S3) The Hip Flashcards
What is the hip joint?
The hip joint is a ball and socket synovial joint which connects the lower limb to the pelvic girdle
Describe the articulating surfaces of the hip joint
- Head of femur articulates with the acetabulum of the pelvis
- Acetabular labrum is a fibrocartilaginous collar which deepens the concavity

Describe the arterial supply of the hip joint
Arterial supply via the medial and lateral circumflex femoral arteries which are branches of the profunda femoris artery

What is the clinical significance of the medial circumflex artery?
- Medial circumflex femoral artery is responsible for the majority of the arterial supply (lateral artery has to penetrate through the thick iliofemoral ligament)
- Damage to the medial circumflex femoral artery can result in avascular necrosis of the femoral head
Describe the innervation of the hip joint
The hip joint is innervated by the femoral nerve, obturator nerve, superior gluteal nerve, and nerve to quadratus femoris
The only intracapsular ligament of the hip is the ligament of the head of the femur.
Describe its structure, function and anatomical location
- Structure: relatively small ligament
- Function: increases stability, encloses a branch of the obturator artery (artery to head of femur)
- Location: runs from the acetabular fossa to the fovea of the femur

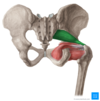
Identify the 3 extracapsular ligaments of the hip joint
- Iliofemoral ligament
- Pubofemoral ligament
- Ischiofemoral ligament
Describe the structure, function and location of the iliofemoral ligament
- Structure: ‘Y’ shaped appearance
- Function: prevents hyperextension of the hip joint
- Location: spans between the anterior inferior iliac spine and the intertrochanteric line of the femur

Describe the structure, function and location of the pubofemoral ligament
- Structure: triangular shape
- Function: prevents excessive abduction and extension
- Location: spans between the superior pubic rami and the intertrochanteric line of the femur

Describe the structure, function and anatomical location of the ischiofemoral ligament
- Structure: spiral orientation
- Function: prevents excessive extension
- Location: spans between the body of the ischium and the greater trochanter of the femur

Identify and describe the factors that stabilise the hip joint
- Acetabulum – encompasses nearly all of the femoral head (decreases chance of dislocation)
- Acetabular labrum – increases depth provides a larger articular surface
- Intracapsular & extracapsular ligaments
- Joint capsule
Explain how the muscles and ligaments work in a reciprocal fashion at the hip joint
- Anteriorly, where the ligaments are strongest, the medial flexors are fewer and weaker
- Posteriorly, where the ligaments are weakest, the medial rotators are greater in number and stronger
Identify the possible movements at the hip joint as well as the muscles involved
- Flexion: iliopsoas, rectus femoris, sartorius
- Extension: gluteus maximus, semimembranosus, semitendinosus, biceps femoris
- Abduction: gluteus medius, gluteus minimus and deep gluteals
- Adduction: adductors longus, brevis & magnus, pectineus, gracillis
- Lateral rotation: biceps femoris, gluteus maximus, deep gluteals
- Medial rotation: gluteus medius & minimus, semitendinosus, semimembranosus
Identify and describe the three articulations of the hip bone
- Sacroiliac joint – articulation with sacrum
- Pubic symphysis – articulation with the corresponding hip bone
- Hip joint – articulation with the head of femur

Which three parts compose the hip bone?

How do the bones composing the hip joint vary before and after puberty?
- Prior to puberty, the triradiate cartilage separates these constituents
- After age 15-17 the three parts begin to fuse (forms acetabulum)

The superior part of the hip bone is formed by the ilium, the widest and largest of the three parts.
Describe its structure

- Body: forms the superior part of the acetabulum
- Wing: expansion above the acetabulum
- Iliac fossa: concave inner surface
- Gluteal surface: convex external surface
- Iliac crest: thickened superior margin (extends from ASIS to PSIS)

Which muscles attach to the ilium?
- Gluteal muscles attach to the gluteal surface of the Ilium (at anterior, posterior and inferior gluteal lines)
- Iliacus muscle attaches medially at the iliac fossa
Why is the anterior superior iliac spine clinically relevant?
The ASIS serves as the attachment site of the inguinal ligament, which runs from the ASIS to the pubic tubercle

The most anterior portion of the hip bone is formed by the pubis
Describe its structure

- Body – located medially & articulates with opposite pubic body at the pubic symphysis
- Superior ramus – extends laterally from the body, forming part of the acetabulum (encloses the obturator foramen)
- Inferior ramus – projects towards and joins the ischium (encloses the obturator foramen)

The posterioinferior part of the hip bone is formed by the ischium.
Describe its structure

- Inferior ischial ramus – combines with inferior pubic ramus to form the ischiopubic ramus (encloses part of obturator foramen)
- Ischial tuberosities – found on posterorinferior aspect of the ischium (carries body weight when sitting)
- Greater sciatic notch – found on the posterior aspect of the ischium

Which ligaments attach to the ischium and what do they do?
- Sacrospinous ligament which runs from the ischial spine to the sacrum, forming the greater sciatic foramen
- Sacrotuberous ligament which runs from the sacrum to the ischial tuberosity, forming the lesser sciatic foramen

What is fascia?
Fascia is defined as a sheet or band of fibrous tissue lying deep to the skin that lines, invests and separates structures within the body

The fascia lata is a deep fascial investment of the whole thigh musculature.
Describe its structure and location
- Structure: strong, extensible and elasticated
- Location: begins around the iliac crest and inguinal ligament, ends at the bony prominences of the tibia (becomes crural fascia)