and its relationships (anatomical)
[*] The uterus consists of the fundus, body, uterine tubes and cervix.
[*] The fundus lies superior to the pubic ramus and is not normally palpable but becomes palpable when uterus enlarges, entering the abdominal cavity – upper part is examined during pregnancy
[*] Relationships of the Uterus. The uterus is enveloped by the broad ligament (specialised peritoneum)
- Uterovesical pouch anteriorly (between uterus and urinary bladder)
- Rectouterine pouch (pouch of Douglas) posteriorly (inferior most recess of the peritoneal cavity).
The Pouch of Douglas is accessible through the posterior fornix of the vagina

Describe the development of the uterus and the creation of the broad ligament
- Paramesonephric ducts (a pair of ducts that are open cranially and connect to the urogenital sinus caudally) persist in the absence of (testis-derived) MIH.
- Fusion of the ducts in the midline creates a broad transverse fold draped by peritoneum => broad ligament which contains the uterus, uterine tubes and ovaries etc (intraperitoneal structures)

Describe the uterus including the myometrium and the endometrium
[*] The uterus is a thick-walled muscular organ covered for the most part by serous membrane, the peritoneum.
[*] The greater part of the uterine wall is a mass of smooth muscle, the myometrium. The cells of the myometrium undergo considerable hypertrophy and hyperplasia during pregnancy in preparation for the requirements to expel the foetus at birth.
[*] Internally the uterine cavity is lined by mucous membrane, the endometrium
- The endometrium consists of tubular glands that extend from the surface into the connective tissue (stroma).
- Most of the superficial part of the endometrium (called the stratum functionalis = functional layer) is subject to cyclical growth, degeneration and shedding of the dead tissues.
- The deeper part of the endometrium (stratum basalis = basal layer) in the vicinity of the myometrium does not exhibit the cyclical changes and is responsible for the regeneration of the upper endometrium.
Describe how the cyclical changes of the endometrium are regulated
The hormones secreted by the ovary regulate the cyclical changes in the structure of the endometrium.
- Oestrogen secreted during the folliculogenesis stimulates growth and proliferation of the endometrium; this is the proliferative phase of the endometrium.
- After ovulation, the newly formed corpus luteum secretes progesterone, which stimulates the endometrial glands to secrete glycogen, and causes their extensive coiling and enriches the vascular supply to the mucous membrane. This is the secretory phase of the endometrium.
- These changes in the endometrium are in preparation for the receipt and embedding (implantation) of the conceptus following fertilization.
If the conceptus fails to implant, the endometrium enters the menstrual phase, which is brought about by the withdrawal of hormonal support (degeneration or luteolysis of the corpus luteum) and changes in the vascular supply of the endometrium. This results in the breakdown and degeneration of the bulk of the upper endometrium (statum functionalis), bleeding and the shedding of the dead tissues; these constitute the production of menses.
Describe the uterus in the proliferative phase
- The bulk of the organ is composed of bundles of smooth muscle fibres.
- The endometrium is covered by an epithelium overlying the stroma containing uterine glands forming the functional layer
- The uterine glands are long, narrow and straight and often slightly dilated.
- In the deepest part of the endometrium (basal layer), the glands show some bifurcation in the zone adjacent to the myometrium and occasionally they penetrate a short distance among the muscle bundles.
- The epithelium lining the uterine cavity and the glands is simple columnar and is composed of a mixture of ciliated and secretory cells.
- Numerous mitoses are evident in the epithelium (particularly in the epithelium lining the glands) and in the endometrial stroma
- The stroma consists of stellate cells surrounded by a fine reticular network
- The arteries (called spiral or coiled arteries) are mostly located in the lower part of the endometrium and appear transversely sectioned.
Describe the uterus in the secretory phase
- The endometrial glands have enlarged to become more tortuous and have developed marked sacculation, resulting in a relatively wide lumen of irregular outline containing secretion.
- The endometrial stroma appears oedematous and some of the stromal cells have undergone hypertrophy.
- The blood supply to the endometrium has become more extensive and the arteries are now present in the superficial regions too.
- The histology of the basal layer of the endometrium remains essentially unaltered
Describe the endometrium in the menstrual phase
The upper endometrium has undergone extensive necrosis and shows ruptured blood vessels.
Describe the position of the uterus
Anteflexed in relation to the cervix (angle of inclination)
Anteverted in relation to the vagina

What ligaments support the uterus?
The ligaments of the uterus:
- The superior aspect is supported by the broad ligament and the round ligaments.
- The middle aspect is supported by the cardinal, pubocervical and uterosacral ligaments.
- The inferior aspect of uterus is supported by the structures in the pelvic floor: the levator ani, perineal membrane and perineal body.
Describe the broad ligament including its parts
[*] Broad ligament: double layer of peritoneum (mesentery) [peritoneal fold] that extends from the sides of the uterus to the lateral walls and floor of the pelvis. It folds over the internal female genitalia, covering their surface anteriorly and posteriorly. It is comprised of the mesentery of the uterus, uterine tube and ovary. The broad ligament assists in keeping the uterus in position. It may be divided into 3 subcomponents
- Mesometrium – the mesentery of the uterus; the largest portion of the broad ligament. It runs laterally to cover the external iliac vessels, forming a distinct fold over them. It also encloses the proximal part of the round ligament of the uterus.
- Mesosalpinx – the mesentery of the Fallopian tube. It originates superiorly to the mesovarium, enclosing the fallopian tubes.
- Mesovarium – the mesentery of the ovaries. It projects from the posterior surface of the broad ligament and attaches to the hilum of the ovary, enclosing its neurovascular supply. It does not, however, cover the surface of the ovary itself.

What are the contents of the broad ligament?
[*] Contents of the broad ligament: uterine tubes, ovary (some sources consider the ovary to be on the broad ligament but not in it), ovarian artery (in the suspensory ligament), uterine artery, ovarian ligament, round ligament of uterus and suspensory ligament of the ovary.
Describe the Round Ligament
The round ligament is the second embryological remnant of the (inferior part) gubernaculum. The round ligament originates at the uterine horns – the point at which the fallopian tubes enter the uterus) and the labium majus as well as travelling through the inguinal canal.
- This gives consequences to the lymphatic drainage of the uterus – the fundus drains to the aortic nodes (where it is embryologically derived from)
- The round ligament can be a source of pain during pregnancy due to increased force placed on the ligament by the expanding uterus.

What is Endometriosis?
[*] Endometriosis is a condition in which ectopic endometrial tissue is dispersed to various sites along the peritoneal cavity and beyond (e.g. near to the umbilicus). It may be associated with the ovaries or the attachments of the uterus and is often associated with severe period pain (dysmenorrhoea), infertility or both.