Peripheral Vascular Disease Flashcards
What is an aneurysm? Is it congenital or acquired? what are the 2 types?
- congenital or acquired
- localized dilation of a blood vessel (aorta) or heart
- types:
- True: involves all 3 layers of wall
- false (pseudoaneurysm): wall defect leading to extravascular hematoma
What are the 3 factors affecting collagen structure or function
- Inadequate or abnormal sythesis of collagen
- Marfan syndrome
- Ehlers Danlos
- Excessive connective tissue degradation
- Occurs with increased matrix metalloproteinase (MMP) or decreased tissue inhibitors of metalloproteinase (TMP) (in the setting of inflammation (atherosclerosis) polymorphisms of MMP and or TMP genes may predispose to aneurysm function)
What is Marfan? What is EHler Danlos syndrome?
- Marfan
- defective synthesis of fibrilin
- fibrilin is “Scaffoliding” for deposition of elastic tissue
- results in cystic medial necrosis of aorta
- leads to aneruysm and arotic dissection
- Ehlers Danlos
- one variant has defective synthesis of Type II collagen
- leads to aneurysm formation
How does smoking influence connective tissue degradation?
smoking influences the balance between MMPs and TMPs
What is the pathogenesis of Aneurysms?
- loss of smooth muscle cells
- thickening of intima (due to atherosclerosis)
- leads to ischemia of inner media
- systemic hypertension
- narrows vasa vasorum, leading to ischemia of outer media
- morphologic result is cyctic medial degradation
- thickening of intima (due to atherosclerosis)
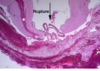
***image shows destruction of the elastic tissue that occurs with an anerysm compared to normal elastc tissue

what are the 2 most common causes of aneurysms? where o these anuerysms occur?
Atherosclerosis-abdominal aorta
Hypertension- ascending aorta
what are some uncommon causes of aneurysm?
- congenital defects
- berry aneurysm: bifurcation of cerebral arteries, subarachnoid hemorrhage
- infections (bacterial, fungi)
- mycotic aneurysm: septic emboli, direct extension, direct infection ny circulating organisms
- syphyllis
- trauma-AV fistula aneurysm
- Vasculitis (inflammation of vessels leads to weakening ot the wall
- IgG4 disease
- Genetic defect in collagen (Marfans and Ehler’s Danlos)
*
What is the most common location of an aneurysm?
Abdominal aortic anerysm (AAA) below the renal arteries and above the bifurcation
arch of the aorta thoracic aorta and iliac arteries also occur but are less common
what is the pathogenesis of an aortic aneurysm(who is it common in and what is the most common cause)?
Describe the morphology (up to X cm etc)
Pathogenesis: more common in men and smokers, most common cause-atherosclerosis
morphology: up to 15 cm diameter.thinning and destruction of media,mural thrombus, saccular or fusiform (one sided or both) variants!
- variants: inflammatory or unkown etiology, mycotic-secondary infection (salmonella gastroenteritis) of an atherosclerotic wall

what is the clinical course of AAA? who is it most common in? how does it present? what are the complications? how do we treat?
more common in men over 50
present as pulsatile abdominal mass
complications
- rupture into peritoneum or retroperitneum
- vascular obstruction-renal, mesenteric, spinal arteries
- embolism of atheroma or mural thrombus to kidenys or lower extremities
aggressive management for large (>5cm) aneurysms, risk of rupture is directly proportional to size
How do we treat?
aggressive management for large (>5cm) aneurysms, risk of rupture is directly proportional to size
open reppair or stent graft inserted through right and left femoral arteries

What are the causes of a thoracic aneurysm? what are the clinical features?
- Causes
- HTN, Marfans syndrome, Tertiary syphyllis
- Clinical Features:
- Mediastinal encroachment
- tracheal compression
- esophageal compression
- bone erosion
- cough due to irritation of the recurrent laryngeal nerve
- cardiac symptoms
- heart failure due to aortic valve insufficiency
- aortic rupture
- Mediastinal encroachment
What is aortic dissection? What is the pathogenesis/etiology?
- blood between and along the laminar planes of media
- causes a blood filled channel that easily ruptures
- pathogenesis/etiology:
- HTN (40-60 yo) >90% of cases
- connective tissue abnormalitiy (younger ages) in association with Marfans syndrom or Ehlers Danlos syndrome
- ascending aorta most commonly involved
- rare causes: post procedural-arterial cannulation; pregnancy
What is the morphology of aortic dissection like? Where does the dissection usualyl occur? inwhat part of the wall?
- initmal tear 10 cm above the arotic valve
- dissetion plane between middle and outer 2/3 of wall in media
- dissection usually extends anterograde
- usually ruptures “out”
- may reenter and form a double barreled lumen
WHat 2 things are associated with an aortic dissection in hypertensive patients?
vasa vasorum: hyaline arteriossclerosis
media: loss of smooth muscle cells
pre-existing pathology of cystic medial degeneration in patients with connective tissue disorder (Marfan syndorme)
How does aortic dissection happen?
Intimal tear begins the process, but trigger for tear is not usually known

what is shown by these pictures?

dissection!
what is this a picture of?

dissection
How does an aortic dissection occur in Marfan Syndrome?
cyctic medial necrosis causes connnective tissue weakness Pools of blue mucinous ground substance disrupt elastic fibers

Describe the clinical course of aortic dissection?
- depenent on level of aorta involved
- sharp pain of anterior chest, uneven pulses and widened meadiastinum
- types A and B
- classical symptoms
- sudden onset of tearing or stabbing pain in anterior chest radiating to the back
what are some possible complications of aortic dissection?
hemopericardium occurs when blood dissects through media proximally
may also rupture into pleural or peritoneal cavities
What is Vasculitis? what 3 things are thought to be involved in the pathogenesis?
inflammation of vessel walls; may affect any size vessel
- pathogenesis:
- immune mediated processes
- infectious origin
- unknown
What immune complex mediated things may lead to vasculitis?
- SLE (systemic Lupus Erythematosis): DNA-nti DNA complexes
- Hypersensitivity to drugs
- Viral infections
- HBsAg-anti HBSAg
How are Anti Neutrophil Cytolasmic Antibodies (ANCA) associated with vasculitis?
- autoantibodies against enzymes in granules of neutrophils
- Ab titiers mirror clinical severity
- two main patterns
- Antiproteinase-3 (PR3-ANCA) granulomatosis with polyangitis (Wegener’s)
- target antigen is PR3 (neutrophil granule constituent)
- Anti-myeloperoxidase (MPO-ANCA)-microscopic polyangitis and CHurg Strauss syndrome
- target is myeloperoxidase
- Antiproteinase-3 (PR3-ANCA) granulomatosis with polyangitis (Wegener’s)









