Pharmocology Flashcards
WHAT IS PHARMOKINETICS?
The action of drugs in the body including/What the body does to a drug
ABSORPTION
DISTRIBUTION
METABOLISM
EXCRETION
What is absorption?
The process of transfer from the site of administration into the general or systemic circulation
What are some routes of administration of drugs?
Enteral (oral)
Enteric-coated (intestinal absorption, e.g. aspirin)
Extended-release (slower absorption, e.g. metformin)
Sublingual/Buccal (rapid absorption + avoids 1stpass metabolism)
Parenteral (systemic circulation)
Intravenous
Intramuscular (anti-psychotics)
Subcutaneous (insulin)
Other
Inhalation(oral, nasal)
Topical
Rectal
How many membranes must most drugs cross? What is the exception to this?
One. IV and IA.
How can transfer through a membrane occur?
Passive diffusion
Facilitated diffusion
Active transport
Endocytosis
What do drugs need to be to pass directly through the cell membrane?
Lipid soluble.
What is the rate of diffusion proportional to?
Rate of diffusion proportional to concentration gradient, the area & permeability of the membrane and inversely proportional to thickness.
What is drug ionisation?
Basic property of weak acids or weak bases.
Why are ionisable groups important for drugs?
The ionic forces are part of the ligand receptor interaction.
What is the PKa of a drug?
pH of which half the substance is ionised and half not.
Where are weak acids absorbed?
Stomach.
Where are weak bases absorbed?
Intestine.
What determines absorption of drugs?
pH
Vascularity (e.g. shock reduces SC absorption)
Surface area
Contact time (e.g. with food = slower gastric emptying)
What are four factors that determine the rate of absorption of an oral drug?
Drug Structure.
Drug formulation.
Gastric emptying.
First pass metabolism.
What do drugs need to be to be absorbed from gut?
Drug needs to be lipid soluble to be absorbed from the gut.
What happens with highly polarised drugs in the gut?
Highly polarised drugs tend to be only partially absorbed with much passed into the faeces.
Some drugs are unstable at low pH or in the presence of digestive enzymes.
What must a tablet be to be absorbed?
The capsule or tablet must disintegrate & dissolve to be absorbed.
Most do so rapidly. Some having coating e.g. Enteric.
What is first pass metabolism?
Concentration of a drug is greatly reduced before it reaches the systemic circulation
What major metabolic barriers do drugs have to cross to reach the circulation?
Intestinal lumen
Intestinal wall
Liver
Lungs
What is contained within the intestinal lumen which limits absorption?
Contains digestive enzymes that can split peptide ,ester & glycosidic bonds.
Peptide drugs broken down by proteases (Insulin).
Colonic bacteria hydrolysis & reduction of drugs.
What is contained within the intestinal wall which limits absorption?
Walls of upper intestine rich in cellular enzymes e.g. Mono amine oxidases (MAO)
Luminal membrane of enterocytes contains efflux transporters such as P-gp which may limit absorption by transporting drug back into the gut lumen
Extensive bowel surgery “short gut syndrome” – poor oral absorption as little surface left and rapid transit time.
How is the liver a metabolic barrier? How can you avoid this barrier?
Blood form gut delivered by splanchnic circulation directly to liver.
Liver is major site of drug metabolism
Avoid hepatic first pass metabolism by giving drug to region of gut not drained by splanchnic e.g mouth or rectum ( GTN )
WHAT IS DISTRUBITION?
Rate & extent of movement of a drug into (and out)of tissues from blood.
What factors control distrubition?
Blood flow (e.g. brain > muscles)
Capillary permeability
Plasma protein binding (e.g. albumin)
Tissue protein binding (e.g. cyclophosphamide accumulating in bladder leading to cystitis)
Lipophilicity(ability to cross cell membranes)
What can some drugs bind to? And what do these act as?
Plasma proteins.
Act as a depot as they release the drug when the blood concentration becomes lower giving a slow release.
What is the half life?
Time taken for a concentration to reduce by half.
In practice the half life is normally for the elimination rate from the plasma as this is easy to measure.
What is bioavailability?
This is the fraction of the administered drug that reaches the systemic circulation unaltered. (F)
IV drugs have F=1 as 100% of drug reaches circulation
Oral drugs may have F< 1 if they are incompletely absorbed or undergo first pass metabolism
What are the factors that control bioavailability?
First Pass Hepatic Metabolism (hepatic transformation of drug to inactive metabolites)
Solubility
Chemical instability (e.g. GI enzyme destruction of insulin)
Why is bioavailability important?
If an oral drug has a score of 0.1 it will need to be 10x the IV dose to be as effective.
Why can’t you measure oral and iv bioavailability at a single point in time?
Different concentration/time profiles.

WHAT IS METABOLISM?
The transformation of the drug molecule into a different molecule.
What happens in metabolism?
Lipid soluble drugs are converted into water soluble ones.
Two phases.
What is first order kinetics?
Catalysed by enzymes, rate of metabolism directly proportional to drug concentration
An exponential fall in the plasma drug concentration
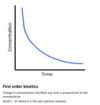
What happens when you plot the log of the concentration in first order kinetics?
Gives a straight line with -k gradient and gives you the concentration at time 0.

What is zero order kinetics?
Enzymes saturated by high drug doses, rate of metabolism is constant, e.g. ethanol, phenytoin
Linear fall in concentration.

What are the steps in metabolism?

What is involved in phase 1 of metabolism?
These reactions involve the transformation of the drug to a more polar metabolite
This is done by unmasking or adding a functional group (e.g – OH, -NH2, -SH)
Oxidations are the commonest reactions catalysed by important enzymes called Cytochrome P450.
What is Cytochrome P450 found?
Smooth endoplasmic reticulum.
Largely in liver tissue.
What increases and decreases P450 metabolism?
Smoking and alcohol increase.
Grapefruit and Cimetidine decrease.
What happens in a phase 2 reaction?
Phase 2 (conjugation)involves the formation of a covalent bond between the drug or its phase 1 metabolite and an endogenous substrate.
The resulting products are usually less active and readily excreted by the kidneys.
Where are some other drugs metabolised?
Plasma, lungs gut.
WHAT IS ELIMINATION?
The removal of a drugs activity from the body.
What is excretion?
The molecule is expelled in liquid, solid or gaseous “waste”.
What does total excretion equal?
Total excretion = glomerular filtration+ tubular secretion-reabsorption.
What does water soluble drugs rate depend on?
Water soluble drugs rate of distribution depends on rate of passage across membranes.
What does lipid soluble drugs rate depend on?
Lipid soluble drugs rate of distribution depends on blood flow to tissues that accumulate drug.
What does Vd stand for?
Vd = total amount of drug in body (dose)/plasma concentration.
The extent of distribution of drug more clinically important as this determines the total amount of drug that has to be administered to produce a particular plasma concentration
This measure is the apparent volume of distribution Vd
What does a low or high apperent volume show?
Low confined to circulatory volume.
High distributed in total body water.
What is clearance?
Clearance ( CL ) is the volume of blood or plasma cleared of drug per unit time.
Eg if 10% of a drug carried to the liver is cleared at flow rate of 1000ml/min the clearance is 100ml/min
If a drug has a high Vd what is the rate proportional to?
If drug has a high Vd it will have a low plasma concentration so the rate of elimination is inversely proportional to Vd.
What is k? What is it equal to?
k is the rate constant of elimination
K= CL/Vd
Previously k =0.693/t1/2
Therefore t1/2 =0.693 Vd/CL
What is the AUC?
Area under the plasma drug concentration versus time curve; a measure of drug exposure.
How is clearance determined?
Clearance is usually determined using the AUC after an iv dose.
CL= Dose/AUC for iv drug
CL= Dose x F/AUC for oral drug with bioavailabilty of less than 1.
What is meant by steady state?
The rate of elimination is the same as drug input.
What does the rate of elimination equal?
Clearance x steady state.
How can an IV steady state be reached?
- With iv infusion it takes approx. 4-5 half lives to reach 95% of Css
- a drug with slow elimination will take a long time to reach steady state and it will accumulate high plasma concentrations before elimination rate rises to match drug infusion
- A high Vd can also lead to a delay in reaching Css as t1/2 is also dependent on Vd ( t1/2 = 0.693Vd/CL )
When is steady state achieved for IV?
For iv infusion, Css is achieved when the rate of elimination equals the rate of infusion
Rate of elimination equals CL x Css so at steady state the rate of infusion also equals this.
So Css = rate of infusion/ CL
or can calculate plasma clearance CL =rate of infusion/Css
What are the properties of oral administration?
- Most long term drug administration is by oral route
- Doses are intermittent so will have peaks and troughs
- Rate of absorption will affect the profile- rapid= exaggerated peaks, slow= flatter peaks
- Correct for bioavailability
D x F/t (t is time interval between doses)
What is the steady state equal to with oral?
- When steady state is reached , the rate of administration is equal to the rate of elimination which is CL x drug concentration between peaks and troughs
- D x F/t = CL x Css
- So Css = D x F/ t x CL
- This means can alter plasma Css by changing either dose ( D) or interval (t )
What is the loading dose and what is it needed for?
- If drug has long t1/2 it will take a long time to reach steady state ( 4-5 half lives) e.g. t1/2 of 24 hours will mean 4-5 days to reach Css
- If give a high initial dose this “loads” the system and shortens the time to steady state
- Loading dose = Css x Vd
- After the loading dose the steady state can be maintained by the maintenance dose given by the equation Css = D x F/ t x CL
WHAT IS THE PERIPHERAL NERVOUS SYSTEM DIVIDED INTO?
Sympathetic and Parasympathetic
What information does the autonomic nervous system convey?
All CNS information except for muscles.
What happens in the somatic nervous system?
One neurone comes from the CNS to innervate one muscle.
What happens in the autonomic nervous system?
Two nerves, pre and post ganglionic fibres.
How long is each parasympathetic and sympathetic fibre?
Parasympathetic long pre ganglionic with short post ganglionic.
Sympathetic short pre ganglionic with long post ganglionic.
What nerves are parasympathetic?
Some cranial nerves and sacral nerves.
What neurotransmitter do post ganglionic fibres release and what receptors do they act on in the parasympathetic system?
Acetylcholine on muscarinic receptors.
What neurotransmitter do post ganglionic fibres release and what receptors do they act on in the sympathetic system?
They release noradrenaline which activates adrenergic receptors, of which there are two main types (alpha/beta) with subtypes.
What parts of the body are only sympathetic control?
Sweat glands and blood vessels.
What parts of the body are only parasympathetic control?
eye and bronchial smooth muscle.
What is the pre ganglionic neurotransmitter for both autonomic systems and what receptor do they act on?
Acetylcholine and nicotinic receptor.
What is released at sweat glands from the sympathetic system?
Acetylcholine on muscarinic receptors.
What are some NANC neurotransmitters?
NO and vasoactive intestinal polypeptide parasympathetic. ATP and neuropeptide Y.
What effect does nicotine have on receptors?
It activates both sympathetic and parasympathetic systems.
What effect does muscarine have on receptors?
Activates the muscarinic receptors on the parasympathetic system.
What are two types of muscarinic receptors?
M1-5, GPCRs.
Where are each of these receptors found? M1. M2. M3. M4/M5.
M1: mainly in the brain.
M2: mainly in the heart. Their activation slows the heart, so we can block these (atropine for life- threatening bradycardias and cardiac arrest)
M3: glandular and smooth muscle. Cause bronchoconstriction, sweating, salivary gland secretion.
M4/5: mainly in the CNS.
What effects does the muscarnic agonist pilocarpine have on the body?
Stimulates salivation.
Activating the sympathetic nervous system. Contracts iris smooth muscle (parasympathetic nervous system).
Side effects would be to slow the heart.
What are some examples of muscarinic antagonists?
Atropine. Hyoscine.
What can Hyoscine be used for?
Antagonise sympathetic driven secretions.
What drugs can you use to treat bronchoconstriction?
Short-acting: ipratropium bromide (atrovent)
Long-acting: LAMAs such as tiotropium, glycopyrrhonium
What else is ACh involved in?
Memory.
What side effects do anti-cholinergic drugs have?
In the brain, anticholinergics worsen memory and may cause confusion Peripherally, may get constipation, drying of the mouth, blurring of the vision, worsening of glaucoma Tricyclic antidepressants, some early antihistamines, some anti-emetics (prochlorperazine).
What side effects do cholinergic drugs have?
Organophosphate insecticides and nerve gases causing poisoning are irreversible acetylcholinesterase inhibitors, and cause muscle paralysis and twitching, salivation, confusion.
What are the catecholamines?
Noradrenaline: released from sympathetic nerve fibre ends, beloved in the management of shock in the intensive care unit.
Adrenaline: released from the adrenal glands (fight and flight, management of anaphylaxis).
Dopamine (the precursor of adrenaline and noradrenaline).
What do each of these receptors do? Alpha 1 Alpha 2 Beta 1 Beta 2 Beta 3
Alpha 1
Contracts smooth muscle (pupil, blood vessels)
Alpha 2
Mixed effects on smooth muscle
Beta 1
Inotropic effects on heart
Beta 2
Relaxes smooth muscle (premature labour, asthma)
Beta 3
Enhances lipolysis, relaxes bladder detrusor
What does alpha 2 receptor do?
Lower blood pressure.