*Seizure Flashcards
Scenario: You are bleeped by one of the staff nurses to review a patient on the orthopaedic ward who is “jerking in her bed”. She tells you the patient is a 74-year-old female who is 2 days post knee replacement. She is a known epileptic who takes sodium valproate daily but has not taken any for the past 2 days because she has been feeling nauseous from the opioids she has been taking post-operatively and can’t keep anything down.
Arrive at the scene… What do you do to manage the deteriorating patient in the first 5 minutes?
- Pull emergency buzzer
- Start a timer
- ABCDE
Meanwhile, if someone else is available, ask that they:
- Obtain IV access & take bloods
- Blood glucose
- Get your local protocol for benzodiazepines (usually IV lorazepam or PR diazepam or buccal midazolam)
- Obtain the notes & drug chart for the patient & start documenting
How do you assess airway in a seizure?
Signs of airway occlusion:
- Paradoxical chest and abdominal movements (see-saw movement)
- Patient looking blue/cyanosed (late sign)
- Depressed consciousness
If occluded perform airway manoeuvres (head tilt, chin lift and applying adjuncts) & put an emergency call out
Apply 15L of oxygen via non-rebreathe mask regardless of airway occlusion
How do you assess breathing in seizure?
- Auscultate breath sounds
- What is their respiratory rate?
- What are their saturations?
- Give 15L/min via non-rebreather mask regardless of comorbidties
Remember: Hypoxia kills before hypercarbia e.g. in COPD patients who are CO2 retainers will still die of tissue ischaemia first.
NB: switch to venturi in COPD pateints so that oxygen requirement can be titrated appropriately
What types of airways can be used if the patient has not been able to maintain their own airway?
Head-tilt chin-lift maneouvre OR jaw thrust
The following can be used in conjunction with the above as the position of the head and neck still need to be maintained:
- NPA
- Guedel ororpharyngeal airway
What is the difference between the head tilt chin lift and jaw thrust?
Jaw thrust is performed where there is severe trauma with potential spinal involvement

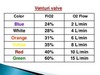
What are the venturi mask colours and their oxygen flows?
What oxygen requirement needs referral to med reg?
10L/min high flow oxygen or greater to maintain sats over 94%
What is the relationship between the FiO2 and pO2 in kPa?
pO2 is roughly 10 units less than the inspired oxygen (FiO2). For example, on FiO2 60%, someone who was not having any issues with gas exchange or oxygen delivery would have a PO2 of 50KPA.
How do you assess circulation in seizures?
- capillary refill
- BP –> correct any hypotension with fluids
- pulse rate
- obtain IV access
- bloods : VBG, FBC, U&Es, LFTs, clotting, group&save, bone profile, magnesium
- consider toxicology, anticonvulsant levels, blood cultures
- ABG
- BM
How much fluid can you give in hypotension in seizures?
Hypovolaemic patients require fluid resuscitation:
- Administer a 500ml bolus Hartmann’s solution or 0.9% sodium chloride (warmed if available) over 15 mins.
- Administer 250ml boluses in patients at increased risk of fluid overload (e.g. heart failure).
After each fluid bolus, reassess for clinical evidence of fluid overload (e.g. auscultation of the lungs, assessment of JVP). Repeat administration of fluid boluses up to four times (e.g. 2000ml or 1000ml in patients at increased risk of fluid overload), reassessing the patient each time.
How do you assess disability in seizures?
- Pupils (PEARL?)
- BM
- Review drug chart
- ?Drugs to terminate seizure
How do you assess Exposure in seizures?
- Rash
- Injuries suggestive on ICH e.g. Cushing’s reflex to suggest raised intracranial pressure
- Review notes
What is the treatment for seizures in an adult?

Define status epilepticus,
Seizure lasting >30min
OR repeated seizures without intrvening consciousness
Who is most affected by status epilepticus?
Usually those with known epilepsy
If no known epilepsy then likelihood of structural brain lesion is >50%
What are the signs and symptoms of non-convulsive status epilepticus?
- Absence seizure
- Continuous partial seizures with preservation of consciousness
- Look for subtle eye or lid movements
- EEG may be helpful
Ensure the patient is not pregnant as this could be eclampsia and immediate delivery may be needed.
Which medication may be used to prevent further seizures if they are due to vasculitis/cerebrak oedema?
10mg IV dexamethasone
What is a complication of lorazepam IV?
Respiratory arrest
How exactly should buccal midazolam be administered?
- 10yr old and over: 10mg
- 5-10yr: 7.5mg
- 1-5yr: 5mg
Squirt half volume between the lower gum and cheek on each side.
When is phenytoin contraindicated?
Bradycardia and heart block
Requires BP and ECG monitoring
What ITU help may be given if seizures continue >20min?
Paralysis and anaesthesia e.g. propofol
What signs are suggestive of pseudoseizures?
- Pelvic thrusts
- Resisting attempts to open lids
- Resisting attempts to do passive movements
- Arms and legs flailing around


