Renal Pathophysiology Flashcards
How is GFR measured?
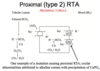
clearance of inulin or creatinine
estimates based on serum creatinine
azotemia
accumulation of nitrogenous waste products in the blood
i.e. urea
any rise in serum BUN or creatinine above normal
uremia
clinical syndrome or symptom compelx associated with severe impariment of renal function
specific gravity of urine
lower specific gravity correlated with low osmolarity (more dilute urine)


This is an example of a urine
1: Here a white cell with red blood cells around it
When you see cells in the urine you do not know if they have come from the kidney or someplace else in the urinary tract a

WBCs and bacteria in urine

tubular epithelial cell (not round like WBC)

squamous epithelial cells - from bladder ureter or urethra NOT kidney
casts
cylindrical masses of agglutinated material
formed in distal nephron, have to come from kidney
Tamm-Horsfall mucoprotein is the major protein constituent
Hyaline, granular or cellular
Where are casts formed?
distal nephron
Tamm-Horsfall mucoprotein
major protein constituent of casts
Hyaline cast
we think the hyaline cast and granular cast are degenerated cellular casts
There is a lot of other amorphous material here

tubular epithelial cell cast
you can see the shape of the cells here are not perfectly round which you would see in a white blood cell cast

broad cast
it was formed further down in the nephron, again there are red cells around this cast

coarse granular cast
notice the granules and degenerating cells

RBC cast

WBC cast

waxy cast (probably has cholesterol)

triple phosphate crystals
often in people with UTIs

calcium oxalate crystals

On the left there are stellar and amorphous Ca Phosphate crystals
On the right Ca Oxalate crystals

cysteine crystals

uric acid crystals
What does dipstick look for?
•Dipsticks (mainly picks up albumin, may miss low molecular weight and other nonalbumin proteins)
Heat and Acetic Acid for urine test?
take a specimen of urine and heat it up and if there’s protein you will see it form at the bottom of the test tube
The test tube has been heated (left) and as it cools you see the protein on the bottom
This is with heat and acetic acid but with sulfosalicylic acid it will look very similar
We don’t do this often, usually send sample off to the lab and they can measure protein or albumin
sulfosalicylic acid test for urine
detects all proteins in the urine
Microalbuminuria - how do we test?
dipsticks not positive until rel high
to find smaller amounts - use direct measrements of albumin secretion
microalbumin - to - creatinine ratio!
How do you determine the type of protein in the urine?
protein electrophoresis
glomerular proteinuria
increase in permeabilty of glomerular capillary wall leads to increased glomerular filtration of protein
tubular proteinuria
impaired reabsorption of normally filtered proteins
overflow proteinuria
increased production of smaller proteins in multiple myeloma and ther plasma cell issues
nephrotic syndrome
massive loss of normal serum proteins in the urine
- heavy proteinuria (>3.5)
- hypoalbuminemia
- edema
- hyperlipidemia
- sometimes HTN
hypoalbuminemia in nephrotic
urinary loss of protein
liver is making more but can’t keep up with loss

Why edema in nephrotic syndrome?
overfill hypothesis
glomerular disease/tubular inflammation leads to increased renal sodium retention (reabsorb mostly in collecting tubules
Why is there no hypertension in nephrotic syndrome?
Na retention USUALLY results in hypertension but nephrotic patients to not
MAY be secondary to hypoalbuminemia
Why hyperlipidemia in nephrotic syndrome?
elevated cholesterol, TG, phospholipids
low plasma albumin?
increased lipoprotein synthesis
lipiduria in nephrotic syndrome
oval fat bodies (tubular cells w fat drops)
maltese crosses (fat drops under polarized light)
on urinalysis

oval fat bodies in neprhotic synd urine
1: oval fat body (tubular cell that is filled with fat)

maltese crosses - polarized light on fat
lipid in urine in nephrotic
If you think a patient has nephrotic syndrome it is important to look at the urine for oval fat bodies and then look under polarized light
thromboembolic events
in nephrotic syndrome!
hypercoagulable state
DVT and renal vein thrombosis
Minimal Change Clinical Picture
acute onset
variable fluid retention
HTN infrequent
renal function is normal
EDEMA and protein in the urine!
urinalysis in minimal change disease
proteinuria (ALBUMIN - selective)
oval fat bodies
few cells
treatment for minimal change
high dose steroids - usually remission in 2-4 wks
membranous nephropathy presentation
insidious - asymptomatic proteinuria or microscopic hematuria
urinalysis in membranous
massive proteinuria (non selective - not just albumin)
HTN and azotemia if late
acute glomerulaonephritis presentation
follows GSA - pharyngitis or skin
gross hematuria and oligouria
edema and pulmonary congestion
flank pain
hypertension
when do you see congested circulation?
nephritic!!
renal retention of salt and water
decreased urine output
dyspnea, orthopnea, cardiomegaly, rales, gallop
urinalysis in acute glomerulonephritis
GAS rxn
hematuria (coca cola)
RBCs, RBC casts
prteinuria (low)
low urine sodium (retaining, vol overload)
very concentrated urine
treatment of acute glomerulonephritis
treat HTN
manage fluids and electrolytes
treat renal failure/dialysis
Hematuria in which syndromes/
gross - nephritic only
microscopic - sometimes nephrotic, always nephritic
hypertension in which syndromes
sometimes in nephrotic, always in nephritic
decreased GFR in which syndromes?
sometimes nephrotic
always nephritic
congestion in which syndromes
only nephritic
hypoalbuminemia in which syndromes
always nephrotic
rarely nephritic
urinalysis in UTI
pyuria and WBC casts
bacteria
urinalysis in pyelonephritis
WBCs and WBC casts
Urinalysis in acute interstitial nephritis
eosinophils
granular or WBC casts
systemic glomerulopathies
nephrotic
diabetes, amyloid
primary glomerulopathies
nephrotic
minimal change
fsgs
membranous
systemic nephritis
SLE
Endocarditis
MPGN
ANCA
kidney only nephritic
post infectious
IgA
congenital nephrotic syndrome of the newborn
finnish
severe NS at birth - all ESKD
need dialysis and transplant
because mutation in nephrin (in the podocyte slit diapragm)
how we learned about it!
secondary causes of minimal change
malignancy (Hodgkin and non-hodgkin lymphoma
drugs (NSAID, lithium, rifampin)
Infections (syphilis, malaria)
clinical presentation of minimal change
mostly children
explosive onset - edema, hypoalbuminemia
kidney biopsy to make diagnosis
treatment of minimal chagne
prednisone - usually dramatic and quick response
treat underlying secondary disease
urokinase plasminogen activating receptor (suPAR)
role in FSGS
Treatment for PRIMARY FSGS
steroids first line
most are steroid resistant
second = calcineurin inhibitors
some targetted thereapy?
recur post transplant!
secondary FSGS
secondary to other kidney disease and obesity
how does primary FSGS present?
NS or asymp prteinuria
normal or elevated BP
how does secondary FSGS present?
NON-nephrotic preinuria, decreased GFR
How do you treat secondary FSGS?
ACEI/ATR blocker
collapsing glomeruloathy etiology
variant of FSGS
characterized by dedifferentiation and proliferation of podocytes with collapse of glomerular tuft
HIV nephropathy (infects podocytes causing proliferation)
or infections, meds, malignanc
treatment of collpsing glomerulopathy
anti retroviral
correct underlying
ACEI/ARBs
APOL1
worse prognosis in FSGS, more likely to develop kidney failure in african americans
1 risk allele = prptection from trypanosomes
2 = risk for kidney failure
histopath of membraous nephropathy
characterized by C3, IgG deposits
SUBEPITHELIAL
how does membranous nephropathy present
NS or asymptomatic proteinuria
outcomes of membranous nephropathy
25% spontaneous remission
50% persistent proteinuria
25% renal failure
treatment for membranous nephropathy
ACEI/ARB
prednisone/calcineuron?
primary membranous nepropathy pathogenesis
IgG antibody to podocyte ag (PLA2R)
Ab fixes compliment and C3 is present in renal tissue
Here would be the podocyte (brownish stuff)
- Expresses the antigen (phospholipase A2 receptor)
- Ab is generated to that autoimmune antibody receptor that binds the receptor
- That then activates complement à destroys the podocyte and gives you this disease
- To remind you, an Ag-Ab complex can activate complement à which ultimately can form this membrane attack complex

PLA2R
phospholipase A2 receptor on the membrane of the podocyte
IgG ab bonds to it and fixes comp
Here would be the podocyte (brownish stuff)
- Expresses the antigen (phospholipase A2 receptor)
- Ab is generated to that autoimmune antibody receptor that binds the receptor
- That then activates complement à destroys the podocyte and gives you this disease
- To remind you, an Ag-Ab complex can activate complement à which ultimately can form this membrane attack complex

secondary membranous nephropathy pantogenesis
trapping of preformed antibody-angigen complexes leading to fixation of complement and podycte damage
SLE
syphilis
malaria
hep B
drugs
tumor
rapidly progressive glomerulonephritis (RPGB)
presentations OF nephritic syndrome that are emergent
based on percent of cresecents (not time!!)
require urgent treatment
post infectious glomerular nephritis
small circulating immune complexes of low-avidity antibody an oligovalent angigen (any infection can cause)
clinical presentation of post infections GN
nephritic syndrome 1-2 wks after strep infection (skin, throat)
pathology of post infectious GN
subepithelial deposition of immune complexes
granular on immunoflorscence
clinical course of post infectious gn
most recover in a couple weeks
control - BP, diuresis, infection
IgA nephropathy pathology
mesangial IC deposits
with IgA and usually C3 and IgG
- Shown biopsy with immunofluorescence
- Slice of kidney à primary Ab against IgA, IgG or IgF à secondary Ab with something that can be detected fluorescently
- In this case see IgA deposited in kidney in mesangium and around glomerular capillaries (L piecture)
- You also see complement (R picture)
- This would be enough to give you a dx of IgA nephropathy

pathogenesis of IgA nephropathy
- incrased levels of galactose deficienct IgA
- production of unique auto antibodies
- formation of pathogenic IgA contianing ICs circulating
- mesangial deposition and glomerular injury
Somehow you get this galactose-deficient IgA à produce unique auto antibody à some systemic (maybe driven by a third factor like infection) à deposition of immune complex à activate immune response à inflammation

membranoproliferative glomerulonephritis causes
hep B, hep C, malignancy, eds
can present w systemic signs of vasculitis and renaly insufficiency and nephritic syndrome
skin rash etc
treat underlying
ANCA associated vasculitis
antibodies to proteins expressed in neutrophil
binding of abs to neutrophil plasma membrane leads to neutrophil activation which causes kidney disease
get autiantibodies by molecular mimicry - present protein that looks like self
treatment of ANCA-associated vasculitis
cancer model
inductions (steroids and abs)
plasmapheresis if severe renal impairment
interfere w immune system
anti-gbm mediated glomerularnephritis
i.e. goodpastures (+ pulmonary hemorrhage)
auto antibodies against alpha3 chain of collagen IV in renal and lung BM
ab activates compliment
presentation of anti-GBM mediated GN
oliguria
advanced renal failure