S7) The Action Potential & Neuromuscular Junction Flashcards
What is an action potential?
An action potential is a change in voltage across the cell membrane
What are the properties of action potentials?
Action potentials:
- Depend on ionic gradients and relative permeability
- Only occur if a threshold level is reached
- Are propagated without loss of amplitude
- all or nothing

Describe the sodium hypothesis of the action potential
1 - Threshold potential reached
2 - Na+ channels open
3 - Na+ channels inactivate & K+ channels open
Explain the term threshold potential
- Threshold potential is the critical level to which a membrane potential must be depolarised to initiate an action potential
- Once this membrane potential is reached, a positive feedback occurs as Na+ channels begin to open
Depolarisation is followed by repolarisation.
What happens during this process?
- Potassium channels open causing an efflux of K+
- Sodium channels inactivate stopping the influx of Na+

What is the absolute refractory period?
The absolute refractory period is the time between the initial opening and subsequent closing of the Na+ channels (approx. ~1 millisecond in nerves)
- no stimulus can create an action potential no matter how strong
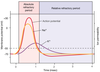
What is the relative refractory period?
The relative refractory period is the time needed for Na+ channels to recover back to their resting membrane potential so they can open again (approx. 4 milliseconds)
- strong stimulus can generate an action potential

Local anaesthetics act by binding to and block Na+ channels, thereby stopping action potential generation.
How is this achieved?
- Most local anaesthetics are weak bases and cross the membrane in their unionised form
- They block Na+ channels easily when the channel is open
- They also have a higher affinity for the inactivated state of the Na+ channel
In what order do local anaesthetics block the conduction in nerve fibres?
- Small myelinated axons
- Non-myelinated axons
- Large myelinated axons
What is electrical stimulation and how is it done?
- Electrical stimulation is used to stimulate an axon / group of axons to threshold potential, thus intiating an action potential
- Stimulation occurs under a cathode (negatively charged)
How does one calculate conduction velocity?
Conduction velocity = distance / time
How is an action potential conducted along an axon?
- A change in membrane potential in one part can spread to adjacent areas of the axon by local currents
- When local current spread causes depolarisation of part of the axon to threshold potential then an action potential is initiated in that location

What are the properties of the axon that lead to a high conduction velocity?
- A high membrane resistance
- A low membrane capacitance
- A large axon diameter
What is capacitance?
Capacitance is the ability of a lipid bilayer to store charge
Why does a low capacitance lead to a faster conduction velocity?
- A high capacitance takes more current to charge
- It can cause a decrease in local current spread
What is membrane resistance?
The membrane resistance is a function of the number of open ion channels
Why does a low membrane resistance lead to a slower conduction velocity?
The lower the resistance, the more ion channels are open and the more loss of local current occurs across the membrane
Local currents cause an action potential to propagate down an axon.
Why do action potentials not move backwards?
The action potential will not move backwards because the area of axon that has just fired an action potential is refractory and cannot fire another action potential until it has recovered from being refractory

Explain how the myelin sheath affects conduct velocity
Myelin reduces the capacitance and increases the resistance of the axonal membrane, hence increasing the overall conduction velocity







