SANS Vascular Flashcards
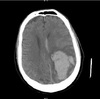
Seorang wanita 22 thn dengan sakit kepala dan pemeriksaan neurologis non-focal selama trimester akhir kehamilan pertama. CT-scan kepala ditampilkan. Intervensi segera paling tepat adalah :
A. Bolus manitol
B. Kortikosteroid
C. Penempatan ICP monitor
D. Evakuasi hematoma
E. Heparinisasi IV

E. Heparinisasi IV
The hemorrhage pattern visualized is the harbinger of a dural sinus thrombosis (DST). DST is an uncommon problem that can present benignly and rapidly deteriorate into a devastating and life threatening situation. Early recognition and intervention, even in stable patients, is is essential to improve outcome.
Venous stasis secondary to dural sinus thrombosis leads to a characteristic “flame Shaped” parenchymal hemorrhage with edema that resembles a contusion, usually in a lobar distribution, near a major venous sinus. Occasionally, asymmetric hemispheric edema can occur without hemorrhage, if there is adequate collateral venous drainage.
There are many risk factors for DST formation including pregnancy, peripartum/postpartum state, hormone replacement therapy, dehydration, malignancy, hypercoagulability, and inflammatory bowel disease.
In the stable patient, immediate anticoagulation with heparin is indicated. This includes patients with a neurological deficit who are not deteriorating. Gradual titration to to a therapeutic PTT (2 - 2.5 times normal) without a loading bolus has been shown to be effective with low risk.
Corticosteroids are not indicated because edema related to DST is cytotoxic rather than vasogenic. Furthermore, corticosteroids can promote hypercoagulability.
Craniotomy should be avoided at all costs in these patients. Venous stasis related to DST increases the risk of uncontrollable intraoperative hemorrhage. Hematoma enlargement following surgery is common.
Mannitol can be used as a temporizing measure when malignant intracranial hypertension is present. In this patient, however, the neurological exam is intact and the scan shows only surrounding edema without significant shift. There is no evidence that the rheological properties of low dose mannitol are beneficial in DST.
Intracranial pressure monitoring may be helpful in the management of patients with DST. In this patient however, the neurological exam can be used as a sensative indicator of deterioration. Some clinicians would consider inserting a monitoring device prior to initiating anticoagulation therapy. A fiberoptic subarachnoid monitor would be preferrable to a ventriculostomy to avoid transgressing the brain parenchyma.
Endovascular thrombolysis has been utilized successfully in some patients.

Seorang pria 36 tahun datang dengan riwayat 4 bulan kesulitan cara berjalan dan sakit kepala progresif lambat. MRI dan MRA otak menunjukkan aneurisma intrakranial sangat besar sebagian trombosis dari arteri vertebralis kiri menyebabkan kompresi batang otak dan hidrosefalus ringan. Angiografi serebral menunjukkan arteri vertebralis paten bilateral dan aneurisma V4 kiri fusiform giant. Manakah langkah manajemen selanjutnya yang paling tepat ?
A. Kraniotomi, bypass dan trapping aneurisma
B. Tes balon oklusi
C. VP shunt
D. Pemasangan stent dgn upfront coiling aneurisma
E. Pemasangan stent dgn staged coiling aneurisma
B. Tes balon oklusi
The most appropriate next step in management is balloon test occlusion. The patient’s primary problem is symptomatic mass effect upon the brainstem (with secondary early hydrocephalus), followed by future risk of aneurysm rupture. Successful treatment of the partially thrombosed aneurysm should lead to its thrombosis and gradual resorption, solving mass effect and hydrocephalus without necessarily invoking cerebrospinal fluid diversion via shunt placement. Both open surgical and endovascular methods are acceptable treatments for this giant aneurysm. However, both surgical bypass and endovascular treatment with parent vessel preservation are associated with significant morbidity and mortality. In selected patients who tolerate balloon test occlusion, parent vessel occlusion (either surgical or endovascular) may be a simpler and/or safer option; knowledge of whether the patient has adequate collateral supply is also very helpful during endovascular or surgical treatment. Therefore, balloon test occlusion should precede discussion and subsequent selection of treatment strategy for this aneurysm, irrespective of whether the latter is achieved via endovascular, surgical, or a combined approach.
Seorang pria berusia 44 tahun datang dengan onset akut sakit kepala dan potongan lapang pandang kiri. CT scan menunjukkan perdarahan akut di lobus oksipital kanan. Pencitraan MR dan angiografi disediakan. Apa manfaat yang paling mungkin dr embolisasi untuk lesi ini?
A. Penurunan resiko ruptur sebelum terapi lebih lanjut
B. Penurunan volume AVM untuk terapi selanjutnya
C. Obliterasi komplit AVM
D. Penurunan resiko kejang
E. Peningkatan penglihatan

B. Penurunan volume AVM untuk terapi selanjutnya
The benefit of embolization of large AVMs is to decrease the lesion size in conjunction with surgical or radiosurgical therapy. Incomplete embolization will not lower the risk of re-rupture and may even increase the rates of rupture in the interim. The likelihood of complete obliteration of large AVMs is low, except in small lesions with few vascular pedicles. There is no significant difference in the incidence of seizures. Visual outcomes are unlikely to be affected by embolization alone.

Seorang wanita 45 tahun menjalani kraniotomi sisi kanan untuk kliping dari pecahnya aneurisma arteri posterior communicating kanan. Pasca-bedah dia mengalami hemiplegia kiri, hemianesthesia kiri, dan defisit lapang pandang kiri homonim. CT kepala non-contrast menunjukkan area focal baru dari hypodensity ditunjukkan oleh panah. Oklusi dari arteri manakah yang dihasilkan infark ini dan sindrom klinis?
A. Recurrent artery of Heubner
B. Posterior Cerebral artery
C. Middle cerebral artery
D. Anterior choroidal artery
E. Posterior choroidal artery

D. Anterior choroidal artery
The correct answer is the anterior choroidal artery.
The anterior choroidal artery usually origates from the internal carotid artery. It provides blood to the choroid plexus within the lateral ventricles, the lateral geniculate body of the thalamus, and the posterior limb of the internal capsule. Occlusion of this artery can result in a clinical triad of contralateral hemiplegia, hemianesthesia, and a homonymous visual field deficit. In this case, the artery likely occluded as a result of vasospasm following subarachnoid hemorrhage. The other arteries do not supply brain regions that would produce this clinical syndrome

Seorang pria berusia 54 tahun datang dengan riwayat beberapa tahun tinnitus berdenyut progresif di telinga kanan dan sakit kepala baru. Dia mengalami angiografi serebral yang menunjukkan adanya shunting vena melalui fossa posterior selama injeksi selektif dari arteri pharyngeal ascending kanan (gambar: AP angiogram, proyeksi Townes). Berdasarkan temuan angiografi, jika tidak ditangani, Apakah kemungkinan besar yg akan terjadi dgn pecahnya malformasi ini ?
A. SDH
B. Perdarahan intraparenkim
C. Tidak bergejala
D. SAH
E. Dural sinus thrombosis

D. SAH
The angiogram demonstrates the presence of a posterior fossa dural arteriovenous fistula. The main arterial input is the right ascending pharyngeal artery and the primary venous drainage is via subarachnoid veins (pre-pontine and pre-medullary veins) with early opacification of the torcula and transverse sinuses. Because these veins are not typically able to withstand arterial pressure, patients with dural fistulae that drain into fragile intracranial such as prepontine/premedullary veins or cortical veins will usually present with rupture into the subarachnoid space. Fistulae that drain exclusively into the dural sinus without traversing subarachnoid veins can present with dural sinus thrombosis and subsequently parenchymal hemorrhage from venous infarction. Subdural hemorrhage as a result of dural fistula rupture is rare but has been reported.

Seorang pria 56 tahun dengan riwayat diabetes mellitus dan hipertensi datang dengan beberapa episode sakit kepala, pusing dan dysarthria dalam satu tahun terakhir. CT kepala normal. Anteroposterior angiogram arteri karotis interna kiri ditampilkan. Apa diagnosis yang paling mungkin?
A. Diseksi karotis
B. Dural arteriovenous fistula
C. Ruptur aneurisma serebral
D. Aterosklerosis intrakranial
E. Carotid-cavernous fistula

D. Aterosklerosis intrakranial
The angiogram depicts intracranial stenosis of the distal ICA, A1 branch of the anterior cerebral artery, and M1 branch of the middle cerebral artery which is most likely due to atherosclerosis given the patient’s history. Treatment options include antiplatelet therapy at a minimum, but can also include endovascular stenting (trials are currently ongoing) and arterial bypass (external carotid-internal carotid).
A dural arteriovenous fistula and carotid-cavernous fistula would demonstrate early filling of the venous system, which is not visualized in this angiogram. Likewise, there is no evidence of a saccular or fusiform dilatation of any of the vessels which would be suggestive of a ruptured cerebral aneurysm. The normal head CT also makes ruptured aneurysm less likely, although CT scans can be normal in up to 5% of patients with ruptured aneurysms. Finally, carotid dissection should demonstrate either irregularity of the carotid artery or an intimal flap indicative of a dissection, neither of which are depicted.

Seorang wanita berusia 58 tahun datang dengan keluhan sakit kepala dan bukti angiografik adanya infundibulum 2.5mm dari arteri communicating posterior. Manakah dari berikut ini mengenai infundibulum yg benar?
A. Memiliki resiko ruptur lebih tinggi dari aneurisma saccular pada ukuran yg sama
B. Tempat tersering terletak di arteri oftalmikus
C. Infundibulum seringnya berkembang menjadi aneurisma
D. Ditemukan lebih dari 25% dari angiogram yg dinyatakan normal
E. Biasanya berbentuk saccular
D. Ditemukan lebih dari 25% dari angiogram yg dinyatakan normal
Rates of infundibula have been reported from 7% to 25% depending on the series. The rate may be even higher (up to 40%) in those with a family history of infundibula. Infundibula may occur bilaterally in as many as 255 of non-familial cases. Aneurysm histology with loss of internal elastic lamina has been demonstrated in some infundibula.
Progression of infundibula to aneurysms has been reported. The most common site of infundibula is the junction of the posterior communicating and internal carotid artery. A large cooperative study demonstrated no rupture of infundibula less than 3mm however there have been a small number of case reports which have demonstrated infundibula themselves may rupture without the need for development of an aneurysm first. Infundibula are defined as being triangular/conical in shape with a vessel at the apex, and a widest portion of 3mm.
The patient can be reassured the chances of SAH or aneurysm formation from the infundibula descrebed here are extremely low.
Seorang pria berusia 67 tahun datang ke ruang emergensi dgn keluhan memburuknya parasthesia wajah ipsilateral dan ekstremitas kontralateral. Gejala tersebut diprovokasi oleh perputaran kepala. Dimana tempat paling mungkin terjadi kompresi vaskular pada pasien ini?
A. Arteri vertebral dominan
B. Arteri serebellar posterior inferior
C. Bifurkasio karotis
D. Arteri basilar
E. Arteri subclavian
A. Arteri vertebral dominan
The patient has Bow Hunter’s syndrome and the most likely site of compression is the dominant vertebral artery. Most cases occur at C1-2 with head rotation, but can occur at lower cervical levels. Constriction of the vertebral artery can be caused by mechanical narrowing, bone spurs, tumors, fibrous bands, infection, or trauma. Symptoms are due to vertebrobasilar insufficiency from intermittent vertebral artery occlusion with head rotation.
Most patients will not have a complete circle of Willis and will have an isolated posterior circulation. The dominant vertebral artery is usually the pathological side and a stenotic or hypoplastic contralateral vertebral artery is often seen. Symptoms will develop when the head is turned to the contralateral side as this compresses the artery maximally. Dynamic cerebral angiography with head turning will demonstrate flow limitation or occlusion when the head is turned to the contralateral side, however is associated with a slight increase in risk of TIA/stroke compared to a standard cerebral angiogram. Patients should be aware of this when consenting to the study. Angiogram will usually demonstrate an absent or hypoplastic posterior communicating arteries. CT/CTA and MR imaging may be helpful in demonstrating a bony spur or other cause of compression that may be amenable to surgical decompression. Cross section vascular imaging has the benefit of demonstrating relations of the vascular structures and the offending structure.
Management options include decompression of the offending structure in the case of the tumors and fibrous bands and bony spurs. Decompression of the bony foramen transversarium has also been used successfully. Soft tissue tethering or fibrous structures along the foramen transversarium or sulcus arteriosus are also viable options. Anticoagulation may be effective but is often not sufficient for complete symptom resolution. Hemilaminectomy at C1 to decompress the vertebral artery is another option to free up the artery. Cervical fusion at C1-2 immobilizes the segment and prevents dynamic compression at the cost of loss of neck rotation. As always; the best option for the patient is determined by the cause, the clincial status of the patient, and teh risks involved in the procedure.
Seorang pria berusia 75 tahun datang berkonsultasi kepada Anda dengan MRA leher (lihat Gambar 1). Berdasarkan MRA ini, tingkat stenosis karotis diestimasi terbaik sebagai :
A. >70%
B. >90%
C. >80%
D. >95%

A. >70%
Since the earliest days of diagnosing carotid stenosis with MRA, study after study has shown that while there is a high degree of correlation between MRA and both angiography and pathological specimens, even the best techniques are not perfect. The truest statement remains the following. When there is focal signal drop-out on the MRA this almost always implies a stenosis of greater than 70%, a fact that can be confirmed with duplex ultrasound. If greater precision is required CT angiography or rotational digital subtraction catheter angiography can be employed. This is especially useful when the MRA and doppler give discordant information.

Seorang pria berusia 75 tahun datang dengan kelemahan sisi kanan akut dan disfagia ekspresif ringan. Sebuah gambar MR representatif dan ipsilateral angiogram karotis disediakan. Menurut penelitian CREST, dibandingkan dengan endarterektomi karotis, angioplasty dan stenting memiliki insidensi lebih tinggi scr signifikan dari komplikasi peri-prosedural yg manakah ?
A. Disfagia
B. Stroke iskemik
C. Mortality
D. Cedera saraf hypoglossal
E. Infark myocardial

B. Stroke iskemik
In the Carotid Revasculatization Endarterectomy versus Stenting Trial (CREST) patients with symptomatic or asymptomatic carotid stenosis were randomly assigned to undergo carotid-artery stenting or carotid endarterectomy. Peri-procedural rates of individual components of the end points differed between the stenting group and the endarterectomy group: for death (0.7% vs. 0.3% p=0.18), for stroke (4.1% vs. 2.3% p=0.01) and for mycardial infarction (1.1% vs. 2.3% p=0.03%). The authors did find an interaction between age and efficacy with patients younger than 70 years having better outcomes with stenting and those older than 70 years having better outcomes with CEA. Cranial nerve dysfunction was higher in the carotid endarterectomy group.

Seorang pria berusia 75 tahun datang dengan progressive difficulty ambulating, kelemahan/ baal dan inkontinensia badder selama 12 bulan terakhir. MRI representatif dan angiogram spinal (injeksi interkostal T8 kiri) ditampilkan. Apa diagnosis yang paling mungkin?
A. Spinal cord glioma
B. Hemangioblastoma
C. Ruptur AVM spinal cord intrameduler
D. Herniasi diskus thoracic
E. Dural arteriovenous fistula

E. Dural arteriovenous fistula
The patient has a dural arteriovenous fistula (Type 1 spinal AVM) with the point of fistulization in or adjacent to the dura around the nerve root sleeve. These are more commonly present in men with an age of 40-70 years and usually occur in the thoracic or upper lumbar spine. No hemorrhage is evident on the patient’s MRI and these lesions have a low risk of hemorrhage. Symptoms are often progressive and due to venous hypertension as these lesions are usually a low-flow system. There is no spinal cord tumor or disk herniation with significant impingement on the spinal cord evident on the MRI.

Seorang pasien dengan riwayat hemiparesis kiri 2 jam yg lalu tetapi pasien tetap sadar dan alert. Pemeriksaan pasien menunjukkan tekanan darah 195/120 meskipun dgn pengobatan medis agresif. CT kepala menunjukkan ribbon sign dengan hilangnya diferensiasi kortikal gray-white tapi tidak ada efek massa atau perdarahan dan cutoff MCA proksimal. Seiring dengan pengobatan anti-hipertensi yang agresif, apa langkah selanjutnya yang paling tepat dalam pengobatan?
A. Pemberian tPA rekombinan IV dgn dosis 0,6 mg/kg
B. Pemberian tPA rekombinan IV dgn dosis 0,9 mg/kg
C. MRI otak
D. Kraniektomi dekompresi
E. Endovascular mechanical thombectomy
E. Endovascular mechanical thombectomy
Because of the persistently elevated blood pressure, this patient is not eligible for fibrinolytic therapy and the most appropriate management is endovascular mechanical thrombectomy. According to the 2007 guidelines for the early management of adult patients with acute ischemic stroke, patients with a blood pressure above 185/110 mmHg should be treated with intravenous labetalol or transdermal nitroglycerin paste or intravenous nicardipine. If this does not correct the blood pressure into the acceptable range, the patient should not be treated with fibrinolytics. The current guidelines do not recommend pursuing more aggressive blood pressure control measures in patients with blood pressures above 185/110 mmHg due to the low likelihood that consistent control can be maintained over the following 24 hour period. In the above scenario, since the patient’s blood pressure cannot be adequately controlled, endovascular thrombectomy should be performed since it is still within the therapeutic window (<8 hours for anterior circulation stroke).
When there are no contraindications to tPA therapy and patients present within a 3 hour window, tPA should be administered a dose of 0.9 mg/kg of tPA intravenously. Given that the infarct has no mass effect and the patient is otherwise alert and communicative, decompressive craniectomy is not indicated at this time. Brain MRI should be deferred until after chemical thrombolysis or mechanical thrombectomy.
Seorang pasien muda teridentifikasi memiliki fistula arteriovenosa dural posterior fossa yang diperdarahi hanya dengan cabang distal dari arteri faring ascending kanan (lihat Gambar 1: AP, proyeksi Townes) dan mengalir secara eksklusif melalui vena subarachnoid ke sinus dural. Manakah dari pilihan pengobatan berikut yg menimbulkan risiko terbesar dari defisit neurologis permanen kepada pasien?
A. Embolisasi coil trans-venous dr draining vein tepat di distal titik fistulisasi
B. Embolisasi trans-arterial melalui arteri pharyngeal ascending dgn onyx
C. Kraniotomi skull base lateral jauh dan ligasi klip dari draining vein
D. Stereotactic radiosurgery ke titik fistulisasi

B. Embolisasi trans-arterial melalui arteri pharyngeal ascending dgn onyx
All of these options represent reasoanble treatment plans for this dural fistula. The goal of the treatment is to occlude the draining vein just distal to the point of fistulaization. This can be accomplished with direct surgical placement of a clip on the draining vein, occlusion of the point of fistulization and proximal draining vein by trans-arterial onyx, trans-venous coil occlusion of the proximal draining vein just distal to the point of fistulization with detachable platinum coils, or radiosurgery. It is important to note that the ascending pharyngeal artery, while in this case, provides an easy trans-arterial route for the purpose of embolizing the fistula, also provides an important vascular supply via the neuromeningeal branch to the lower cranial nerves of the jugular foramen (IX, X, and XI). Using a liquid embolic agent in this area can occlude these perforating arteries and produce cranial nerve palsies that are unlikely to improve. Direct surgical visualization, trans-venous coil embolization, and radiosurgery represent safer alternatives to treatment of this particular fistula.

Menurut North American Symptomatic Carotid Endarterectomy Trial (NASCET), pada pasien dengan stenosis karotis simtomatik > 70%, dengan berapa kali carotid endarterectomy (CEA) dapat mengurangi tingkat cerebrovascular accident (CVA) dan kematian dari setiap penyebab saat 2 tahun dibandingkan dengan terapi medis terbaik?
A. 16,5%
B. 12,5%
C. 5,8%
D. 20,5%
E. 24,5%
A. 16,5%
The results of NASCET were published in 1991 and demonstrated that in symptomatic patients with > 70% stenosis (hemispheric or retinal transient ischemic attack or mild CVA within prior 120 days), CEA afforded an overall risk reduction of 16.5% at 2 years when compared to best medical management. In NASCET the perioperative risk of stroke or death from CEA was 5.8%.
Menurut meta-analisis dari tiga studi acak (HAMLET, DESTINY, dan DECIMAL), dibandingkan dengan manajemen medis terbaik, apakah efek hemicraniectomy dekompresi dalam waktu 48 jam dari onset stroke pada pasien <60 tahun dengan space occupying infark serebral terhadap mortalitas dan hasil yang buruk (modified Rankin Score [mRS]> 3) pada 1 tahun?
A. Penurunan tingkat kematian dan hasil buruk
B. Tidak ada perubahan pd tingkat kematian tetapi penurunan tingkat hasil buruk
C. Penurunan tingkat kematian tanpa perubahan pd tingkat hasil buruk
D. Penurunan tingkat kematian dengan peningkatan tingkat hasil buruk
E. Tidak ada perubahan pada keduanya (tingkat kematian dan hasil buruk)
A. Penurunan tingkat kematian dan hasil buruk
The correct answer is a decrease in both mortality and rate of poor outcome. The meta-analysis of patients in DECIMAL (DEcompressive Craniectomy In MALignant middle cerebral artery infarction), DESTINY (DEcompressive Surgery for the Treatment of malignant INfarction of the middle cerebral arterY), and HAMLET (Hemicraniectomy After Middle cerebral artery infarction with Life-threatening Edema Trial) who were randomised within 48 h of stroke onset revealed that surgical decompression reduced both poor outcome (absolute risk reduction of 23%) and case fatality (50% reduction).
While the results of HAMLET itself revealed a significantly decreased mortality rate in patients undergoing decompressive craniectomy compared to best medical management (22% vs 59%), the rate of poor outcomes between the two groups was not significantly different. The decrease in mortality mirrored what was previously reported by the DECIMAL and DESTINY trials but differed in that the DECIMAL and DESTINY trials demonstrated a trend towards improved outcomes that did not reach significance. The meta-analysis reported as part of the HAMLET study however was sufficiently powered to identify a significant reduction in both outcomes.
Seorang pria 80 tahun dengan riwayat demensia dan perdarahan intraserebral sebelumnya ditemukan tidak responsif dengan CT kepala yang ditunjukkan pada gambar. Apa ciri khas histopatologis dari kondisi yang paling mungkin?
A. Area dari protein tau terfosforilasi yg abnormal
B. Deposit beta amyloid di dalam tunika media pembuluh darah
C. Penebalan dinding oleh deposit lipid sub-intimal yg kaya akan hyaline
D. Deposit Ab-Ag komplek dan infiltrasi sel inflamasi
E. Deposit kolesterol dan plak fibrous

B. Deposit beta amyloid di dalam tunika media pembuluh darah
The histopathological hallmark of amyloid angiopathy is beta amyloid deposition within the tunica media of cerebral blood vessels. The CT scan demonstrates a lobar intracerebral hemorrhage (ICH), which in the context of an elderly patient with a history dementia and prior ICH is most likely due to amyloid angiopathy. This pathology is marked by beta-amyloid deposition within the media of leptomeningeal and cortical vessels, which demonstrates a characteristic yellow-green birefringence under polarized light microscopy when stained with Congo red dye. Fibrinoid necrosis may also be present.
Hypertensive ICH most commonly occurs in the basal ganglia (specifically, the putamen) (60%), thalamus (20%), pons (10%), and cerebellum (10%). Arteries and arterioles in hypertensive ICH demonstrate arteriolosclerosis with subintimal lipid-rich hyaline deposits. Antigen-antibody complexes and inflammatory cell infiltrates can be seen in several of the vasculidites. Types of vasculitis that can result in intracranial hemorrhage include polyarteritis nodosa, hypersensitivity vasculitis, Takayasu’s arteritis, Wegener’s granulomatosis, Behcet’s disease, and isolated angiitis of the CNS. Cholesterol deposits and fibrous plaques are the hallmarks of atherosclerotic disease, which is more likely to result in intracranial stenosis and thrombosis, not intracerebral hemorrhage. Areas of abnormally phosphorylated tau protein are seen in Alzhemer’s disease.
Berdasarkan studi ISUIA, hasil bedah dari aneurisma AComm unruptured ini tergantung pada :
A. Umur pasien
B. Daughter sacs
C. Konfigurasi aneurisma
D. Riwayat SAH sebelumnya
E. Riwayat merokok

A. Umur pasien
In the 2003 Lancet article, factors predicting surgical outcome of unruptured aneurysms include patient age >50, aneurysm location (anterior vrs. posterior circulation), aneurysm size, previous ischemic cerebrovascular disease and aneurysmal symptoms other than rupture.
According to the ISUIA, anterior circulation aneurysms with a maximal diameter between 7-12mm have a 2.6% risk of rupture within 5 years. In smaller aneurysms those with a prior SAH had a higher risk of rupture. Predictors of hemorrhage in multivariate analysis included size and posterior circulation location. Specifically, those with basilar tip aneurysms (OR=2.3, 95% CI 1.1-4.8, p=0.025) and posterior communicating aneurysms (OR=2.1, 95% CI 1.1-4.2, p=0.02) were more likely to rupture as compared with ICA aneurysms and cavernous aneurysms were less likely to rupture (OR=0.15, 95% CI 0.04-0.64, p=0.01).
In the cohort of treated patients with microsurgery and endovascular intervention, factors significantly associated with outcome included age, aneurysm size, and location. In anterior circulation aneurysms less than 12mm, microsurgery and endovascular treatment had similar rates of poor overall outcome at one year, but patients older than 50 years of age treated with endovascular therapy had better outcomes one year follow up. Aneurysm configuration, daughter sacs, smoking and history of prior subarachnoid hemorrhage were not predictors of surgical outcome.

The Carotid Revascularization Endarderectomy vs. Stenting Trial (CREST) baru-baru ini menyimpulkan bahwa risiko stroke dalam waktu 4 tahun setelah carotid endarderectomy tidak berbeda dengan risiko menjalani stenting arteri karotis. Apakah yang ditemukan dr penelitian CREST sehubungan dengan serangan jantung dan stroke dalam waktu 2 bulan pengobatan dan dampak dari peristiwa ini terhadap kualitas hidup?
A. Pasien dgn stenting arteri karotis mengalami stroke lebih jarang dalam 2 bln prosedur dibanding pasien dgn carotid endarderectomy dan penelitian menunjukkan stroke kurang begitu berdampak terhadap kualitas hidup dibanding serangan jantung
B. Pasien dgn carotid endarderectomy lebih sering terkena serangan jantung dalam 2 bln prosedur dibanding pasien dgn stenting arteri karotis dan penelitian menunjukkan serangan jantung kurang begitu berdampak terhadap kualitas hidup dibanding stroke
C. Pasien dgn stenting arteri karotis lebih sering terkena serangan jantung dalam 2 bln prosedur dibanding pasien dgn carotid endarderectomy dan penelitian menunjukkan serangan jantung berdampak banyak terhadap kualitas hidup dibanding stroke
D. Pasien dgn stenting arteri karotis lebih sering terkena stroke dalam 2 bln prosedur dibanding pasien dgn carotid endarderectomy dan penelitian menunjukkan stroke berdampak banyak terhadap kualitas hidup dibanding serangan jantung
E. Pasien dgn carotid endarderectomy lebih sering terkena serangan jantung dalam 2 bln prosedur dibanding pasien dgn stenting arteri karotis dan penelitian menunjukkan serangan jantung berdampak banyak terhadap kualitas hidup dibanding stroke
B. Pasien dgn carotid endarderectomy lebih sering terkena serangan jantung dalam 2 bln prosedur dibanding pasien dgn stenting arteri karotis dan penelitian menunjukkan serangan jantung kurang begitu berdampak terhadap kualitas hidup dibanding stroke
Patients undergoing carotid endarderectomy suffered more heart attacks within 2 months of the procedure compared to patients undergoing carotid artery stenting and the study showed that heart attack impacts quality of life less so than stroke. On the other hand, the risk of peri-procedural stroke was significantly higher in the stenting group. The study results demonstrated no difference in the estimated number of strokes within 4 years of either procedure. Interestingly, participants less than 70 years old appeared to benefit more from stenting than those over the age of 70. The CREST study enrolled patients with both asymptomatic and symptomatic carotid stenosis. The results of this trial show that carotid artery stenting (performed by well trained interventionalists) is a viable option versus traditional surgery, yet the decision to pursue stenting versus surgery must be done carefully.
Pendekatan bedah untuk lesi yang ditunjukkan (Gambar 1) yang membawa risiko terendah cedera neurologis adalah:
A. Pterional
B. Far lateral suboccipital
C. Orbitozygomatic
D. Midline suboccipital
E. Presigmoid

B. Far lateral suboccipital
This lateral vertebral angiogram demonstrates a small posterior inferior cerebellar artery aneurysm. This lesion can be approached using either a lateral suboccipital craniotomy/craniectomy or a far lateral suboccipital craniotomy/craniectomy, but the latter has been shown to be associated with a reduced incidence of lower cranial nerve palsies. The other approaches listed are inapproapriate. A midline suboccipital craniotomy would give one access to the distal PICA but not the proximal PICA where this aneurysm originates. The orbital zygomatic and pterional craniotomies are useful for aneurysms of the upper basilar artery and anterior circulation aneurysms. The presigmoid craniotomy is useful in gaining access to the mid-basilar artery and while one might see the dome of this aneurysm from a presigmoid approach one would not have proximal vertebral control.

Biasanya terdapat hubungan erat antara aneurisma ophthalmic dengan saraf optik (lihat Gambar). Defisit visual adalah risiko dengan operasi pada lesi ini. Strategi bedah untuk mencegah defisit visual meliputi:
A. Memotong pembuluh darah kecil hingga saraf untuk mendapatkan akses ke aneurisma leher
B. Pembukaan terlebih dahulu optic canal dan falciform ligament untuk membebaskan saraf optik
C. Retraksi saraf optik untuk mengoptimalkan penglihatan dari kubah aneurisma
D. Pembukaan terlebih dahulu sinus kavernosus untuk mendapatkan akses ke tempat tersering dari asal arteri oftalmikus dari ICA
E. Reseksi bagian dari gyrus rectus untuk mendapatkan visualisasi yg lebih baik

B. Pembukaan terlebih dahulu optic canal dan falciform ligament untuk membebaskan saraf optik
Early opening of the optic nerve and falciform ligament best prevents visual deficit. The optic nerve is often displaced superiorly by the aneurysm, and can be pressed against the falciform ligament, a dural fold that covers a segment of the optic nerve proximal to the optic foramen. This structure can act as a sharp tethering edge. Early opening of the optic canal and falciform ligament reduces the shear forces on the nerve during manipulation, and may reduce the chance of iatrogenic injury.
Visual deficits are potential complications of both the open and endovascular treatment of ophthalmic aneurysms. Visual loss can be caused by excessive heat from a drill, vascular compromise, retraction, mass effect of the aneurysm or other factors unknown to the surgeon.
Certain surgical principles may minimize the risk of visual deficit. The blood supply to the nerve should be meticulously preserved and every effort should be made to spare perforating arteries. Retraction of the nerve should be minimized. Resection of a portion of the gyrus rectus may be appropriate for exposure of an anterior communicating artery aneurysm, but this technique would not aid in exposure of the neck of an ophthalmic aneurysm or prevent a visual deficit. The most common site of origin of the ophthalmic artery is distal to the dural ring, outside of the cavernous sinus. Only approximately 8% of ophthalmic arteries originate within the cavernous sinus.

Apakah manajemen lini pertama yg plg tepat dari spinal dural fistula arteriovenous tipe 1 (lihat gambar) ?
A. Radiosurgery ke bagian proksimal dari fistula
B. Superselektif kateterisasi dan mengusahakan embolisasi
C. Observasi
D. Fractionated stereotactic radiotherapy
E. Surgical obliteration dari fistula

B. Superselektif kateterisasi dan mengusahakan embolisasi
The best initial therapy for this lesion is superselective catheterization of the fistula with attempt to embolize the lesion. Observation, radiosurgery or fractionated radiotherapy of these lesions is not indicated. Surgical obliteration is a viable alternative for a persistent fistula following embolization

Apakah saraf kranial yang paling sering pertama kali dipengaruhi oleh fistula arteriovenous di daerah sinus kavernosus?
A. CN IV
B. CN III
C. CN VI
D. CN V
E. CN II
C. CN VI
The sixth nerve is most commonly first affected by a cavernous sinus fistula, probably because it is typically free floating in the cavernous sinus and not within a dural fold as are the other nerves. Venous pressure is increased in the affected orbit, and the arterial pressure is decreased; this impairs perfusion of the eye and causes hypoxia. The hypoxic damage to the trabecular meshwork impairs aqueous outflow, raising intraocular pressure, which in turn increases resistance to perfusion even more, leading to further hypoxic damage. Damage to CN II therefore manifests later than that to the other intra-cavernous cranial nerves.


