Inflammation, ischaemia, normal and abnormal development Flashcards
What is inflammation?
A reaction to injury or infection involving cells such as neutrophils and macrophages.
When is inflammation good?
Infection or injury.
When is inflammation bad?
Autoimmunity or when an over-reaction to a stimulus.
How is inflammation classified?
Acute and Chronic.
What happens in acute inflammation?
Sudden onset
Short duration
Usually resolves
What are the steps in acute inflammation?
Initial reaction of tissue to injury
Vascular component: dilatation of vessels
Exudative component: vascular leakage of protein-rich fluid
Neutrophil polymorph is the characteristic cell recruited to the tissue
Outcome may be resolution, suppuration (e.g. abscess), organisation, or progression to chronic inflammation
What are the causes of acute inflammation?
Microbial infections, e.g. pyogenic bacteria, viruses
Hypersensitivity reactions, e.g. parasites, tubercle bacilli
Physical agents, e.g. trauma, ionising radiation, heat, cold
Chemicals, e.g. corrosives, acids, alkalis, reducing agents,
Bacterial toxins
Tissue necrosis, e.g. ischaemic infarction
What are the essential characteristics of acute inflammation?
Rubor (red due to blood vessels)
Calor (heat due to blood vessels)
Tumor (swelling due to oedema)
Dolor (Pain due to sweeling and stretching, bradykinin, prostaglandin and serotonin also cause pain)
Loss of function is also characteristic.
What happens in chronic inflammation?
Slow onset or sequel to acute
Long duration
May never resolve
What cells are involved in inflammation?
Neutrophil polymorphs
Macrophages
Lymphocytes
Endothelial cells
Fibroblasts
Plasma cells
What are neutrophil polymorphs and what are their function?
Short lived cells
First on the scene of acute inflammation
Cytoplasmic granules full of enzymes that kill bacteria
Usually die at the scene of inflammation
Release chemicals that attract other inflammatory cells such as macrophages
What are macrophages and what are their fuction?
Long lived cells (weeks to months)
Phagocytic properties
Ingest bacteria and debris
May carry debris away
May present antigen to lymphocytes
What are lymphocytes and what are their function?
Long lived cells (years)
Produce chemicals which attract in other inflammatory cells
Immunological memory for past infections and antigens
What are endothelial cells and what happens to them in inflammation?
Line capillary blood vessels in areas of inflammation
Become sticky in areas of inflammation so inflammatory cells adhere to them
Become porous to allow inflammatory cells to pass into tissues
Grow into areas of damage to form new capillary vessels
What are fibroblasts?
Long lived cells
Form collagen in areas of chronic inflammation and repair
What is an example of acute inflammation?
Acute pancreatitis
Empyema of the gall bladder
Fibrinous pleuricy
What is involved with acute pancreatitis?
Unknown precipitating factor
Neutrophils appear
Blood vessels dilate
Inflammation of serosal surface occurs
Pain felt
Appendix either surgically removed or inflammation resolves or appendix bursts with generalised peritonitis and possible death
What is an example of chronic inflammation?
Tuberculosis
What is involved with tuberculosis?
No initial acute inflammation
Mycobacteria ingested by macrophages
Macrophages often fail to kill the mycobacteria
Lymphocytes appear Macrophages appear Fibrosis occurs
What is the difference between an exudate and a transudate?
Exudates have a high protein content due to increased vascular permeability whilst transudates have a low protein content due to a normal vascular permeability.
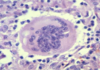
What is a granuloma?
An aggregate of epithelioiod histiocytes and a feature of some-specific chronic inflammatory disorders.
What is granulation tissue?
Granulation is an important component of healing and comprises small blood vessels in a connective matrix with myofibroblasts (A myofibroblast is a cell that is in between a fibroblast and a smooth muscle cell in phenotype)
What are histiocytes?
Specialised macrophages e.g. Kupffer cells
What is fibrin?
Deposited in blood vessels and tissues or on surfaces as a result of the action of thrombin or fibrinogen.
What does fibrous mean?
Describes the texture of non-mineralised tissue of which the principal component is collagen.
What happens in the early stage of acute inflammation?
In the early stages, oedema fluid, fibrin and neutrophil polymorphs accumulate in the extracellular spaces of the damaged tissue.
The presence of the cellular component, the neutrophil polymorph, is essential for a histological diagnosis of acute inflammation.
What are the three processes of acute inflammation? (In relation to vessels and formation of product)
Changes in vessel calibre and, consequently, flow
Increased vascular permeability and formation of the fluid exudate
Formation of the cellular exudate – emigration of the neutrophil polymorphs into the extravascular space.

How is the cellular exudate formed?
The accumulation of neutrophil polymorphs within the extracellular space is the diagnostic histological feature of acute inflammation.
The stages whereby leucocytes reach the tissues are shown in the next figure.

What do the endogenous chemical mediators cause?
Vasodilatation
Emigration of neutrophils
Chemotaxis
Increased vascular permeability
Itching and pain.
What are the plasma factors?
The plasma contains four enzymatic cascade systems:
Complement
The kinins,
The coagulation factors and the
Fibrinolytic system
which are interrelated and produce various inflammatory mediators.

What are the endogenous chemical mediators of the acute inflammatory response?

What causes vascular dilation?
Histamine
Prostaglandins
PGE2/I2
VIP
Nitric oxide
PAF
What causes increased vascular permeability?
Transient phase – histamine
Prolonged phase – mediators such as bradykinin, nitric oxide, C5a, leucotriene B4 and PAF, potentiated by prostaglandins
What causes adhesion of leukocytes?
Interleukins.
What does the outcome of acute inflammation depend on?
The type of tissue present and the amount of tissue destruction which in turn depend on the nature of the injurious agent.
What are the outcomes of inflammation?
Resolution
Suppuration (Suppuration is the process of pus forming)
Organisation
Progression to chronic inflammation
What does suppuration involve?
Excessive exudate.
What is pyrexia?
Raised body temperature.
What are some systemic effects of inflammation?
Pyrexia
Constitutional symptoms
Weight loss
Reactive hyperplasia of the reticuloendothelial system
Haematological changes
Amyloidosis
How can chronic inflammation take place?
Primary chronic inflammation
Transplant rejection
Progression from acute inflammation
Recurrent episodes of acute inflammation
What are the macroscopic appearances of chronic inflammation?
Chronic ulcer
Chronic abscess cavity
Thickening of the wall of a hollow viscus
Granulomatous inflammation
Fibrosis
What are the microscopic appearances of chronic inflammation?
Lymphocytes plasma cells and macrophages.
A few eosinophil polymorphs may be present, but neutrophil polymorphs are scarce.
Some of the macrophages may form multinucleate giant cells.
Exudation of fluid is not a prominent feature, but there may be production of new fibrous tissue from granulation tissue.
There may be evidence of continuing destruction of tissue at the same time as tissue regeneration and repair.
Tissue necrosis may be a prominent feature, especially in granulomatous conditions such as tuberculosis.
What is involved with connective tissue proliferation? How are these processes regulated?
The predominant features in repair are angiogenesis followed by fibroblast proliferation and collagen synthesis resulting in granulation tissue.
These processes are regulated by low molecular weight proteins called growth factors which bind to specific receptors on cell membranes and trigger a series of events culminating in cell proliferation.
What are some examples of chronic inflammation?
Chronic peptic ulcer of the stomach
Gall bladder chronic cholecystitis
How are macrophages involved in chronic inflammation?
Move by amoeboid motion through tissues.
Respond to certain chemotactic stimuli.
Ingest a wider range of materials than polymorphs.
Harbour viable organisms if they are not able to kill them.
In the delayed-type hypersensitivity response, they often die, contributing to the large areas of necrosis by lysozymes.
They are part of the mononuclear phagocyte system (reticuloendothelial system).
What else can a granuloma contain?
lymphocytes and histiocytic giant cells.
What are epithelioid histiocytes?
Named for vague histological resemblance to epithelial cells,
They tend to be arranged in clusters.
Little phagocytic activity, adapted to a secretory function.
One product of the secretory function is angiotensin converting enzyme.
Used as measurement for systemic granulomatous disease, such as sarcoidosis.
What does the association of granulomas with eosinophils show?
A parasitic infection.
What is a common feature of many of the stimuli that induce granulomatous inflammation?
Indigestibility of particulate matter by macrophages.
What is a histiocytic giant cell?
Histiocytic giant cells form where particulate matter that is indigestible by macrophages accumulates.
Histiocytic giant cells form when foreign particles are too large to be ingested by just one macrophage
The multinucleate giant cells develop when two or more macrophages attempt simultaneously to engulf the same particle.
Little phagocytic activity and no known function.
What are the characteristics of Langhans’ giant cells and where are they seen?
Horseshoe arrangement of peripheral nuclei at one pole of the cell. Tuberculosis.

What are the characteristics of foreign body giant cells and where are they seen?
Large cells with nuclei randomly scattered throughout their cytoplasm.
They are characteristically seen in relation to particulate foreign body material.
What are the characteristics of Touton giant cells and where are they seen?
Central ring of nuclei, peripheral to which there is lipid material.
They are seen when macrophages attempt to ingest lipids, and in xanthomas / dermatofibromasof the skin.

How does resolution happen after inflammation?
Initiating factor removed.
Tissue undamaged or able to regenerate.
How does repair happen after inflammation?
Initiating factor still present.
Tissue damaged and unable to regenerate.
What can pneumocytes do very well?
Regenerate.
What are the two different kinds of wound healing?
1st intention and 2nd intention.
How does healing by 1st intention work?
Weak fibrin joint into a strong collagen join.
What happens during 2nd intention?
You get granulation tissue formed.
What are examples of cells that don’t regenerate well?
Myocardial cells
Neurones
What is repair and what are some examples?
Replacement of damaged tissue by fibrous tissue
Collagen produced by fibroblasts examples
Heart after myocardial infarction
Brain after cerebral infarction
Spinal cord after trauma
What is laminar flow?
Normal flow through a capillary.
What disrupts the laminar flow?
Endothelial damage.
What is a thrombosis?
solid mass of blood constituents formed within intact vascular system during life.
What factors contribute to thrombosis?
Change in vessel wall.
Change in blood flow.
Change in blood constituents.
What does aspirin do?
Inhibit platelet aggregation.
What is an embolus?
Mass of material in the vascular system able to become lodged within vessel and block it.
What is ischaemia?
Reduction in blood flow.
What is infraction?
Reduction in blood flow with subsequent death of cells.
When will an infarction become a problem?
When blood supplied to a tissue is an end artery supply.
What is repercussion injury?
Body produces reactive oxygen species after you give the tissue blood back too fast.

What is an example of an end artery?
Kidney. Spleen. Bowel.
What is dual artery supplied?
Lungs. Liver. Brain.
What is the circle of wills for?
Equalise pressure within the brain.
What is a watershed area?
Areas far away from the brain likely to lose blood flow.
What does an aorta look like when people get older?
End up with atherosclerosis plaque.
What are fatty streaks?
Little lines in the aorta in peoples 30s, start of atherosclerosis.
Where do you never find any atherosclerosis?
In pulmonary arteries and low pressure systems.
What is in a plaque?
Fibrous tissue.
Lipids - cholesterol.
(crystals).
Lymphocytes.

What are the risk factors for atherosclerosis?
Smoking.
High blood pressure.
Diabetes.
Hyperlipidaeima.
What is the lipid insudation theory?
Lipid in blood goes into the wall and causes a plaque.
What is the theory for predicting plaques?
Endothelial damage theory.
What damages endothelial cells?
Free radicals. Nicotine. Carbon monoxide.
How does hypertension damage endothelial cells?
Shearing of cells.
How does poorly controlled diabetes damage endothelial cells?
superoxide anions glycosylation products.
How does hyperlipidaemia damage endothelial cells?
Direct damage to endothelial cells.
How does a vessel become occluded?
Thrombus and then endothelial cells form over the top, repeated events like this cause an occlusion.
What are some complication of atherosclerosis?
Cerebral infarction.
Gangrene.
Peripheral vascular disease.
Aortic aneurysms.
What is apoptosis?
Programmed cell death.
How does a cell know to die.
Itself tells itself to die.
Why would a cell undergo apoptosis?
DNA damage.
What are some examples of DNA damage?
Single strand break.
Double strand break.
Base alteration.
Cross linkage.
What is an important part of apoptosis?
p53 gene.
What is apoptosis useful for?
In development, webbed hands and feet, cells in the web apoptose.
In the gut, cells differentiate until the surface then apopotose.
What happens when the cell can no longer apoptose?
Cancer.
In what disease is there too much apoptosis?
HIV in destroying T lymphocytes.
What is necrosis?
Traumatic cell death.
What are some examples of necrosis?
Cerebral infacrtion.
Pancreatitis.
Frostbite.
What are two different types of necrosis?
Coagulative necrosis.
Liquifactive necrosis
What does caseous necrosis mean?
Cheese like appearance.
When do you get the most chromosomal abnormalities?
Before the first month.
Hole in heart?
Left into right ventricle.
What is congenital abnormality?
Present at birth.
What are homeobox genes?
Genes that control development.
What is a acquired abnormality?
caused by non-genetic environmental factors.
What does inherited mean?
caused by an inherited genetic abnormality.
What do Down’s syndrome get more of?
Beta amyloid - dementia. Cataracts.
What is autosomal abnormalities?
Non-sex chromosomes.
What does a pituitary adenoma affect before puberty?
Long bones.
What does a pituitary adenoma affect after puberty?
Skull. Hands. Feet.
What is Amyloidosis?
Build up of amyloid in your body leading to:
Swelling of your ankles and legs
Severe fatigue and weakness
Shortness of breath
Numbness, tingling or pain in your hands or feet, especially pain in your wrist (carpal tunnel syndrome)
Diarrhea, possibly with blood, or constipation
Unintentional, significant weight loss
An enlarged tongue
Skin changes, such as thickening or easy bruising, and purplish patches around the eyes
An irregular heartbeat
Difficulty swallowing


