Respiratory Flashcards
What is the alveolar gas equation?
PAO2 = FiO2(PB – PH2O) – PCO2 / RQ PAO2 = alveolar oxygen partial pressure FiO2 = fraction of inspired oxygen PB = barometric pressure (760) PH2O = vapor pressure of water (47) RQ = respiratory quotient (0.8)
What are the key anesthetic points to peripheral neuropathies such as a acute inflammatory demyelinating polyradiculopathy (AIDP) also known as Guillain-barre sydrome?
absolute contraindication to succinylcholine due to risk of hyperK.
avoidance of prolonged paralysis at all costs to help prevent the risk of prolonged muscle weakness
whats the deal with hyperoxia?
microvascular perfusion have demonstrated a peripheral vasoconstrictive response to hyperoxia.
so in total hyperoxia will tend to cause systemic vasoconstriction and pulmonary vasodilation. Excess dissolved oxygen in the plasma may cause an increase in circulating reactive oxygen species which may increase the oxidative stress on teh body’s system.
when would both peak inspiratory and plateau pressures be elevated?
lung resistance can be divided into airway resistance and elastic resistance.
airway resistance affects airflow into the lungs. Peak inspiratory pressure directly varies with flow resitance. if resistance to flow increases, Pip increases. Pip measures resistance from the ventilator tubing to the segmental bronchi.
elastic resistance affects teh expansion of the lungs. this can also be thought of as pulmonary compliance. when elastic resistance increases, pulm compliance decreases. Changes in elastic resistance causes changes in both peak pip and plateau pressure.
situations that increase airway resistance (or decrease airflow) will result in increased PIP. includes: bronchospasm, airway compression, kinked ett, airway secretions, mucus plugs. P plateau remains unchanged.
situations that increse the elastic resistance (or decreased compliance) will result in increased pip and Pplateau. these include intrinsic pulmonary diseases, ascites, obesity, abdominal insufflation, tension pneumothorax, and trendelenburg position.
what is the most common acid in teh body? what are the bodys buffering systems?
Bottom Line: Carbon dioxide is the most common acid in the body, and its regulation and elimination have the most impact on whole-body acid-base regulation. There are three primary mechanisms by which acid-base balance is maintained. The first and most direct are buffer compounds such as bicarbonate, phosphate, and plasma proteins. These compounds bind the hydrogen ions that are produced by the ionization of carbonic acid and prevent a pH change in the serum. Second, the ventilatory response to either increased or decreased serum pH will result in an increased or decreased serum CO2 level respectively. Third, over the span of hours to days the kidneys will begin to excrete hydrogen ions in the setting of systemic acidosis.
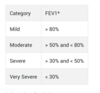
what is severe vs moderate vs mild copd?
All patients with COPD have some degree of airways obstructive disease by definition and this is manifested by an FEV1/FVC ratio of < 70% predicted on spirometry.
The severity of the COPD can further be stratified based upon the FEV1 according to the table below.
what are ecg changes assoc. with phtn?
Electrocardiographic findings of right axis deviation, right bundle branch block, and peaked P waves all suggest right heart changes consistent with pulmonary hypertension.
what is dlco? what dlco is associated with poor outcomes? in what surgery?
what can be used instead of dlco?
DLCO, a measurement of gas exchange, correlates with the total functioning surface area of the alveolar-capillary interface. A predicted postoperative DLCO of less than 40% is associated with increased postoperative respiratory complications after lung resection surgery. Alternatively, adequacy of gas exchange can be assessed by an arterial blood gas showing PaO2 greater than 60 mm Hg and a PaCO2 of less than 45 mm Hg.
what is this showing?

The inspiratory portion of a pressure-volume loop classically shows two inflection points. The first, or lower inflection point, represents the pressure needed to effectively recruit collapsed alveoli. The second, or upper inflection point, marks the transition from normal compliance to over-distention. A sharp rightward deflection of the pressure-volume loop, as in this case, represents progressively increasing pressure without a significant increase in delivered volume. This “bird’s beak” appearance should prompt the anesthesiologist to reduce driving pressures or delivered tidal volume to prevent volutrauma.
what does respirtory or metabolic alkalosis do to ca, k and phos levels?
Respiratory and metabolic alkalosis leads to a decrease in extracellular hydrogen ion concentration. This, in turn, leads to extracellular shifting of hydrogen ions and reciprocal intracellular shifting of reciprocal cations such as calcium, phosphate, and potassium. Respiratory alkalosis leads to hypocalcemia, hypokalemia, and hypophosphatemia.
An otherwise healthy patient presents to the Emergency Department after a severe house fire. The hemoglobin is 14 mg/dL and the oxygen saturation measures 98% on room air. An arterial blood gas is drawn and is noted for acidosis with a pH of 7.05 and a PaO2 of 97 mmHg. What is the driving force behind the acid-base disturbance in this patient?
Carbon monoxide poisoning leads to the formation of CO-Hgb and causes a decrease in oxygen delivery to tissues. This eventually will lead to the development of lactic acidosis and the corresponding metabolic disturbances.
This is do to carbon monoxide poisoning
what is. the o2 content equation?
CaO2 = [(SaO2 * Hgb * O2 carrying capacity of Hgb) + (O2 solubility * PaO2)]
how does carbon monoxide poisoning work?
what is methemoglominemia? causes?
Methemoglobinemia is due to the oxidation of iron from the Fe2+ (ferrous) to the Fe3+ (ferric) form, which leads to the inability of heme to bind oxygen. This results in diminished oxygen content and less oxygen delivery. This combination could lead to lactic acidosis. Exposure to carbon monoxide from a fire would lead to CO-Hgb being formed and not the oxidation of the heme group.
Important causes of methemoglobinemia include benzocaine, dapsone, and inhaled nitric oxide.
Tx: methyelene blue
how does one manage a bronchopleural fistula?
End expiratory pressure, a short inspiratory time, low tidal volumes, and low respiratory rate are the tenants of management to help decrease the risk of leakage across the bronchopleural fistula (BPF). Lung isolation techniques can help decrease the pressures and volumes needed. Spontaneous ventilation is preferred over positive pressure ventilation.
what are the apnea/hypopnea index for osa?
The total number of episodes of apnea or hypopnea (reduction of airflow >50%) divided by the total sleep time creates an apnea/hypopnea index (AHI). An AHI of 5-15 events per hour indicates mild disease, 15-30 events indicates moderate disease, and severe disease is indicated by an AHI of >30 events per hour.
in obesity what happens to:
pulmoonary compliance
ERV
FRC
closing capacity
Obesity leads to a reduction in pulmonary compliance, ERV, and FRC. Closing capacity is largely unchanged. When FRC falls below closing capacity, it leads to undesirable effects such as atelectasis, shunt, and hypoxemia.
what is postpneumonectomy pulmonary edema? causes?
Acute lung injury (ALI) associated with pneumonectomy, also known as “post pneumonectomy pulmonary edema”, has an incidence of only 4% but a mortality rate of 30-50%. It is defined as acute hypoxemic respiratory failure of a non-cardiogenic nature. Patients present with acute onset tachycardia, tachypnea, fever, and hypoxemia. Although mainly a diagnosis of exclusion, it requires a PaO2/FiO2 < 200, pulmonary capillary wedge pressure < 18 mm Hg, and bilateral infiltrates on chest radiograph. The exact etiology is unclear and thought to be multi-factorial. The pathophysiology is thought to revolve around loss of endothelial integrity leading to capillary leak and subsequent extravasation of proteins and inflammatory cells into the interstitium.
Studies have shown risk factors associated with post pneumonectomy pulmonary edema (PPE) to be:
- Pre-op alcohol use
- Right sided pneumonectomy
- Perioperative fluid overload
- High intraoperative airway pressures
- High urine output in the post-operative period
what patients are at high risk for complications post thoracic surgery?
hese highest-risk patients are those with a predicted postoperative FEV1 or DLCO of less than 30%, or a VO2max of less than 15 mL/kg/min before the surgery

C
at what PaO2 is the hypoxic respiratory drive kicked in?
Peripheral chemoreceptors, primarily the carotid bodies but also the aortic bodies, are responsible for the hypoxic ventilatory response. In an otherwise healthy individual, this response will tend to trigger only when hemoglobin oxygen saturation levels begin to reach critical values (around 85%) which corresponds to an arterial oxygen tension of around 50 mmHg.
how does nitric oxide work?
Nitric oxide acts to cause vasodilation by binding to guanylate cyclase and increasing intracellular cyclic guanosine monophosphate (cGMP). The cGMP inhibits calcium entry into cells and activates myosin light chain phosphatase. These mechanisms cause smooth muscle relaxation. Nitric oxide also has a very short half-life, at 0.05-0.1 msec.
A 42-year-old female is planned to undergo a right ankle arthroscopy for tarsal tunnel syndrome. She has no other medical problems and is a non-smoker. Her body mass index (BMI) is 31 kg/m^2. Her preoperative SpO2 in the sitting position is 98% with a pulse of 82 beats per minute and blood pressure of 139/43 mm Hg. Prior to pre-oxygenation and induction of anesthesia, she is positioned supine on the operating room table. You note a decrease in oxygen saturation to 95% over the next few minutes. Which of the following is MOST likely true regarding supine positioning for functional residual capacity (FRC) and closing capacity (CC)?
Supine positioning will decrease functional residual capacity (FRC) but has no effect on closing capacity.
what increases closing capacity?
what decreases FRC?
what is it about the supine position that leads to hypoxia quicker?
A mnemonic for factors increasing closing capacity is ACLS-S: Age, Chronic bronchitis, LV failure, Smoking, Surgery.
A mnemonic for factors that decrease FRC is PANGOS: Pregnancy, Ascites, Neonate, General Anesthesia, Obesity, Supine position.
It is important to remember that the development of hypoxemia in this patient is due to a reduction in FRC, not an alteration in closing capacity as positioning has no effect on closing capacity. This results in a reduction in the margin between the FRC and closing volume resulting in airway closure earlier in expiration. Other factors that increase closing capacity include increasing age, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), smoking, and surgery. All of these factors cause alterations in transpulmonary pressure across airways resulting in easier airway collapse at higher lung volumes
what are the positives of CPAP?

is laryngospasm suppressed more by propofol or sevoflurane?
propofol
Patients in respiratory failure are at high risk for rapid desaturation. The following techniques have been shown to enhance preoxygenation in these patients:
- Positioning the patient at 20 degrees in reverse Trendelenburg
- Attaching a nasal canula running at 15 LPM of oxygen during apnea
- Placing the patient on CPAP or BPAP, consider leaving in place during apneic period
- Using rocuronium at 1.2 mg/kg instead of succinylcholine in high-risk patients to prolong the time to desaturation
In a study of operative patients, time to desaturation to 95% was 242 seconds after succinylcholine compared to 378 seconds after rocuronium.
what are the 3 ways CO2 is transported in the blood?
bicarbonate and hydrogen ions formed following dissociation of carbonic acid (about 73% of carbon dioxide), hemoglobin-bound carbon dioxide (about 20% of carbon dioxide) and dissolved carbon dioxide (about 7% of carbon dioxide).
what is the haldane effect?
The process of oxygen binding to hemoglobin and displacing carbon dioxide from the blood is called the Haldane effect. Because of carbon dioxide being displaced from the blood, there is a downward shift in the carbon dioxide dissociation curve that takes place in physiologic settings with higher oxygen levels, such as the lungs. This facilitates the removal of carbon dioxide from the body.
what is the bohr effect?
Bohr effect, which is when an increase in carbon dioxide in the blood causes oxygen to be displaced from hemoglobin. This is an important effect taking place at the tissue level to increase oxygen transport, where higher levels of carbon dioxide displace the oxygen to the tissue and the bound carbon dioxide can now be transported via the blood to the lungs for removal. This effect will result in a rightward shift of the oxygen-hemoglobin dissociation curve.
what are the findings of an upper airway obstruction (kid swallowed something)
Lower airway?
Tracheal?
- inspiratory stridor
- Expiratory stridor
- Asthamoid wheezing, audible slap of foreign body against trachea during ventilation, and palpable thud
Advanced copd with advanced disease what are ecg findings that would should right heart strain indicative of phtn?
RBBB, right axis deviation, or peaked p waves may indicat right atrial enlargement
what is ARDS?
What is the PaO2/FiO2 ratio?
Acute respiratory distress syndrome (ARDS) is a multifactorial and complex clinical state that is the end result of an acute alveolar injury caused by any of a variety of physiologic insults. This syndrome is characterized by a diffuse capillary leak caused by a complex interaction of inflammatory cells and mediators that eventually results in a loss of effective pulmonary surfactant. These features result in markedly decreased lung compliance and atelectasis. The end result of these pathologic changes is tremendous intrapulmonary shunting resulting in potentially profound systemic hypoxemia that is refractory to increases in inspired oxygen concentrations.
Because the source of hypoxemia in ARDS is a profound shunt caused by diffuse atelectasis, the severity of the syndrome itself can be characterized by the PaO2/FiO2 ratio. According to the Berlin Definition, ARDS can be stratified into the mild, moderate, and severe ranges based upon the following PaO2/FiO2 ratios that are obtained when the patient is given a PEEP greater than 5 cmH2O: Mild 201 to 300; Moderate 100 to 200; Severe less than 100.
what is PA-a ratio? what does it do?
Arterial blood gas analysis can be used to assess for the degree of V/Q mismatching and shunt through a variety of indices such as the alveolar-to-arterial PO2 (A-a PO2) gradient and the PaO2 to FiO2 ratio (P/F ratio). The A-a PO2 ratio uses ABG analysis to determine the partial pressure of oxygen in both the alveoli (PAO2 = [FiO2 * (Patm - PH2O)] - (PaCO2/R)) and the arterial system. This ratio helps to differentiate V/Q mismatching and shunt from hypoventilation and low FiO2 as causes of hypoxemia as it is unchanged under conditions of decreased FiO2 and hypoventilation. During states of V/Q mismatching or shunt, however, is can become profoundly elevated. A normal value for this ratio is around 10 mmHg in young adults breathing room air, and will physiologically increase as patients age or FiO2 is increased above the level of room air.
In practice, the A-a PO2 gradient tends to be used to identify states of high V/Q mismatch, while the P/F ratio tends to be more used to identify states of right-to-left shunting.
what should asplenic patients be vaccinated against?
Asplenic patients should be vaccinated against encapsulated organisms, including H. influenzae B, Neisseria meningitides, and Streptococcus pneumoniae.


