Physiology of the heart 1 Flashcards
(30 cards)
What happens during phase 0 of the cardiac cycle
The critical membrane potential is reached, followed by an all or nothing depolarisation. This is caused by a rapid sodium influx
What happens during phase 1 of the cardiac cycle
Partial repolarisation due to rapid sodium influx deactivation
What happens during phase 2 of the cardiac cycle
The plateau phase - due to slow inward calcium current and an initial fall in outward potassium.
What happens in phase 3 of the cardiac cycle
Repolarisation - due to deactivation of inward calcium current, also an increasing outward potassium current
What happens during phase 4 of the cardiac cycle
The pacemaker potential. This has a gradual repolarisation in diastole, it is found in the nodal and conducting tissue. Its driven by increases in the inward sodium/ calcium flow and decreases in the outward potassium flow.
Where is the pacemaker activity present in the cardiac tissue
The atria, which contracts first and then once the impulse has passed through the AV node, it goes through the bundle of His before dividing into the left and right bundles and then to the purkinje fibres. The AV node introduces a delay into the system, allowing the blood to fill the vesicle.
Which cells is the pacemaker activity not present in
Not the atria and ventricles.
What currents are found in the SA and AV node
No rapid Na currents, They’re depolarised by slow calcium currents.
What is the result of increased automaticity
Extra beats, every normal heart can generate these, it creates small waves which are called ventricular ectopics which are due to the heart firing on its own accord.
What is abnormal impulse propogation due to re-entry
Impulses travel along the heart, if they meet a damaged tissue it may act as an insulator or cause abnormal defraction. This may cause earlier tissue that has already finished its refractory period to again depolarise. This is self perpetuating and the arrhythmia may be sustained and lead to tachycardia.
What is the result of a first degree heart block (AV block)
The impulses being blocked are usually at the level of the AV node.
There’s a standard delay of up to 200ms but this can be delayed further.
In frist degree heart block the QRS complex is significantly delayed but every beat is still getting through despite the delay
What does the P wave/ QRS complex represent
P wave = atrial contraction
QRS = ventricular contraction
What does the gap between the P and R wave represent
The delay at the AV node
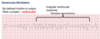
How does 2nd degree heart block present on an ECG
Each P wave has a QRS complex up to a certain point and then there is an ectopic P wave
How does 3rd degree heart block present on an ECG
Complete dissociation between the P wave and the QRS complex. Each goes on its own and the escape rhythm created by the purkinje fibres keeps the person alive.
How are arrhythmias classified?
Firstly from their origin. i.e Sinus, Atrial, Nodal or ventricular
Then the effect on heart rate. Brady or tachycardia.
What is atrial tachycardia
If there are multiple P waves for every QRS complex
What is ventricular tachycardia
A rhythm without a P wave, with a wide QRS complex as it takes longer to propogate. This indicates that the wave does not pass through the normal conductive tissue but originates in the ventricles.

What is atrial fibrilation
No true P wave or atrial rhythm, with an irregular ventricular response. The atria don’t contract, they are just fibrilating. There is no discernable P wave and there is an irregular ventricular response as the AV node allows some impulses through, but some not.

Can a patient survive atrial fibrilation
Yes, however if the atria arent contracting then blood is more likely to clot and create an atrial thrombosis. This may lead to a stroke if the clot breaks off and into circulation.
What is ventricular fibrilation
No defined rhythm or output, wide QRS complex, irregular ventricular response, variable morphology. This is highly life threatening, it leads to cardiac arrest as the cardiac output can’t be sustained. Defibrilators are used to reset the heart rate.
How does the sympathetic nervous system effect heart rate
Increases heart rate (chronotropic effect) through the stimulation of B1 adrenoreceptors.
Increases the slope of the pacemaker potential, increasing automaticity.
How does the parasympathetic nervous system effect heart rate
Reduces heart rate via muscarinic M2 acetylcholine receptors. M2 is mainly found in nodal and atrial tissue.
Decreases the slope of the pacemaker potential, decreasing automaticity and inhibiting atrioventricular conduction.
How are Na channel blockers classified
class 1A/B/C dependent on their rate of dissociation from Na channels (A fast, C slow)


