physiology of the heart 3 Flashcards
What are the first arteries that stem from the aorta and what is their role
The coronary arteries - These feed the heart muscles.
What is a coronary angiogram?
A small dye is injected into the coronary artery to assess if an individual has coronary heart disease.
What is coronary blood flow
Perfusion pressure / resistance
When does coronary blood flow occur and why?
In diastole - because when the heart contracts it squashes its own blood supply due to the pressure in the heart being so high in systole.
What is the basic metabolism of an arrested heart
2ml/min/100g
What is the metabolism of a resting heart
8ml/min/100g
What is the metabolism of a heart during heavy exercise
70ml/min/100g
How does the metabolism of cardiac myocytes compare to that of skeletal muscle
It is much greater than skeletal
Give the equation for oxygen delivery
Arterial O2 conc x coronary blood flow
What is the result of a patient with coronary heart disease also having anaemia
Anaemia causes reduced O2 delivery - if the patient already suffers from CHD then tissues of the heart may become ischaemic
What is the main target for increasing oxygen making it to the heart muscle?
Coronary blood flow. Not O2 conc as this sees very little change.
Describe the aortic pressure trace
When the heart stops contracting, blood in the aorta attempts to rush back into the left ventricle but is prevented from doing so due to the aortic valve snapping shut. The peak pressure is the systolic pressure and the trough is the diastolic. Coronary blood flow only occurs in diastole so diastolic pressure must have something to do with coronary blood flow.

Describe the left ventricle pressure trace.
To measure a catheter is placed in the left ventricle - The QRS complex is associated with ventricular systole.
Immediately after the heart is activated there is a huge increase in ventricular pressure up to 120mmHg.
When the ventricle relaxes pressure drops to almost zero.
Systolic pressure equates to the peak of the left ventricular pressure
Diastolic pressure equates to LVEDP. The LEVDP is the pressure that stretches the fibres and is important for contraction.
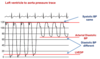
What is the method of performing a left ventricle to aorta pressure trace.
The catheter is put in the left ventricle and then pulled into the aorta - this is a pull-back trace. The systolic BPs are the same, but diastolic pressures are different. The difference between the two is the perfusion pressure
What are the pysical factors effecting diastolic coronary flow
The time interval of diastole and the difference in diastolic pressures of the aorta and LV.
Describe three ways in which the perfusion pressure is decreased.
Reduced aortic diastolic pressure - Reduces the difference between aortic and LVEDP
Raised LVEDP - again reduces the difference
Tachycardia - Disproportionately reduces diastole compared to systole.
Does tachycardia favour changes in systole or diastole
Systole stays te same
The heart rate increases due to a shortening of diastole. It relaxes quicker in order to again fill with blood and perform the next contraction. Some patients become ischaemic because of tachycardia.
What is autoregulation of coronary blood flow
The ability of the heart to maintain a constant blood flow despite changes in perfusion pressure.
How is autoregulation of coronary blood flow performed
The resistance of the vasculature bed is lowered when pressure drops. As a result flow is increased back toward the same level as when pressure initially dropped.
What effect does hypoxia have on coronary arteries
Marked coronary vasodilation in situ but not in isolated coronary arteries.
What is the local metabolite that causes coronary vasodilation during hypoxia, which can be used as a treatment as a result.
Adenosine
What other local metabolites/ mediators cause coronary vasodilation
Increase potassium
Increased carbon dioxide
Increased lactate
Increased hydrogen ions.
What other systems are responsible for autoregulation (not metabolites and mediators)
The autonomic NS and circulating hormones can often effect the coronaries but are much less important.
What hormones are released from the heart and why
Released by stretching of atrial and ventricular muscle cells, raised atrial and ventricular pressures and volume overload
ANP from the atria - Atrial natriuretic peptide
BNP from the ventricles - Brain natriuretic peptide


