Restrictive Airways Disease Flashcards
(57 cards)
What is happening in restrictive lung disease?
People find it hard to fully expand their lungs with air on inhalation
What area is affected by restrictive disease?
Lungs
What is restrictive lung disease?
A category of extrapulmonary, pleural, or parenchymal respiratory diseases that restrict lung expansion, resulting in a decreased lung volume, an increased work of breathing, and inadequate ventilation and/or oxygenation.
What are causes of thoracic restriction out-with the lungs?
-Vertebrae, e.g. kyposcoliosis - Ribs e.g. traumatic multiple ribs - Muscle weakness e.g. intercostal or diaphragmatic - Abdominal obesity or ascites
What occurs with lung restriction?
Chronic alveolar under-ventilation with low PaO2 and raised PaCo2 and reduced lung volumes
What is Diffuse Parenchymal Lung Disease (DPLD)?
Disease of alveolar structures, specifically affecting the interstitium (the tissue and space around the air sacs of the lungs). Also known as interstitial lung disease - umbrella term.
What is the spectrum for Diffuse Parenchymal Lung Disease according to BTS classification?
1.Acute DPLD 2.Episodic DPLD, all of which may present acutely 3.Chronic DPLD due to occupational or environmental agents or drugs. 4.Chronic DPLD with evidence of systemic disease 5.Chronic DPLD with no evidence of systemic disease
What is the aetiology of DPLD?
1) Fluid in alveolar air spaces 2) Consolidation of alveolar air spaces e.g. infection or infarct 3) Inflammatory infiltrate of alveolar walls e.g. EAA, sarcoidosis etc 4) Dust disease (pneumoconiosis) e.g. fibrogenic and non-fibrogenic 5) Carcinomatosis
What are various causes of alveolitisi (i.e. inflammatory infiltrate of alveolar walls)?
- Granulomatous alveoli’s - Extrinsic allergic alveoli’s e.g. farmers lung and avian - Sarcoidosis - Drug induced alveoli’s e.g. amiodarone or bleomycin - Fibrosisng alveolitis e.g. rheumatoid or cryptogenic (IPF) - Toxic gas/fumes e.g. chlorine - Autoimmune e.g. churg strauss
What are the various dust-diseases related to DPLD?
- Fibrogenic: asbestosis and silicosis - Non -fibrogenic: sideriosis (iron), stenosis (tin) and baritones (barium)
What is the clinical syndrome of DPLD?
-Breathless on exertion -Cough but no wheeze -Finger clubbing -Inspiratory Lung crackles -Central cyanosis (if hypoxaemic) -Pulmonary fibrosis occurs as end stage response to chronic inflammation
What are the diagnostic factors in spirometry for DLPD?
-Reduced lung volumes •↓FEV1 ↓FVC normal ratio > 75% •Peak flow normal
Which serum factors are raised in sarcoidosis?
ACE and Ca2+
What antibodies may be seen in DPLD?
Avian, Fungal, Auto-antibodies (Rheumatoid, Anti-nuclear)
What tests would you do to diagnose DPLD?
-Reduced lung volumes on spirometry -Reduced gas diffusion -Arterial oxygen desaturation -Antibodies: Avian, Fungal, Auto-antibodies -Serum ACE and Ca2+ raised in Sarcoidosis -Bilateral diffuse alveolar infiltrates on chest X-ray -High resolution CT scan-Inflammatory ground glass vs Fibrotic nodular component of alveolar infiltrates -Bronchoalveolar lavage or induced sputum-to exclude Pneumocystis, TB or other infection
What is the management for DLPD?
- Remove any trigger - Treat inflammation with corticosteroids e.g. oral prednisoline (not inhaled) -O2 if hyperaemic - Lung transplant as last resort
Pulmonary interstitium
Basically the gas exchange areas of the lungs
Alveolar Type I cells
Form the blood air barrier (squamous epithelium)
Alveolar Type II cells
Produce surfactant (cuboidal)
What is the early stage of interstitial lung disease?
Alveolitis
What is the late stage of interstitial lung disease?
Fibrosis
How do you diagnose interstitial lung disease?
Transbronchial biopsy – special forceps used at bronchoscopy Thoracoscopic biopsy – more invasive but more reliable and generates far more tissue
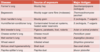
What are the main forms of chronic interstitial disease?
- Fibrosing alveolitis (aka idiopathic pulmonary fibrosis)
- Sarcoidosis
- Extrinsic allergic alveolitis (hypersensitivity pneumonitis)
- Pneumoconiosis (caused by inhalation of mineral dust)
- Connective tissue diseases
What is fibrosing alveolitis also known as?
Idiopathic pulmonary fibrosis