Porth: Chpt. 28 Flashcards
What is the GI Tract also referred to as?
- Digestive Tract
- Alimentary Canal
- Gut
What is the Intestinal Portion of the GI Tract called?
- Bowel
Name the Accessory Organs that produce secretions & aid in digestion?
- Pancreas
- Liver
- Salivary Glands
Major Physiologic Functions of the GI Tract
- Digest food
- Absorb nutrients
How does the GI Tract carry on the functions of digestion & absorption?
- Motility
- Secretion
- Digestion
- Absorption
What happens to the Unabsorbed Nutrients & Wastes in the Large Intestine?
- Collected
- For later elimination

What must Nutrients do in order to become part of the body’s Internal Environment?
- Pass through Intestinal Wall
- Enter Blood & Lymph Channels
For Simplicity’s Sake:
What are the 3 parts of the GI Tract?
- Upper part
- Mouth, Esophagus, Stomach
- Intake source & Receptable
- 1st portion of digestive process
- Mouth, Esophagus, Stomach
- Middle part
- Duodenum, Jejunum, Ileum
- Digestion & Absorption!
- Duodenum, Jejunum, Ileum
- Lower part
- Cecum, colon, recturm
- Storage channel
- Elimination of waste
- Cecum, colon, recturm
Which President signed Father’s Day into Law?
- 1966, President Lyndon B. Johnson issued the first presidential proclamation honoring fathers, designating the third Sunday in June as Father’s Day.
- Six years later, the day was made a permanent national holiday when President Richard Nixon signed it into law in 1972.
What does Saliva do?
- Moisten & lubricates food
- Eaiser to Swallow
- Enzymes
- Initial digestion of Lipids and Starches
The Esophagus
- 25cm, straight, collapsible tube
- Connects oropharynx w/ stomach
- Conduit for passage of food
- Smooth muscle = Peristalsis!
- Mucosal/Sub-mucosal glands = Protects surface, lubricates food
The Esophagus
&
Its Sphincters
- 2: Upper & Lower
-
Upper = pharyngoesophageal
- Striated muscle
- Keeps air from entering stomach
-
Lower = gastroesophageal
- Circular muscle
- Tonically contracted
- Zone of high pressure
- Prevents reflux
- Passes through hiatus in diaphragm to join w/ stomach
-
Upper = pharyngoesophageal
The Esophagus
&
“Receptive Relaxation”
-
Lower = gastroesophageal sphincter
- Allows propulsion of esophagus contents into stomach
- Hiatus region = high pressure
- Prevents reflux

The Stomach
-
Pouchlike structure
- Food storage reservoir

The Stomach
+
Cardiac Orifice
Where esophagus opens into stomach

The Stomach
+
Pyloric Sphincter
End of pyloric canal
Circular, Smooth muscle
Valve = controls rate of stomach emptying
+ Prevents regurgitation of intestinal contents into stomach
Middle GI Tract
-
Duodenum:
- 22cm long
- Connects Stomach to Jejenum
- Opening for Common Bile Duct + Main duct
- Juices enter via ducts
-
Jejunum & Ileum:
- 7m (23ft) long [folded]
- DIGESTION & ABSORPTION!
Lower GI Tract
- Large intestine = 1.5m (5ft) long
- Cecum, Colon, Rectum, Anal Canal
- Cecum = Pouch @ junction btwn Ileum & Colon
- Valves - prevent return of feces into small intestine
- Appendix = 1in from ileocecal valve
- Colon
- Descending colon extends to rectum
- Rectum = sigmoid colon to anus
- Anal Canal = btwn levator ani muscles
- Spinchter muscles = no incontinence
How fast does a crack in glass travel?
When glass breaks, the cracks move faster than 3,000 miles per hour!!!
GI Wall Structure
The Digestive Tract is a __________ tube

-
Four-Layered Tube
- Inner Mucosal Layer
- Epithelium, Lamina propria, Muscularis mucosa
- Submuscosal (2nd layer)
- Connective & Adipose
- Muscularis externa (3rd layer)
- Serosal (4th layer)
- Mesothelium (squamous)
- Inner Mucosal Layer
GI Wall Structure
Inner Mucosal Layer - Functions
- Lubricates & Protects inner surface of alimentary canal
- Secretes digestive enzymes
- Break down food
- Absorb breakdown products
- Prevents entry of bad substances
- Lymphatics in here = 1st line of defense
GI Wall Structure
Inner Mucosal Layer - Epithelial Lining
- Rapid turnover rate
- Replaced q 4-5 days
- Heals rapidly
- No scar tissue
GI Wall Structure
Second Layer - Function
- Secretes digestive enzymes
- Has lots of vasculature
GI Wall Structure
Third Layer - Function
- Circular smooth muscle cells
- AND
- Longitudinal smooth muscle cells
- =’s
- Facilitate MOVEMENT of GI Tract contents
- =’s
GI Wall Structure
Fourth Layer - Function
- Equivalent to:
- Visceral Peritoneum
- Most superficial layer of digestive tract parts suspended in peritoneal cavity

The Peritoneum
Largest serous membrane in the Body!
2 layers;
- Visceral
- Parietal
The Peritoneum
What is between the 2 layers of the Peritoneum?
Peritoneal Cavity!
“Potential Space containing serous membrane fluid”
Moint & Slippery Surface - preventing Friction!
The Mesentery
Double layer of peritoneum
Encloses abdominal viscera & attaches it to the abdominal wall
-
Contains: Blood vessels, nerves, lymph vessels
- Supply intestinal wall
- Holds organs in place
- Stores Fat

The Omentum
- Double-layered extension of peritoneum
- Passes from stomach or proximal part of duodenum to adjacent organs in abdominal cavity/wall
- Greater Omentum
- Lesser Omentum

The Omentum
Greater Omentum Functions
- Contains fat
- can be A LOT in obese people
- Mobile
- Moves around in cavity w/ peristatsis of intestine
- Forms adhesions
- Fiborous scar tissue
- Walls of infection & prevents spread
- Cushions & Insulates!

Which Continent contains the most Deserts?
- Antarctica
- Antarctica is considered a desert, with annual precipitation of only 200 mm (8 inches) along the coast and far less inland

The movements of the GI Tract can be:
Rhythmic & Tonic
-
Rhythmic
- Intermittent contractions
- Mix & Moves food along tract
- esophagus, antrum, small intestine
-
Tonic
- Constant level of contraction w/o relaxation
- lower esophagus, upper stomach region, ileocecal valve, internal anal sphincter
What parts of the GI Tract are NOT made of Smooth Muscle?
- Pharynx
- Upper 1/3 of Esophagus
- External Anal Sphincter
Basic Properties of the GI Tract Smooth Muscle
- Cells electronically coupled by low-resistance pathways
- =’s electrical signals that contract muscle move quickly from one fiber to the next!
- Pacemaker cells
- Rhythmic, spontaneous oscillations
- SLOW WAVES
- Enteric Nervous System run this
- Located in GI Tract wall
- PNS and CNS
- Peptides, NTs, Hormones assist in Motility!
- Rhythmic, spontaneous oscillations
Enteric Nervous System
- Myenteric & Submucosal Plexuses in wall
- Nerve fibers & ganglion cell bodies
Enteric Nervous System
Myenteric Plexus
- Linear chain of interconnecting neurons
- Btwn longitudinal & circular msucle layers
- Runs all way down wall
- Motility along length of gut!

Enteric Nervous System
Submucosal Plexus
- Btwn mucosal & muscle layers of intestine
-
Controls function of each segment of intestinal tract
-
Local control of
- Motility
- Intestinal Secretions
- Nutrient Absorption
-
Local control of

Enteric Nervous System
Myenteric & Submucosal Plexuses
Regulation
- Local influences
- Input from ANS
- Interconnecting Fibers transmit Info
- Mechanoreceptors
- Monitor stretch & distention
- Chemoreceptors
- Monitor chemical composition (pH, osmolality…)
Which Insect has the Longest Life Span?
A queen termite has been known to live 50 years….gross!

What mediates the Autonomic NS of the GI System?
Sympathetic & Parasympathetic NS
- Parasympathetic NS = Increase in Enteric NS activity
- Sympathetic NS = Inhibits Activity
Parasypathetic Inneveration occurs through what nerve?
Vagus Nerve
(+ some of the colon is innvervated by fiber that exits via sacral region of spinal cord)
Preganglionic Parasympathetic Fibers
Synapse w/ Plexus Neurons
(or) Act directly on Intestinal Smooth Muscle
+ Provide afferent nerves!
Receptors lie w/in various gut tissue
These nerves project to spinal cord & brain
=’s Sensory Input for Integration
Most Parasympathetic Innervation is….
Excitatory!
How does Sympathetic Innveration occur?
Via Thoracic chain of sympathetic ganglia, superior mesenteric, inferior mesenteric ganglia.
Sympathetic Innveration
- Controls extent of mucous secretion by mucosal glands
- Reduces motility
- (inhibits activity of intramural plexus neurons)
- Enhances sphincter function
- Increases vascular smooth muscle tone of blood vessels
Sympathetic Innveration
&
Its effect
Blocks release of the excitatory neuromediators in intramural plexuses, which inhibits GI Motility!

What begins the Digestive Process?
Chewing!
Breaks food into small particles to swallow
Lubricates it w/ salvia
Mixes starch food w/ Salivary Amylase

Swallowing…
Voluntary, or Involuntary?
- Initiated as Voluntary
- Becomes involuntary when reach Pharynx

Where is the “Swallowing Center”?
- Reticular formation of the medulla and lower pons
- Responds to the Tactile receptors in pharynx & esophagus
- Turns into motor response via Medulla & Pons
- Responds to the Tactile receptors in pharynx & esophagus
What nerves carry out the Swallowing Phases?
- V, IX, X, XII
- oral & pharyngeal
- X
- esophageal
If you damage the nerves that help you swallow - What are you at risk for?
- Asphyxiation
- Aspiration pneumonia
Three Phases of Swallowing
- Oral
- Voluntary
- Bolus touches pharynx
- Pharyngeal
- Epiglottis covers larynx
- Bolus moved by constrictive pharynx movements
- Involuntary!
- Esophageal
- Peristalsis triggered as Esophagus walls are stretched
2 Types of Peristalsis
- Primary
- Controlled by swallowing center
- When food enters esophagus
- Secondary
- Mediated by smooth muscle fibers
- Occurs when primary is inadequate
Where does Peristalsis begin and go?
- Begins: Site of distention
- Goes: Downward
- Before wave reaches stomach
- Lower esophageal sphincter relaxes & allows bolus to enter stomach
- Before wave reaches stomach
Why is it good to have greater pressure in the lower esophageal sphinter versus the stomach?
To PREVENT REFLUX of gastric contents

What’s the difference between a dirty old bus station and a lobster with boobs?
One’s a crusty bus station, and the other is a busty crustacean.

What is the creamy mixture of food in the stomach called?
Chyme

What is the Volume of an Empty Stomach?
& How big can it expand to?
- 50mL = empty
- 1000 mL (before intraluminal pressure rises)
Motility of the Stomach results in….
- Churing & mixing of solid foods
- Regulates emptying of chyme into duodenum
- Begins in Pacemaker area in middle of stomach
- Moves to Antrum (contractions increase)
- Pyloric sphincter is contracted during antral contraction
- Gastric contents emptied into dueodenum btwn contractions
Pyloric Sphincter constriction prevents
- Backflow of gastric contents
- Allowing them to flow into duodenum at a good speed/rate
Why is the prevention of backflow into the stomach important?
- Backflow of bile salts & duodenal contents =
- Damage of mucosal surface of antrum
- ULCERS!!
- Damage of mucosal surface of antrum
Neural & Humoral Signals
- Regulates stomach emptying
- Signals from stomach & duodenum
- DUODENUM = gives the strongest signals
- signals at rate to digest & absorb chyme
What slows Gastric Emptying?
- Hypertonic Solutions in the Duodenum
- Duodenal pH below 3.5
- Presence of Amino Acids, Peptides & Fatty Acids in Duodenum
Stimulation of Gastric Emptying
- Enteric NS & PNS, SNS connections mediate reflexes
- Hormones:
- Cholecystokinin & Glucose-dependent insulinotropic peptide
- slow emptying
- Cholecystokinin & Glucose-dependent insulinotropic peptide
Stimulated by: Fats (& other foods)
If Gastric motility is TOO SLOW due to Obstruction or Gastric Atony what can occur?
- Gastric Retention
Obstruction can be due to:
- Formation of Scar Tissue in pyloric area after a Peptic ulcer
- Hypertrophic Pyloric Stenosis
- in infants w/ thick muscularis layer in terminal pylorus
-
Treatment:
- Myotomy - Surgical incision of muscular ring

Gastric Atony
- Can occur as complication of Visceral Neuropathies in DM
- Distruption of Vagal Activities
Abnormally Fast Emptying
-
“Dumping Syndrome”
- Surgical complications
- characterized by:
- Rapid dumping of highly acidic & hyperosmotic gastric secretions into Duodenum & Jejunum

What is the National Animal of Scotland?
UNICORN!!!!

Small Intestine
Major site for what?
Digestion & Absorption of food
Movements = mixing + propulsive
Small Intestine
2 Patterns of contractions
- Segmentation
- Peristaltic
Small Intestine
Segmentation Contractions
- Slow contractions
- Circular muscle layer
- Occlude lumen
- Drive contents forwards & backwards
- Most = local contractions
- Freq increases after meals
- Mix chyme + digestive enzymes
- & ensure absorption occurs
Small Intestine
Peristaltic Movements
- Rhythmic, propulsive
- Propels chyme along small intestine towards large
- Smooth muscle contracts -> Contractile band forces intraluminal contents forward
- Regular movements begin in deodenum near the common & hepatic ducts
- Propulsive & synchronized
- then relaxation…
- Propelled to ileocecal junction
- Sphincter relaxes & fluid goes into cecum
- Propulsive & synchronized
What is a simple way to assess bowel activity?
- Auscultation
- Inflammatory changes often increase activity
- Transient interruption can occur post-GI surgery
Colon Movement & Defecation!
-
2 types of colon movements:
-
Haustrations
- Segmental Mixing Movements
- occur in haustra (sacculations)
- “Digging type action”
- Exposes all portions of fecal mass to intestinal surface
-
Propulsive Mass Movements
- Large colon segments contract as a unit
- Last ~30seconds & 2-3min relax
- Series lasts ~10-30 minutes several times a day
-
Haustrations
Defecation is initiated by what?
& What’s its transit time?
& Normal Stool Weight?
- Mass movement
- Transit: 24-48 hours
- Weight: 250g/day
What 2 Sphincters control action of defecating?!
- Internal Anal
-
External Anal
- Controlled by pudendal nerve (somatic NS)
- Voluntary Control
What Reflexes control Defecation?
- Defecation Reflexes!!
-
1. Intrinsic Myenteric Reflex
- Mediated by enteric NS
- Intiated by rectal wall distention
- Mediated by enteric NS
-
2. Parasympathetic Reflex
- Sacral Cord
-
1. Intrinsic Myenteric Reflex
- Impulses increase peristaltic movements & relax the Internal Sphincter

Thank you Cortex for…..
Preventing Involuntary Defecation !
(via Conscious Control - Constricting the External Sphincter)
The cortex is alerted of a distended rectum via Afferent impulses arriving to let it know…
& Afferent impulses get tired sometimes… Ceasing urge to defecate!
Which Dr. Suess Book has exactly 50 words in it?
Green Eggs and Ham!

GI Hormones
What is the Largest Endocrine Organ in the Body?
GI Tract
GI Hormones
Where do the GI Hormones go?
Everywhere!
- Locally
- Pass into general circulation
- Interact w/ CNS via enteric & autonomic NS
GI Hormones
What are some of them?
- Gastrin
- Ghrelin
- Secretin
- Cholecystokinin
- Incretin Hormones
- GIP
GI Hormones
What do they influence?
- Appetite
- GI Motility
- Enzyme activity
- Electrolyte levels
- Secretion & Action of other hormones

GI Hormones
Stomach Hormones
- Gastrin
- Ghrelin

GI Hormones
Stomach Hormones
Gastrin
- Gastrin
- Produced by: G cells
- Fxn: Stimulation of gastric acid secretion
- Growth producing effect on mucosa of small intestine, colon, & acid secreting area of stomach
- Removal of gastric producing tissues causes atrophy to these regions
GI Hormones
Stomach Hormones
Ghrelin
- Ghrelin
- Potent growth-releasing activity
- Stimulatory effect on food intake & digestive fxn
Random fact: Isolation of this hormone = bringing insights into gut-brain regulation of growth hormone secretion & energy balance
GI Hormones
Intestine Hormones
- Secretin
- Cholecystokinin
- Incretin

GI Hormones
Intestine Hormones
Secretin
- Secretin
- Secreted by S Cells in duodenum & jejenum
- Inhibits gastric acid secretion
- Chyme presence stimulates secretin
- Which then inhibits gastrin release
- Chyme presence stimulates secretin
- Stimulates Pancreas to secrete fluid w/ [high bicarb. & low Cl]
GI Hormones
Intestine Hormones
Cholecystokinin
- Cholecystokinin
- Secreted by I cells
- Stimulates pancreatic enzyme secretion
- Potentiates action of secretin
- Stimulate biliary secretion of fluid & bicarbonate
- Regulates gallbladder contraction & gastric emptying
- Inhibit food intake (Mediator for appetite & meal size control!)
GI Hormones
Gut-Dervied Hormones
- &*
- the Incretin Effect*
- Incretin Effect
- Increase insulin release after an oral glucose load
- Gut-derived factors can stimulate insulin secretion after a high carb meal
- 2 Hormones involved:
- GLP-1
- GIP
- Increase insulin release after an oral glucose load
GI Hormones
Gut-Dervied Hormones
- &*
- the Incretin Effect and the hormones GLP-1 & GIP*
- GLP-1 & GIP
- Augment insulin release in a glucose-dependent manner
- Targets as possible: Anti-diabetic drugs
- GLP-1
- suppress glucagon release
- slow gastric emptying
- augment net glucose clearance
- decrease appetite & body weight
What does CHARGOGGAGOGGMANCHAUGGAGOGGCHAUBUNAGUNGAMAUGG mean?
It means “you fish on your side, I fish on my side, and no one fishes in the middle.”
There’s a Native American lake named Chargoggagoggmanchauggagoggchaubunagungamaugg.
This lake is located in Webster, Massachusetts.

2 Basic Functions of Secretory Glands
in the GI Tract
- Production of mucus to lubricate & protect mucosal layer of tract wall
- Secretion of fluids & enzymes to aid in digestion & absorption of nutrients
GI Secretions
Each day 7000mL of fluid is secreted into GI tract & 50-200mL leaves in stool.
- Secretions = water + [Na & K]
- Excessive secretion or impaired absorption = Extracellular fluid deficit
GI Secretions
What influences the secretory & digestive functions?
- Local
- Humoral
- Neural
- via ANS
- Secretion increases w/ parasypathetic activity (like motility)
- Inhibited by sympathetic
- pH, osmolality, chyme - stimuli for neural & humoral mechanisms
Salivary Secretions
- Salvia is secreted
- Remember your glands from Anatomy!
- Parotid, submaxillary, buccal….
-
3 fxns:
- Protection & Lubrication
- Muscus (sublingual & buccal glands)
- Protective antimicrobial action
- Lysozyme
- Ptyalin & Amylase
- Initiate digestion of starches
- Protection & Lubrication
Salivary Secretions
- ANS regulates secretions
- Parasympathetic = incrases flow
- Sympathetic = decreases
- Dry mouth? Thank your sympathetic NS
- Mumps (parotitis)
- Parotid gland infection
- Can occur in ill person w/ bad oral hygiene
Gastric Secretions
- Stomach has mucus secreting cells & others:
- Pariteal (oxyntic) cells
- Secrete HCl & Intrinsic factor
- Chief cells
- Secrete pepsinogen
- Initiates protein-breakdown
- Secrete pepsinogen
- G cells
- Secrete Gastrin
- Pariteal (oxyntic) cells

Gastric Secretions
Pariteal (oxyntic) cells
- Secrete HCl & Intrinsic Factor
- Approximately 1 Billion cells in stomach
- Produce & Secrete 20mEq of HCl in several hundred mL of gastric juice/hour
- Intrinsic Facor
- Absorbs Vit. B12
Gastric Secretions
Gastric Mucosa Characteristics
- Resistant to highly acidic secretions it produces
- When damaged (via nsaids, etoh, bile), Hydrogens move into tissue & accumulate
- pH decreases
- Ezymmatic reactions impaired
- Structures disrupted
- Results in:
- Ischemia, vascular statsis, tissue necrosis
- When damaged (via nsaids, etoh, bile), Hydrogens move into tissue & accumulate
Gastric Secretions
Gastric Mucosa Characteristics
- Protected by Prostaglandins
- Aspirin & NSAIDs decrease PG synthesis…
- =’s impairs integrity
- Aspirin & NSAIDs decrease PG synthesis…
The average person spends 2 weeks of their lifetime waiting for the light to change from red to green.
Isn’t that refreshing?

Gastric Acid Secretion
What cellular mechanism is in charge of the HCl secretion in the Parietal Cells?
- Hydrogen Ion (H+)/Potassium Ion (K+)-ATPase Transporter
+
- Chloride Ion (Cl-) channels
- (in the Luminal membrane)
Gastric Acid Secretion
HCl Secretion Process
Pt. 1
- CO2 combines with H2O
- catalyzed by carbonic anhydrase
- Forms carbonic acid
- Turns into H+ + HCO3-
- H+ + Cl- secreted into stomach
- HCO3- moves out of cell & into blood
- Turns into H+ + HCO3-
- Forms carbonic acid
- catalyzed by carbonic anhydrase
Gastric Acid Secretion
HCl Secretion Process
Pt. 2
- HCO3- =’s alkaline increase (^pH) occuring after meal
- Proton pump (H+/K+-ATPase Transporter) moves H+ into stomach
- Cl- follows (via diffusion in luminal membrane)
Gastric Acid Secretion
Proton Pump Inhibitor (PPI) Function
- Inhibit gastric acid secretion by binding irreversible to sulfhydryl groups of H+/K+-ATPase transporter
- Treat Acid Reflux & Peptic Ulcer
Gastric Acid Secretion
3 Substances that Stimulate HCl secretion
- ACH (from vagal nerves)
- Gastrin (G cells)
- Histamine (endocrine cells)
Each bind to a different Parietal cell & different MOA, BUT:
-stimulate increase of H+ via Proton Pump

Gastric Acid Secretion
H2 Receptor Blockers function
- Treats peptic ulcer & GERD
- Binds to H2 Receptors & blocks action of Histamine on Parietal Cells
Gastric Acid Secretion
Prostaglandin E2
- Inhibits acid secretion & simulates mucous production
- Important in: Maintenance of Gastric Mucosal Barrier!
Intestinal Secretions
Small Intestine
- Secretes digestive juices & recieves secretions from liver & pancreas
Intestinal Secretions
Brunner Glands
- Mucus-producing glands
- Concentrated:
- where contents from stomach & secretions from liver + pancreas enter the duodenum
- Secrete alkaline mucus
- Protects from duodenum from acidic content
- Influenced by ANS
- Concentrated:
Intestinal Secretions
Brunner Glands
Activity Example
+ Peptic Ulcer FYI
- Sympathetic stimulation
- Marked decreased in mucous production
- =’s more susceptible to irritation
- Between 75-80% of Peptic Ulcers occur at this site
Intestinal Secretions
Mucus + other Secretions in the Small Intestine….
- 1. Mucus secretions
-
2. Serous fluid
- pH 6.5-7.5
- secreted by crypts of Liberkuhn
- ABSORPTION Vehicle
-
3. Surface Enzymes
- Aid in absorption
- Ex: Peptidases & Disaccharidases
Intestinal Secretions
Mucus + other Secretions in the Large Intestine….
- Secretes only mucus (usually)
- ANS activity = influencer
Intestinal Secretions
Mucus Secretion in the Large Intestine, pt. II
- Intense Parasympathetic Stimulation
- Mucus secretion increases so much, that stool contains lots of mucus
- When bowel irritated or inflamed:
- Water & Electrolytes lost in large quantities
How long do Taste Buds last for?
Taste buds go through a life cycle where they grow from basal cells into taste cells and then die and are sloughed away.
Taste Bud’s normal life cycle is anywhere from 10 days to two weeks.

Intestinal Flora
Major functions
- Gut = natural habitat of tons of bacteria
- Metabolic activites
- salvage energy & absorbable nutrients
- trophic effects on intestinal epithelial cells
- protection of colonized host against invasion of pathogenic organisms
Intestinal Flora
Stomach & Small Intestine
- Contain only a few species of bacteria
- B/c composition of luminal contents kills most microorganisms
- & B/C constant propulsive movements of this area
Intestinal Flora
Large Intestine
- Large & Complex Ecosystem
-
300-500 different species of intestinal bacteria
- Anaerobic bacteria > Aerobic Bacteria
Intestinal Flora
Colon-ization!
- Begins post-partum
- Influenced by:
- Passage through birth canal
- Infant’s diet
- Other Environmental factors
- Influenced by:
Intestinal Flora
Major Metabolic Function
- Ferments of undigestable dietary residue & endogenous mucus
- Fermentation of non-digestable carbs (starches, cellulose, pectins…) =’s
- Major source of Energy!!
- Fermentation of non-digestable carbs (starches, cellulose, pectins…) =’s
- Vitamin Synthesis
- Absorbs Ca, Mg, Fe
- Line of resistance to colonization by exogenous microbes
- Protective!
Intestinal Flora
Metabolic Endpoint
- Generation of short-chain fatty acids
- =’s aid in epithelial growth & differentiation
Intestinal Flora
Broad-Spectrum Abx
- Administration of broad-spectrum abx
- disrupts microbial balance
- allows overgrowth of species that can be BAD!
- ex: C. diff
Intestinal Flora
Probiotics
- Increasingly recognized
- Supplement to normal diet + treatment use
- Live microorganisms
- When ingested - modify composition of enteric microflora
- Common ones:
- lactobacilli, bifidobacterida, non-pathogenic E. coli
- Valuable in some diseases:
- ex: Remission in Ulcerative Colitis!
Digestion
Process of dismantling foods into constituent parts.
Digestion
Requirements
- Hydrolysis
- Breakdown of compound involves H2O
- Enzyme cleavage
- Fat Emulsification
Digestion
Intestines are impermeable to
- Large Molecules!
- Proteins, Fats, Carbs
- must be broken down
- Proteins, Fats, Carbs
Digestion
Intestines are impermeable to
- Large Molecules!
- Proteins, Fats, Carbs
- must be broken down
- Proteins, Fats, Carbs
Digestion
Digestion mainly takes place in….
The Small Intestine!!
- Fats to free fatty acids
- Monoglyceride breakdown
The liver & pancreas supply digestive enzymes & help out!
Digestion
Absorption
Process of moving nutrients & other materials from external environment in the lumen of the GI Tract into the Internal Environment
Digestion
Absorption- Accomplished by
Active transport & diffusion
Digestion
Absorption
Large Intestine Absorption
Focuses mainly on water reabsorption
Digestion
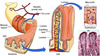
Distinguishing factor of the Small Intestine
LARGE Surface Area
(~250 m2)
Large b/c circular folds & MANY Villi!
Digestion
Villi of the Small Intestine
Contain:
- Artery
- Vein
- Lymph Vessel
- Bring blood to surface of intestine &
- Transport nutrientns & other materials
Digestion
Villi of the Small Intestine
&
Enterocytes + Mucus
- Covered in cells called Enterocytes!
- __Absorption & Digestion
- Goblet Cells
- Mucus
Digestion
Villi of the Small Intestine
&
Crypts of Lieberkühn
- Crypts of Lieberkühn
- Glandular structures that open into villi spaces
- New (replacement) enterocytes are created here
Digestion
Villi of the Small Intestine
&
Brush Border Enzymes
- Enzymes that aid in Carb & Protein digested
- Secreted by Enterocytes
- Stick to border of villus structures & eat up the carbs and protein as they come in contact w/ the intestine surface
Digestion
Villi of the Small Intestine
&
Where do digested Molecules go?
- Diffuse through membrane
- or
- Actively transported across mucosal surface to enter blood (fatty acids enter luteal)
- Molecules are transported through portal vein or lymphatics into systemic circulation
What Animal is the Sleepiest in the World?
The koala sleeps 22 hours a day!
Next is the sloth (20 hours), armadillo and opossum (tied at 19 hours each), lemur (16 hours), then hamster and squirrel (tied at 14 hours each).

Carbohydrate Digestion & Absorption
- Carbs must be broken down into
- Monosaccharides
- (before absorption!)
- Monosaccharides
Carbohydrate Digestion & Absorption
Begins with the Action of…..
-
Amylase!
- Pancreatic secretions contain this.
- Breaks down starch into disaccharides.
Carbohydrate Digestion & Absorption
Amylase breaks down Starch, then….
-
Brush Border Enzymes
- Break down Disaccharides into Monosaccharides
Carbohydrate Digestion & Absorption
If Disaccharides cannot be Broken down:
- Cannot be absorbed
- Remain osmotically acitve particles
- Causing:
- Diarrhea
- Causing:
- Remain osmotically acitve particles
Carbohydrate Digestion & Absorption
Carbohydrate Breakdown chart

Carbohydrate Digestion & Absorption
What occurs when people have a lactase deficiency?
- They cannot break down lactose
- So when they have dairy products (milk, etc..) =’s
- Diarrhea
- So when they have dairy products (milk, etc..) =’s
Carbohydrate Digestion & Absorption
Water absorption in the intestine is linked to?
- Absorption of osmotically active particles
- (glucose & sodium)
So - if you are having bowel disruptions, include glucose & sodium in fluids being consumed to decrease diarrhea
Fat Digestion & Absorption
What is the main type of Fat the average adult eats daily?
- Triglycerides
Fat Digestion & Absorption
First step in Lipid digestion
- Break down large globules of dietary fat
- Make smaller particles
- so H2O soluble digestive enzymes can act on them
- Make smaller particles
Fat Digestion & Absorption
Emulsification
- Breaking down of lipids to smaller particles
- Begins in the stomachs, continues in duodenum
- Bile from liver helps!
- Exposes lipids to pancreatic lipase =’s
- Creates free fatty acids & monoglycerides
Fat Digestion & Absorption
Bile Salts Role
- Form Micelles
- Transport broken down lipids to intestinal villi
Fat Digestion & Absorption
What occurs when broken down Fats are brought to the Intestinal Villi?
- Taken into epithelial cells & form NEW TRIGLYCERIDES!
- Released into the lymphatic system (as chylomicrons)
(& some fatty acids are instead absorbed directly into portal blood - instead of becoming triglycerides)
Fat Digestion & Absorption
What do you call Fat that is NOT absorbed into the Intestine?
-
Steatorrhea
- Excreted in the stool
- >20g+ of fat in stool in a 24-hour stool sample

The Chapter is almost DONE!!
Wahoo!

Protein Digestion & Absorption
Begins where? & Who is the main player?
- Begins in the: Stomach
- Player: Pepsin
[Pepsinogen (enzyme precursor to pepsin) = secreted by chief cells in response to a meal & acid pH –> Acid is required to convert to Pepsin.]
Protein Digestion & Absorption
When does Pepsin gets inactivated?
- When it enters the Intestines
- alkaline pH inactives it
Protein Digestion & Absorption
Further Protein break-down
- Pancreatic Enzymes aid in breakdown
- Ex: Trypsin, Chymotrypsin….
- Proteins are broken down:
- into Peptides
- 1, 2, or 3 amino acids long
- into Peptides
Anorexia, Nausea, Vomiting
Physiologic Responses common to MANY GI Disorders
- Are both:*
- Protective & Destructive*
Anorexia
Loss of Appetite
- Influences:
- Hunger
- Stimulated by empty stomach contractions
- Hunger
- Regulated by:
- Hypothalmus & assc. brain centers
- Smell = plays important role
Anorexia
Factors for Loss of Appetite
- Emotional Factors
- Fear, depression, anxiety…
- Drugs
- Diseases
- Ex: uremia (accumulation of nitrogenous wastes in blood)
Is a “forerunner” of Nausea!
Nausea
- Conscious sensation
- Stimulation of Medullary vomiting center
- Precedes/accompanies vomiting
- Stimulation of Medullary vomiting center
- Stimulants:
- Foods
- Drugs
- Distention of duodenum or upper small intestine
Nausea
Accompanied By:
- ANS Manifestations:
- Watery Salivation & Vasoconstriction
- Pallor, sweating, tachycardia
Retching
- Retching:
- Rhythmic spasmodic movements of diaphargm, chest wall, abdomial muscles
- Precedes/alternates w/ vomiting
Vomiting
- Vomiting:
- Sudden & Forceful oral expulsion of contents of stomach
- preceded by nausea
- Physiologic Protective Mechanism:
- Limits damage of ingested noxious agents by emptying contents of stomach/sm. intestine
Vomiting
2 Medullary Centers
- Vomiting Center
* Reflex, integrated here
* Near sensory nuclei of vagus
- Vomiting Center
- Chemoreceptor Trigger Zone
* Mediates emetic effects of blood-borne drugs & toxins
- Chemoreceptor Trigger Zone
Vomiting
Factoids
- Gastroesophageal Sphinter relaxes
- Respiration ceases
- Accompanied by:
- Dizziness
- Light-headedness
- BP drop
- Bradycardia
Vomiting
Vomiting Center, pt. 1
- Input from
- GI Tract
- Cerebral Cortex
- Vestibular Apparatus
- (motion sickness)
- & Chemoreceptor Trigger zone
Vomiting
Vomiting Center, pt. 2
Causes of N/V:
-
Hypoxia
- periods of: decreased cardiac output, shock, brain ischemia…
-
Intra-abdominal organ inflammation
- b/c stimulates visceral afferent pathways
-
Distention or Irritation of the GI Tract
- b/c stimulates visceral afferent neurons
Vomiting
Neuromediators
- Dopamine
- Serotonin
- Opiod
- Receptors found in GI Tract, vomiting center & chemoreceptor trigger zone
- ACH receptors = Excite vomiting center
- Norepinephrine receptors = stablizing influence resisting motion sickness
Vomiting
Neuromediator Drugs
- Dopamine antagonists = depress vomiting
- Serotonin Antagonists = depress N/V assc. w/ chemo
- Motion sickness drugs = CNS Anti-cholinergic effects
- Act on vomiting center + vestibular system


