Review questions (1-8, 12-15) Flashcards
Which large leukocyte with one kidney-shaped nucleus and some granulesis is located in the bloodsteam?
Monocytes

The immune biochemical mediators secreted by the immune cells are responsible for which of the following tissue destruction seen in periodontitis?
A. Destruction of gingival connective tissue
B. Resorption of alveolar bone
C. Breakdown of periodontal ligament
D. All of the above
D. All of the above

Which large leukocyte with one kidney-shaped nucleus and is located in tissues?
Macrophages

Redness, swelling, bleeding, and tenderness of the gingiva in response to dental plaque only are clinical signs of which of the following?
A. Periodontitis
B. Non–plaque-induced gingival diseases
C. Plaque-induced gingival diseases
D. Gingivostomatitis
C. Plaque-induced gingival diseases
Gingivitis as a result of an exaggerated inflammatory response to plaque and hormone changes in a pregnant woman that includes a localized mushroom-shaped mass projecting from a gingival papilla is termed:
A. Non–plaque-induced gingival disease
B. Puberty-associated gingivitis
C. Leukemia-associated gingivitis
D. Pregnancy-associated pyogenic granuloma
D. Pregnancy-associated pyogenic granuloma
The gingival mass is characterized by a mushroom-like tissue mass that most commonly occurs in the maxilla and interproximally

In which of the following phases of periodontal disease progression does the plaque biofilm extend subgingivally into the gingival sulcus?
A. Plaque accumulation phase (Initial lesion)
B. Established gingivitis phase (Established lesion)
C. Inflammatory mediator phase
D. Periodontitis phase (Advanced lesion)
B. Established gingivitis phase (established lesion)
Initial lesion = Bacteria colonize the tooth surface near the gingival margin
Early lesion = Bacterial accumulation continues and biofilm maturation occurs.
Established lesion = Plaque biofilm extends subgingivally into the gingival
sulcus, disrupting the attachment of the coronal-most portion of the JE from the tooth surface
Advanced lesion = This phase is characterized by periodontal pocket formation, bleeding on probing, alveolar bone loss, furcation involvement, and tooth mobility.
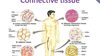
Connective tissue is comprised of a gel-like substance, fibers, and few cells
A. True
B. False
True
The gingival connective tissue is comprised of a gel-like substance,
protein fibers, and cells.

In the junctional epithelium, epithelial cell attaches to neighboring epithelial cells via:
A. Desmosomes
B. Hemidesmosomes
C. External basal lamina
D. Internal basal lamina
A. Desmosomes
Desmosome—a specialized cell junction that connects two
neighboring epithelial cells and their cytoskeletons together.

What are S. mitis, S. sanguis, and Actinomyces viscosus associated with?
Tooth-associated plaque biofilm
bacteria that are attached to the tooth surface.
A cell junction that connects an epithelial basal cell to the basal lamina is termed:
A. Hemidesmosome
B. Desmosome
C. Epithelial ridge
D. Connective tissue papilla
A. Hemidesmosome
Hemidesmosome—a specialized cell junction that connects the
epithelial cells to the basal lamina. You might think of
hemidesmosomes as specialized structures that represent half of a desmosome.
1. A cell-to-basal lamina connection
2. An important form of cell junction found in the gingival epithelium

. What type of bone resorption occurs in an uneven oblique direction affecting only one tooth?
A. Osseous crater
B. Horizontal bone loss
C. Vertical bone loss
D. Infrabony defect
D. Infrabony defect
Infrabony defects result when bone resorption occurs in an uneven,
oblique direction. In infrabony defects, the bone resorption
primarily affects one tooth.
- Infrabony defects are classified on the basis of the number of osseous
walls. Infrabony defects may haveone, two, or three walls

The deep extensions of epithelium that reach down into the connective tissue are termed:
A. Hemidesmosomes
B. Desmosomes
C. Epithelial ridges
D. Connective tissue papillae
C. Epithelial ridges
Epithelial ridges—deep extensions of epithelium that reach down
into the connective tissue. The epithelial ridges are also known as rete pegs.
With the Cairo classification system, which type is associated with recession from traumatic toothbrushing?
A. RT1
B. RT2
C. RT3
A. RT1
Recession Type 1 (RT1)**: Gingival recession with **no loss of interproximal attachment.** Interproximal **CEJ** is **clinically not detectable at both mesial and distal** aspects of the tooth. **RT1 recession** defects represent defects that are most likely associated with **traumatic toothbrushing** in **healthy periodontal tissues.

Identify the hypothesis:
Accumulation of plaque biofilm leads to gingival inflammation
Non-Specific Plaque Hypothesis
Which of the following forms the base of a gingival sulcus?
A. Interdental gingiva
B. Attached gingival
C. Junctional epithelium
D. Periodontal Ligament
C. Junctional epithelium

Which of the following are the three major forms of periodontitis?
A. Necrotizing periodontitis, periodontitis, periodontitis as a manifestation of systemic disease
B. Stage I, Stage II, Stage III
C. Grade A, Grade B, Grade C
A. Necrotizing periodontitis, periodontitis, periodontitis as a manifestation of systemic disease

All of the following are classic symptoms of acute inflammation, EXCEPT:
A. Loss of function
B. Bruising
C. Swelling
D. Heat
B. Bruising

Class II Miller Classification for Gingival Recession indicates:
A. Recession does not extend into MGJ
B. Recession is so severe that root surfaces are not covered
C. Recession extends to the MGJ but all of the root is covered
C. Recession extends to the MGJ but all of the root is covered
- Class II: Marginal tissue recession, which extends to or beyond the
- *MGJ**. There is no periodontal loss (bone or soft tissue) in the
- interdental area**, and 100% root coverage can be anticipated.

Identify the hypothesis:
This theory postulates that it is a shift in the local environment that drives the changes in microbial composition that lead to periodontal disease.
Ecological Plaque Hypothesis
Which of the following is a normal process that protects and heals the body?
A. Acute inflammation
B. Chronic inflammation
A. Acute inflammation

Which of the following tissues fills the spaces between the tissues and organs of the body?
A. Basal lamina
B. Connective tissue
C. Epithelial tissue
D. Keratinized tissue
B. Connective tissue
Gingivitis in an adolescent as a result of an exaggerated inflammatory response to a relatively small amount of plaque and increased levels of sex hormones is termed:
A. Non–plaque-induced gingival disease
B. Puberty-associated gingivitis
C. Diabetes-associated gingivitis
D. Cyclosporine-induced gingivitis
B. Puberty-associated gingivitis
puberty-associated gingivitis is characterized by an exaggerated inflammatory response of the gingiva to a relatively small amount of plaque biofilm around the
time of puberty. The exaggerated response is modulated by hormones released during puberty.

A bacterial infection of the periodontium characterized by a slow destruction of the periodontal ligament, slow loss of supporting bone, and a good response to periodontal therapy is termed:
A. Periodontitis
B. Refractory periodontitis
C. Necrotizing periodontal disease
D. Recurrent periodontal disease
A. Periodontitis
Periodontitis is a complex microbial infection that triggers a host mediated
inflammatory response within the periodontium, resulting in progressive destruction of the periodontal ligament and supporting alveolar bone.

Current perspective on the etiology of periodontal disease states plaque biofilm is necessary for initial inflammation, and plaque biofilm alone is not sufficient for periodontal destruction.
A. The first phrase is true, second phrase is false
B. The first phrase is false, second phrase is true
C. Both phrases are true
D. Both phrases are false
C. Both phrases are true
Nonspecific Plaque Hypothesis**
This theory proposed that the **accumulation of plaque
biofilm**—an abundance of bacteria in the biofilm—adjacent to the
gingival margin led to **gingival inflammation** and the **subsequent tissue
destruction seen in periodontitis.
In what ways do antibodies participate in the host defense?
Neutralize bacteria or bacterial toxins to prevent bacteria from destroying host cells
Coat bacteria making them more susceptible to phagocytosis
Activate the compliment system
Identify the hypothesis:
The presence of certain microbial pathogens—even in low numbers—can cause a shift from beneficial to pathogenic microbes in the biofilm community. The key concept of this theory is that even at low levels, keystone pathogens can have a significant impact on the oral biofilm that initiates an uncontrolled host immune response.
Keystone Pathogen Hypothesis
Ascorbic acid–deficiency gingivitis is a severely low level of:
A. Vitamin B
B. Vitamin K
C. Vitamin A
D. Vitamin C
D. Vitamin C

A single microscopic organism is termed:
A. Bacteria
B. Bacterium
C. Nucleoli
D. Aerobic
B. Bacterium
Bacterium (plural, bacteria). Bacteria are the simplest organisms
and can be seen only through a microscope.
Which pattern of bone loss results in a fairly even, overall reduction in the height of the alveolar bone?
A. Horizontal bone loss
B. Vertical bone loss
C. Both A and B
A. Horizontal bone loss

An important function of the cementum of the tooth is to attach the periodontal ligament fibers to the tooth.
A. True
B. False
True
The attachment of the fiber bundles occurs when the cementum and
bone are forming. As cementum forms, the tissue calcifies around the
ends of the periodontal fibers (Sharpey fibers) surrounding them with
cementum.

Examples of medications that cause gingival enlargement include all EXCEPT:
A. Calcium channel blockers
B. Anticonvulsants
C. Nonsteroidal anti-inflammatories
D. Immunosuppressants
C. Nonsteroidal anti-inflammatories
Drug-influenced gingival enlargements are an increase in size of the
gingiva associated with certain systemic medications, most commonly
anticonvulsants, calcium channel blockers, and immunosuppressants.
The pattern of tissue enlargement is irregular, usually first observed in the papillae, beginning as a painless area of enlargement on the papilla and then proceeding to the marginal gingiva.

Which of the following tissues serves as a covering tissue for the outer surfaces of the body and a lining tissue for body cavities such as the mouth, stomach, and intestines?
A. Basal lamina
B. Connective tissue
C. Epithelial tissue
D. Keratinized tissue
C. Epithelial tissue
The epithelial tissue is the tissue that makes up the outer
surface of the body (skin or epidermis) and lines the body cavities such
as the mouth, stomach, and intestines (mucosa). The skin and mucosa of
the oral cavity are made up of stratified squamous epithelium—a type
of epithelium that is comprised of flat cells arranged in several layers.
Which of these immune cells secrete antibodies?
A. Macrophages
B. Polymorphonuclear leukocytes
C. B-lymphocytes
D. T-lymphocytes
C. B-lymphocytes
B-lymphocytes: small leukocytes that help in the defense against bacteria, viruses, and fungi; principal function is to make antibodies. B-lymphocytes can further differentiate into one of the two types of cells: plasma B-cells and memory B-cells.

. If gingival tissues are healthy they will ALWAYS have a stippled appearance.
A. True
B. False
False
Healthy gingival tissue showing a stippled appearance.
Stippling varies greatly from individual to individual. In some patients,
healthy tissue may not exhibit a stippled appearance.

Gingivitis from poor self-care that has existed for years without progressing to periodontitis is termed:
A. Localized gingivitis
B. Generalized gingivitis
C. Necrotizing Gingivitis
D. Plaque-induced gingivitis
D. Plaque-induced gingivitis
The primary purpose of the immune system is to:
A. Defend the life of the host (the individual)
B. Identify bacterial invaders
C. Cause swelling and redness at the infection site
D. Phagocytize bacteria
A. Defend the life of the host (the individual)
The prime purpose of the human immune system is to defend the life of the individual (host) by identifying foreign substances in the body (bacteria, viruses, fungi, or parasites) and developing a defense against them
Non–plaque-induced gingival lesions:
A. Heal after meticulous plaque control
B. Are not affected by the presence of plaque
C. May have various causes
D. Always require periodontal therapy
C. May have various causes
non–plaque-induced gingival diseases—are not caused by plaque biofilm and do not resolve after plaque biofilm removal.
Why is frequent periodontal instrumentation important in the control of dental plaque biofilms located in periodontal pockets?
A. A toothbrush and floss cannot clean root surfaces within a periodontal pocket
B. Few patients take the time for self-care at home
A. A toothbrush and floss cannot clean
root surfaces within a periodontal pocket
Which phase of periodontal disease progression is characterized by tissue destruction?
A. Plaque accumulation phase
B. Established gingivitis phase
C. Inflammatory mediator phase
D. Periodontitis phase
D. Periodontitis phase
Periodontitis phase = Advanced lesion
This phase is characterized by periodontal pocket formation, bleeding on probing, alveolar bone loss, furcation involvement, and tooth mobility.
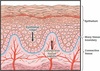
In MOST places in the body, the epithelium meets the connective tissue in a wavy, uneven junction.
A. True
B. False
True
- In most cases, the epithelium meets the connective tissue at*
- an uneven, wavy border.*
- Epithelial ridges extend down into the connective tissue.
- Connective tissue** papillae extend upward into the epithelium.

Identify the hypothesis:
Specific groups of bacteria (T. forsythia, P.gingivalis, and Treponema denticola) cause various periodontial diseases.
Orange, red = Perio
Yellow, green blue and purple = health
Socransky’s Microbial Complexes

Cytokines that play an important role in periodontitis are:
A. PGE
B. IL-1, IL-6, IL-8, and TNF-a
C. PPT
D. MMP
B.
IL-1, IL-6, IL-8, and TNF-a

A well-organized community of bacteria that adheres to surfaces and is embedded in an extracellular slime layer is termed:
A. Aerobic
B. Anaerobic
C. Biofilm
D. Bacterial microcolony
C. Biofilm
A biofilm is a complex and dynamic microbial community— containing a diverse array of many types of microbial species (bacteria, fungi, and viruses)—embedded within a self-protective matrix that adheres to a living or nonliving surface.
The junctional epithelium attaches to the connective tissue via the:
A. Desmosomes and the internal basal lamina
B. Desmosomes and the external basal lamina
C. Hemidesmosomes and the internal basal lamina
D. Hemidesmosomes and the external basal lamina
D. Hemidesmosomes and the external basal lamina
The epithelial cells of the JE attach to the underlying gingival
connective tissueviahemidesmosomesand theexternal basal lamina












































