Random 1 Flashcards
What a painful 3rd nerve palsy may be suggestive of?
Posterior communicating artery aneurysm
e.g. 3rd nerve palsy + headache
What muscles are affected in 3rd nerve palsy?

- Lateral rectus* + superior oblique -> unopposed action = eye down and out
- Levator palpebrae* = ptosis
What may be the cause of:
3rd nerve palsy (ptosis + eye down and out) + pupil dilation
microvascular cause (e.g. compression/aneurysm)
also look for: neck stiffness, vomiting and headache) -> an aneurysm compressing on posterior communicating a.
Where would be the lesion localised if:
3 rd nerve palsy (ptosis) + upgaze
Midbrain
Where would be the lesion localised if:
ptosis + ataxia + hemiparesis
midbrain
Location of the lesion if:
facial pain, numbness (forehead) + 3rd nerve palsy + decreased corneal reflex
Cavernous sinus #

What’s Weber’s syndrome?
Weber’s syndrome:
ipsilateral third nerve palsy with contralateral hemiplegia -caused by midbrain strokes
Autonomic dysreflexia
- symptoms and signs
- at which level of spinal cord injury does it occur?
Autonomic dysreflexia
Spinal cord injury: above T6 level
Presentation: a combination of severe hypertension, flushing and sweating without a response in heart rate in the context of spinal cord injury -> autonomic dysreflexia
What is the cause of autonomic dysreflexia in a person with spinal cord injury and when (example) a catheter is placed?
Cause: discontinuity between the nociceptors on the viscera and the brain stem autonomic centres due to the cord injury
- all the pain receptors on smooth muscle on the abdominal and some pelvic viscera are carried by the sympathetics
- the specific nerve which extends to the pelvis is the greater splanchnic nerve (which has its lowest innervation at T6 and so this is the lowest level at which autonomic dysreflexia can still occur)
Patient with unilateral deafness or tinnitus
What condition do we need to consider?
Acoustic neuroma
*also may present with facial palsy
* requires urgent referral for ENT surgery
What is the nature of symptoms in Presbycusis?
Bilateral
When otitis media may be excluded - examination wise
The normal ear examination and Rinne’s/Weber’s tests suggesting a sensorineural deafness
Typical history of vestibular schwannoma (acoustic neuroma)
The classical history of vestibular schwannoma includes a combination of: vertigo, hearing loss, tinnitus and an absent corneal reflex.
Features can be predicted by the affected cranial nerves:
- cranial nerve VIII: vertigo, unilateral sensorineural hearing loss, unilateral tinnitus
- cranial nerve V: absent corneal reflex
- cranial nerve VII: facial palsy
What are (5) sinister signs of headache?
*what to do?
Sinister signs of headache
- Vomiting more than once with no other cause
- New neurological deficit (motor or sensory)
- Reduction in conscious level (GCS)
- Valsalva (associated with coughing or sneezing) or positional headaches
- Progressive headache with a fever
Do an urgent CT head scan
CSF flow

Essential tremor
- what’s the cause
- management
Essential tremor
Cause: an idiopathic, mixture of genetic and environmental factors (no specific gene has been identified yet)
Management:
(depend on Rx severity - not all require treatment)
- lifestyle: cut down on caffeine, avoid stress, good sleep
- Meds:
1st line -> B blockers -> propranolol
2nd anti-epileptics: topiramate, gabapentin or other alternatives
3rd line -> mirtazapine, clonazepam
- if meds do not help: botulinum toxin, deep brain stimulation and occupational therapy input
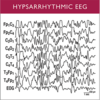
Hypsarrhythmia on EEG is suggestive of which type of seizure?
Hypsarrhythmia
- seen in infantile spasms or West’s syndrome
- It has a poor prognosis and regression in skills often occurs
- Hypsarrhytmia - is defined as continuous, high-amplitude, arrhythmic, asynchronous delta activities with interspersed independent, multiple spikes
Thrombolysis
- (2) criteria
- Drug used
Thrombolysis should only be given if:
- it is administered within 4.5 hours of onset of stroke symptoms (unless as part of a clinical trial)
- haemorrhage has been definitively excluded (i.e. Imaging has been performed)
Alteplase is currently recommended by NICE.


