Pattern Recognition Flashcards
What are the 4 components of a medical image?
Equipment Patient Signal Receptors Signal Processing
Describe equipment as a component of a medical image.
It is dealt with in relation to the patient It relates to: - positioning of equipment - equipment used - MRI specific or surface coils
Describe signal processing as a component of a medical image
It tended to via a computer using specific algorithms Can be chemical in terms of film processing
Describe signal receptors as a component of a medical image
Change between modalities - Transducers - Image recording plate - Film / Screen combination - Radioreceiver - PMTs
Describe the patient as a component of a medical image
Need to understand the anatomy and physiology Positioning of the patient
What needs to be understood to interpret an image?
- Interaction of the source with various tissue types - Affect of beam geometry - Affect of patient position on structures - Anatomical structures (localisation, physiology and manifestation of disease)
What is the effect of beam divergence? How is it reduced?
Image magnification Gives a geometric unsharpness Reduce by placing the recording medium as close to the object
Why is a chest X-ray taken PA?
Allows for assessment of heart size It reduces unsharpness and magnification It reduces the effect of breast tissue If AP then the scapula can be projected into the lung field
How is a chest X-ray taken?
PA (posterio-anteriorly) Remove the scapula out of the image view
How does shade and colour alter perception of images?
Shade helps to identify structures The mind fills the gap to create the perception of depth 10% of colour interpretation is governed by context not wavelength
What are the problems associated with radiography?
3D representation in a 2D image Summation of shadows Standardisation in positioning is vital to identify positioning and location
What is the benefit of standardisation of positioning?
Allows you to identify the position and the location You become familiar with the orientation - familiar frame of reference
How are hands X-rays usually acquired?
Dorsi-palmar Need to label right and left
What is a reason for altering from a standard projection?
Makes it more comfortable for the patient If the patient is less likely to move
What are the 4 different types of contrast?
Subject Recording medium/system - Image Objective Subjective
What is the difference between subject and image contrast?
Subject contrast is the differences between X-ray intensities emerging from the patient Image contrast is the differences recorded in the radiographic image
What is the difference between subjective and objective contrast?
Subjective - dependent on the eye of the observer, varies from person to person Objective - actual differences in densities or black and white
How can subject contrast be changed?
Altering differences in attenuation using contrast agent - Barium, iodide, gadolinium
What are examples of contrast agent?
Barium Iodide Gadolinium
What are examples of contrast agent?
Barium Iodide Gadolinium
Why is it important to get the patient, X-ray detector and beam source parallel?
Need to get a truly representative image Otherwise can get: foreshortening or elongation
What is foreshortening in an X-ray image?
The image appears squashed Happens when the patient leans forward
What is elongation in an X-ray image?
If the detector is angled you get a stretched/elongated image Can be used advantageously in the scaphoid
Where can beam geometry be applied usefully?
- PA chest radiography - Sacroiliac joints demonstration - Aid to identifying patient positioning
What are the identification points when assessing a radiographic image?
- Check patient ID - Time & date of examination - Check correct anatomical markers and appropriate legends - Facility name
What are the identification points when assessing a radiographic image?
- Check patient ID - Time & date of examination - Check correct anatomical markers and appropriate legends - Facility name
What anatomical features do you need to check when assessing a radiographic image?
- Check all relevant anatomy is included in the projection - Are all anatomical features accurately displayed? - Sharp definition of all cortical outlines and/or soft tissue - Protocols (differ between facilities) - Trace bony outline (disruption = pathology) - Compare both sides and projections
What are the points to check in terms of image quality in a radiographic image?
- Is there adequate contrast and density displayed? - Is there adequate penetration? - Is there any signs of unsharpness? - Is there any evidence of collimation? - Are there any artefacts present?
What is the sign that indicates adequate penetration in a chest X-ray?
Should be able to see the 4 thoracic vertebrae through the heart. If this is not visible, could be pathology or inadequate exposure.
What are the categories for artefacts?
Anatomical e.g. hair External e.g. clothing, pins, hearing aids Internal e.g. swallowed items Equipment/imaging related e.g. dust
What are the problems with X-ray interpretation that can lead to misdiagnosis?
Overlapping structures Projecting what you expect to see onto the image (e.g. if the patient is in pain, a soft tissue line can be viewed as a fracture)
What are the requirements for interpretation of an image?
- Understand what is in the image - Understand what is in the patient - Understand what was conducted - Be aware of the limitations of the procedure
What are the requirements for interpretation of an image?
- Understand what is in the image - Understand what is in the patient - Understand what was conducted - Be aware of the limitations of the procedure
What is pattern recognition?
It is an information reduction process. The assignment of visual logical patterns to classes based on features of these patterns and their relationship
What is clinical judgement?
It is the interpretation of X, being a real example of Y or support the conclusion reached
What is clinical judgement?
It is the interpretation of X, being a real example of Y or support the conclusion reached
What is the function of an X-ray examination?
- Accurate localisation of fracture and determination of number of fragments - Indicate the degree and direction of displacement - Provide evidence of pre-existing disease - May demonstrate a foreign body - May show indication of nature of injury (This can be linked to any imaging modality)
What are the limitations of an X-ray examination?
- Contrast resolution 2. Spatial resolution 3. Sensitivity of the system - Need 30-50% bone loss to detect osteoporosis
What modalities can be used to detect osteoporosis?
- X-ray (poor) due to low sensitivity - DEXA - Radionuclide (very sensitive but not specific)
What are the points on a checklist for reviewing diagnostic image appearances?
- Size and shape of structure - Position of structures - Thickness of structures - Mineralisation - Trabeculation of cancellous bone - Vascular patterns - Contour of structure (smooth/sharp) - Look for symmetry - Joint space, size, shape, normal? - Alignment/articulation - Soft tissue assessment - Changes with development - Correct numbers of bones - Relationship with other structures
What are the points on a checklist for reviewing diagnostic image appearances?
- Size and shape of structure - Position of structures - Thickness of structures - Mineralisation - Trabeculation of cancellous bone - Vascular patterns - Contour of structure (smooth/sharp) - Look for symmetry - Joint space, size, shape, normal? - Alignment/articulation - Soft tissue assessment - Changes with development - Correct numbers of bones - Relationship with other structures
What are the starting points to interpreting an image?
- Examine general appearance of the bone - Trace the contour of each bone for irregularities - Examine joint space - Examine soft tissue (can provide indirect evidence of a fracture)
Why is it important to examine soft tissue in an X-ray?
Can provide indirect evidence of a fracture.
Why is it important to examine soft tissue in an X-ray?
Can provide indirect evidence of a fracture.
What are the 2 ossification centres and what are they responsible for?
Primary - controls width of bone Secondary - controls the length of bone
What is an additive disease?
Abnormal condition leading to an increase in fluid or bone. Fluid has the effect of distending tissue, which increases the thickness.
What are the results of having an additive disease?
- Bone has a higher than average atomic number (compared to normal bone) - Excessive bone growth or the replacement of cartilaginous tissue with bone - Increase n the amount of calcium present in the bone - Bone becomes denser in structure - Bone is more radio-opaque - Can be focal or general
What are the most common additive disease?
- Acromegaly - Paget’s disease - Osteoarthritis - Osteochondroma - Osteopetrosis
What is a destructive disease?
Abnormal condition leading to an increase in air or fat OR a decrease in normal body fluid or bone
What are the results of having a destructive disease?
- Demineralisation of bone or an invasive destruction of bone tissue - Decrease in the amount of calcium in the bone - Bone becomes less dense in structure - Bone more radiolucent - Can be general or focal
What are the common destructive diseases?
- Osteoporosis - Rheumatoid arthritis - Osteomalacia - Exostosis - Osteomyelitis - Gout - Hyperparathyroidism - Ewings tumour
What are the 3 types of bone abnormalities?
- Opacity - increased radiographic density e..g overlapping bone fragments 2. Radiolucency - decreased radiographic density e.g. fracture line 3. Distortion/displacement of normal structures e.g. - Bump/step/gap in cortex - buckle or bowing - collapse (vertebrae) - subluxation/dislocation - soft tissue swelling
What are the 3 types of bone abnormalities?
- Opacity - increased radiographic density e..g overlapping bone fragments 2. Radiolucency - decreased radiographic density e.g. fracture line 3. Distortion/displacement of normal structures e.g. - Bump/step/gap in cortex - buckle or bowing - collapse (vertebrae) - subluxation/dislocation - soft tissue swelling
What is a Jones/avulsion fracture?
Tendon pulls off part of the bone it is attached to
What is a Jones/avulsion fracture?
Tendon pulls off part of the bone it is attached to
What are the points to note on a pelvis X-ray?
- Sacro-iliac joints should be equal in width 2. Sacral foramina should not be disrupted 3. Superior surface of the symphysis pubis should be aligned (should be approx 5mm) 4. Acetabular regions should be compared for variation
What does a widening in the sacro-iliac joint represent?
Fracture of the main ring
What is the usual distance between the superior surface of the symphysis pubis?
5mm
What are the 2 rings of the pelvis?
- Main pelvic ring 2. 2 Smaller rings formed from pubic and ischial bones
What are the frequent pelvic fractures?
Acetabular Sacral Coccygeal
What should be checked when looking at an X-ray of the cervical spine?
- Lines should be smooth and unbroken - Check vertebral alignment: - Along the anterior margins of vertebral bodies - Along the posterior margins of vertebral bodies - Along anterior bases of spinous processes (may be slight step at C2) - Vertebral bodies below C2 have a uniform, oblong shape - Intervertebral discs should be of equal height - The relationship between the anterior aspect of the odontoid peg and posterior aspect of the anterior arch of C1 should be no more than 3mm in adults and 5mm in children
What should be checked when looking at an X-ray of the cervical spine?
- Lines should be smooth and unbroken - Check vertebral alignment: - Along the anterior margins of vertebral bodies - Along the posterior margins of vertebral bodies - Along anterior bases of spinous processes (may be slight step at C2) - Vertebral bodies below C2 have a uniform, oblong shape - Intervertebral discs should be of equal height - The relationship between the anterior aspect of the odontoid peg and posterior aspect of the anterior arch of C1 should be no more than 3mm in adults and 5mm in children - Spinous process should be in a straight line - Distances between spinous processes should be equal - Atlanto-axial distance approximately equal distance - Lateral margins of C1 should align with lateral margins of C2
Describe the normal relationship between C1 and the odontoid peg.
The anterior aspect of the odontoid peg and posterior aspect of the anterior arch of C1 should be no more than 3mm in adults and 5mm in children Peg = 1/3 Space = 1/3 Cord = 1/3 Lateral margins of C1 should align with lateral margins of C2
Describe the soft tissue in the cervical spine
C1-C4 7mm approximately 30% of the vertebral body C5-C7 22mm approximately 100% of the vertebral body
Describe the soft tissue in the cervical spine
C1-C4 7mm approximately 30% of the vertebral body C5-C7 22mm approximately 100% of the vertebral body
What are the 5 lines to consider when assessing facial bones?
- Superior orbital margin - Inferior orbital margin - Inferior zygomatic - Superior mandibular - Inferior mandibular

What are the rules for trauma imaging?
- 2 views or possibly more required - Joints above and below the fracture must be visualised in case they may be involved - Ensure to continue the search even if a fracture is noted - When no fracture is noted, note any changes to the joint - Look for indirect evidence of fractures such as displacement of fat pads - Examine for a foreign body
If a decision cannot be made about a diagnosis based on an image, what should be done?
- Postpone the decision - Get more information - Get further views - Ask a colleague - Use a reference
How can you tell if a chest x-ray is foreshortened?
The clavicles appear higher than normal
It alters the shape of the mediastinum
It changes the shapes of the ribs
What condition is shown here?

Osteochondroma
What condition is shown here?
What are the notable features?

Paget’s disease
Thickened trabecular and cortical bone
The bone is weaker and as a result of it being a weight bearing bone, it bends.
It doesn’t affect the fibular
What condition is shown here?
What are the notable features?

Osteoarthritis
- Reduced Joint space due to erosion of cartilage
- Joint area more radio-opaque due to bodies protective mechanism (laying down extra bone to protect the joint)
- Can have (but not present) bony outgrowths/osteophytes
What condition is shown here?
What features can be noted?

Rheumatoid arthritis
Z deformity in the thumb
Swan neck deformity in the little finger
Carpal bones, loss of joint spaces / decrease bone density
What pathology can be seen here?

Radial head fracture
What pathology can be seen here?
What are the notable features?

Fractured Neck of Femur
The left leg is shorter than the left due to the raised greater trochanter
The leg is externally rotated as you can see more of the lesser trochanter
What pathology can be seen here?
What are the notable features?

Osteoporosis - vertebral collapse
The bone is thinner resulting in less attenuation of the Xray beam
Only the trabecular bone is degraded so the framing occurs as the cortical bone remains - this gives low contrast
What sign is apparent in this image?

Sail sign
It is a soft tissue sign. Due to the increased pressure within the joint, the fat pad is elevated.
It is indicative of a radial head fracture
What can be seen in this image?

Bipartite patella - this is a normal variation
What can be seen in the image?

Multiple pelvic fractures - the likelihood of multiple fractures is increased due to the circular shape
What pathology can be seen here?

Facial fracture
It can be identified as one of the sinuses has filled with blood, indicating a fracture.
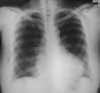
What are the 7 stages to Chest X-ray interpretation?
- Acceptability of the radiograph
- Diaphragm, heart and mediastinum
- Lung edges
- Lung fields and posterior ribs
- Anterior ribs & shoulder girdles
- Neck and soft tissue
- Assess for any tubes/wires/catheters
What should be checked to make sure a chest radiograph is suitable for use?
- Patient ID
- Date of examination
- Markers
- Patient position (standard projection, is the patient erect)
- Medial clavicles shoud be equidistant from the spinous processes
- Scapula should be free from the lung field
- Sufficient phase of respiration (count ribs)
- Adequate penetration
How do you assess for adequate penetration in a chest X-ray?
Should be able to see down to T4 spinous process
Beam should have enough power to display all features
Need to be able to see behind the heart - if not could be a hidden pathology
What is the normal number of ribs seen in a X-ray when erect?
8-11
What is the normal number of ribs seen in a X-ray when seated?
7-9
In a chest X-ray what must be assessed in terms of technical quality of the image?
Projection
Orientation
Rotation
Penetration
Degree of inspiration
CXR: What needs to be assessed in stage 2?
Diaphragm, heart and mediastinum
Trace around and assess:
- heart size and shape
- mediastinum
- hilar vessels
- fissures
- shape of aortic knuckle
- Free gas
CXR: Where should you look most closely for free gas?
Right hemidiaphragm
Under the pericardium
CXR: How would aortic stenosis present?
Increased size in the left ventricle - the heart has to work harder against the resistance of the stenosis
Can cause increase in the size of the ascending aorta and the aortic arch - depends on where the stenosis is
CXR: How would mitral disease present?
Increase in the size of the left atrium
Deviated pulmonary trunk
In later stages, the left and right atria can enlarge in addition to a larger left ventricle. Pulmonary trunk enlargement.
CXR: How do you check the mediastinum?
Check the shape - is it normal?
Check the edge outline - it should be clear
Some fuzziness is acceptable:
- at the angles between the heart and diaphragm
- apices
- right hilum
CXR: What does fuzziness in the edge of the mediastinum indicate?
It could be normal (in expected places)
Can indicate collapse or consolidation
CXR: In a normal image how do the hilar appear?
Left should be higher than the right
Difference between them should be less than 2.5cm
Should be concave in appearance
Should have similar densities and shapes
CXR: In a normal image how does the trachea appear?
Should be central
Slight deviation to the right at the aortic knuckle
A shift is indicative of mediastinal problems
Spinous processes should be in the centre of the trachea
The white edge on the right should be no larger than 2-3mm on an erect film
Right main bronchus is wider and steeper than the left
CXR: How would a right upper lobe collapse appear?
Change in aeration of the right upper lobe - becomes more radio-opaque (whiter)
Trachea pulled slightly to the right
Displacement of horizontal fissure
Hilum displaced
No change in heart border
Minor fissure deflected upwards
CXR: How would a major right upper lobe collapse appear?
Right upper lobe is a flat wedge of opacity
Trachea deviated to the right
Aortic arch is tilted to the right
Upper lobe opacity is against the superior mediastinum
Right hilum is drawn upwards
Compensatory overaeration in lower lobes (more radio-lucent)
CXR: What is the normal appearance of the diaphragm?
Right is higher than the left
Difference should be less than 3mm
Outline should be smooth
The highest point of the right diaphragm should be in the centre of the right lung field
Highest point on the left is slightly more lateral
CXR: What is the normal appearance of the costophrenic angles?
Well defined
Acute angles
CXR: What are the early signs of a left lower lobe collapse?
Less heart shadow to the right of the spine
Vague decrease in lucency of the lower left lobe
Preservation of the left hemidiaphragm (slightly elevated medially)
Displacement of the hilum
CXR: What are the signs of a major left lower lobe collapse?
Little or no heart shadow at the right of the spine
Medial half of the border fo the left diaphragm is missing
Left lower lobe is a wedge of opacity
Left hilum is depressed
Medial hemidiaphragm is obscured
Upper lobes overaerated
CXR: What are the mediastinal lines and stripes that are visible?
Anterior pleural junction line
Posterior pleural junction line
Right paratracheal stripe
Left paratracheal stripe
Aortopulmonary window
Para-aortic stripe
Azygoesophageal stripe
Paravertebral/paraspinal stripe
CXR: Describe the anterior pleural junction line
It is a result of parietal and visceral pleura meeting anteromedially
Seen on 40% of frontal chest X-rays
CXR: Describe the posterior pleural junction line
Formed by the opposition of pleural surfaces of posteromedial surfaced of upper lobe of lungs
Posterior to the oesophagus
Anterior to T3-T5
Seen on 32% of PA chest X-rays
CXR: Describe the right paratracheal stripe
Normal on a frontal chest X-ray
Represents right tracheal wall, adjacent pleural surfaces and any mediastinal fat
Measures less than 4mm (widens in disease)
Appears radio-opaque
Lungs and pleura wrap around trachea
Seen in 97%
CXR: Describe the left paratracheal stripe
Formed by the interface of medial pleura surface of the left upper lobe and the left lateral border of trachea.
Less common to see due to aorta/subclavian/common carotid
Seen in 20-30% of PA chest X-rays
CXR: Describe the aortopulmonary window
Lies between the aorta and pulmonary vessels
Look to see if the window is obscured
Can be obscured by lymph vessels
CXR: Describe the para-aortic stripe
Line that follows the aorta down
CXR: Describe the azygoesophageal stripe
Indicates the border of the pleura and fllows the oesophagus and azygous vein
CXR: Describe the paravertebral line
Refelection of the lungs around the vertebrae
Only see if there is a pathology - haematoma, osteophytes
RIGHT –> interface of right lung and posterior mediastinal soft tissue (25% of frontal chest Xray)
LEFT –> left lung and left posterior mediastinal tissue, appears darker due to the heart shadow (35% of frontal chest X-rays)
CXR: What should be assessed in step 3?
Lung edges
Look for evidence of effusion or pneumothorax
Look for evidence of thickening of tagging of the pleura
Don’t forget to check behind the heart
CXR: What features demonstrate effusion?
Blunting of the costo and cario-phrenic angles
CXR: Descibe the hilar vascular markings
Hilar vascular markings are smaller in the top half of the X-ray field - this is due to gravity
When the lung field is divided into thirds vertically:
The 1/3 closest to the midline - vascular markings are prominent
The middle 1/3 - vascular markings are visible but are less prominent
The outer 1/3 - vascular markings are fine and difficult to visualise
CXR: What should be assessed in stage 4?
- Compare the right and left lung fields for similar densities
- Compare zones on both sides
- Compare vascular markings to surrounding features
- Any changes in radio-opacity?
- Check for lung tissue behind the heart
- Count posterior ribs (DON’T MISS 1ST RIB)
- Note the hilar shadows
CXR: Normally how many posterior ribs should be visible?
9-10
Can vary on each side
Don’t omit the first rib
CXR: What are the lobes and fissures that can be seen?
Oblique or major fissure
Minor fissure
Azygous lobe fissure
Azygous lobe (NV)
Superior accessory fissure (NV)
Inferior accessory fissure (NV)
(NV) - normal variant
Which lung is visible in this image? Why?

Right
The right diaphragm is higher and is continuous from anterior to posterior and extends all the way from the sternum
The right major fissure has union with the minor
CXR: Which lung is visible in this image?

The left diaphragm is lower and it extends to the heart shadow.
Major fissures merge with the ipsilateral diaphragm.
Describe the left minor fissure of the lung
It only occurs in 8% of people but can only be seen in 1.6% of chest x-rays
It separates the lingula from the rest of the left upper lobe
Often resembles the right minor fissure
CXR: What is the companion shadow of the 2nd rib?
It is a dark shadow in the apical region approximately 2mm in width at the interior border of the 2nd rib
CXR: What should be assessed in stage 5?
Check the bony skeleton of the anterior ribs and shoulder girdle
- Look for changes in density, compare side to side
- Look for fractures and changes in shape
- Any erosions
CXR: What should be assessed in stage 6?
Neck and soft tissues
- Start at the neck and note any bony cervical abnormalities
- Follow line around soft tissue (through axillary region and over the breast)
- Look for evidence of surgery
- Look for air in soft tissue
- Consider skin folds in larger patients
- Consider posterior and anterior axillary folds
- Breast tissue
- Can see the sternocleidomastoid on thinner patients
- Can sometimes see nipples due to different densities
CXR: What should be assessed in stage 7?
Check for wires, catheters and foreign bodies
What should be assessed along these 3 lines?

- Look for name, date and anatomical markers, consider the apical sections
- Check for rotation. See if the lungs are of similar densities. Are they of equal size? Is the trachea central? Is it adequately exposed?
- Assess the lung bases. Adequate inspiration (9-10 ribs)
CXR: What are the risky areas that need to be checked twice? Why?
Pulmonary apices
Hila
Retrocardiac areas
Costophrenic angles
Lesions hide here!
What is a tension pneumothorax and how does it present on a CXR?
Opening acts as a one way value
Results in an increase in intrathoracic pressure with each breath
Mediastinal shift away from the affected side
Ipsilateral depression of the hemidiaphragm
Mediastinal compression compromises venous return
Black shadow
What is pleural effusion and how does it present on a CXR?
Depressed diaphragm
Can contain air or fluid
Massive collection can displace the mediastinum
Look for upward curve against the lateral chest wall
Get a fluid level appearance
CXR: What do you need to look for in lung collapse?
Movement of the horizontal fissure
Deviation of the trachea
Raised diaphragm (dependent on which lobe)
Variation in radiodensity
Overaeration of affected side to compensate
How does consolidation appear on a chest x ray?
Appears white
Obliterates mediastinal line
Lung becomes airless
Similar in density to soft tissue
Loss of diaphragm
CXR: How would consolidation of the left lower lobe appear?
Lose the diaphragmatic border
Keep the left heart border
CXR: How would consolidation of the left upper lobe appear?
Lost the left heart border
Keep diaphragmatic border
What pathology is visible?

Teratoma metastases
What pathology is visible?

Left pneumothorax
What pathology is visible?

Pleural effusion
What pathology is visible?

Calcified trachea and bronchi
What pathology is visible?

Fractured ribs and hydropneumothorax
What pathology is visible?

Lung abscess
What pathology is visible?

Acute TB with cavities query
What pathology is visible?

Sarcoidosis Progressive granulomatous recticulosis of unknown etiology.
Invloves almost any organ. Characterised by non-caseating (caseation – tissue changed into a dry amorphous mass resembling cheese) epitheliod cell tubercules.
What pathology is visible?

Polycystic lung disease with fluid levels
What pathology is visible?

Right upper lobe collapse
What pathology is visible?

Lesion in the right upper lobe
What pathology is visible?

Consolidation of the right base
Filling of air passages with exudate
What pathology is visible?

Infection in the right lower lobe
What pathology is visible?

Pleural effusion in right lung
Fluid level - indicates effusion rather than consolidation
What pathology is visible?

Pleural effusion right lung
Lateral view
What pathology is visible?

Left sided mass
What pathology is visible?

Metastases
What pathology is visible?

Emphysema with possible effusion
What pathology is visible?

pneumoconiosis
What pathology is visible?

Pulmonary calcification
Query old TB
What pathology is visible?

Cardiomegaly
What pathology is visible?

Consolidation of lung bases
What pathology is visible?

Old TB - calcified deposits
What pathology is visible?
Cardiomegaly
Increase in left ventricle size, possible increase in right atrium size, and left atrium.
Consider mitral disease
What pathology is visible?

Free air under right diaphragm
What pathology is visible?
Right pleural effusion
What pathology is visible?

Opacification of the right lower lobe
What pathology is visible?

Congestive heart failure
What pathology is visible?

Diffuse opacities
Fibrosing alveolitis
What are the 3 main scan planes used in ultrasound?
Longitudinal/saggital
Transverse
Coronal
Describe the orientation seen on a longitudinal US scan?
Top = skin
Right = Feet
Bottom = Back
Left = Head
Describe the orientation seen on a transverse US scan?
Top = Skin
Right = Patient’s left
Bottom = Back
Left = Patient’s right
How does fluid appear on an US scan?
Appears black
Clear fluid should contain no echoes
Some post-cystic enhancement behind the fluid
If it has any internal echoes - suggestive of a thicker fluid
How does a solid mass appear on an US scan?
Usually well defined
Full of echoes
Mostly echogenic
Can observe posterior shadowing
How does air/gas appear on an US scan?
Air/gas reflects US
Can obscure the object you are trying to view
Appears very bright
Ususally see linear echoes
How do arteries appear in US?
Arteries should be pulsatile and have echogenic walls
How do veins appear in US?
Veins should be non-pulsatile
Thin walls
Should collapse on respiration/val-salva and compression
US: What are the components of patient safety to be considered?
No harmful effects
Ensure the examinations are appropriate and necessary
Always keep the US power as low as reasonably practicable
Don’t leave the transducer on the patient unless acquiring an image
Keep scanning time to a minimum
US: Why is it necessary to use coupling gel?
Essential to obtain the image
Eliminates the air interface to allow US transmission into the body
Need to use sufficient for the transducer to glide smoothly
Too much makes it harder to get
US: What are the effects of having the gain set too high?
Image is too bright
US: What are the effects of having the gain set too low?
Image is too dark
US: What is the procedure for setting the depth of the ROI?
Start scanning with the depth set to allow a full view of all major organs
Adjust the depth according to the depth of the ROI
Need to make the ROI as large as possible without losing information off the bottom of the screen
If the depth is not correctly set up, landmarks will be difficult to assess
US: How is the focus area indicated and changed?
Indicated by a small arrow at the side of the image
Can be moved up or down using the focus control
US: What is the effect of increasing the amount of focal zones?
Increases resolution
Lowers the frame rate
US: When is it better to use only one focal zone?
Better for moving objects e.g. aorta
US: When is it better to use multiple focal zones?
Good for non-mobile superficial objects e.g. testes
US: What is the benefit of narrowing sector width?
Improves the image
Need to not exclude any of the ROI
Good for looking at the gall bladder and transverse aorta
US: What are the 4 movements possible with the probe?
Sliding
Rotating
Angling
Dipping/rocking
US: Describe the probe movement of rotation
Rotation of the probe around a fixed point.
Switching between LS and TS while keeping an organ in view
US: Describe the probe movement of angling
Alteration of the angle of the probe in relation to the skin
US: Describe the probe movement of dipping/rocking
Describes gently pusing one end of the probe into the abdoment
US: What are the steps for setting up the equipment?
- Power on
- Enter patient details
- Annotate the images
- Select the probe
- Select the preset
- Orientate the scan
- Select transmit frequency
- Set overall gain
- Set time gain control
- Set focus
- Set depth/magnification/FOV
US: How do you decide how to select the transmit frequency?
Always use the highest frequency that would provide adequate penetration
This increases spatial resolution
US: What is the overall gain?
Controls the amount of amplification fiven to all returning echoes regardless of depth
Should be set so soft tissue is mid-grey and fluid is black
US: What is time gain control?
It corresponds to specific depths within the patient and is used to compensate for increased attenuation with depth.
Need to get similiar structures to appear at the same brightness at all depths
US: What is the effect of changing the focus to the depth of the ROI?
It increases lateral resolution
US: What happens to the frame rate as the field of view is decreased?
Increased frame rate
What position is this image taken in? Why?

The barium is raised at the top of the stomach.
The patient is either lateral or supine.
What position is this image taken in? Why?

Patient is prone.
The air is at the top of the stomach with the barium collected at the bottom.
What position is this patient in?

Supine
What position is this patient is in?

Prone
What position is this patient in?

Patient is prone
The barium is the transverse colon with air in the ascending and descending colon
What position is this patient in?

Supine
The air is in the transverse colon.
The barium has collected in the ascending and descending colon
US: What is the examination technique for upper abdominal US?
- Need to fast for 6 hours before to assess biliary tree
- Variable patient positions required
- Start supine but can do erect, lateral, right and left anterior oblique
- Minimum of 2 scan planes
- Curvilinear transabdominal between 3-7MHz
US: On a longitudinal scan, what is in each direction?
Top: skin
Right: feet
Left: head
Bottom: back
US: Describe how veins appear?
No bright walls
Walls are indistinct
All collapse on inhalation
US: How does the portal system appear?
Bright walls
US: What is the normal liver appearance?
Homogeneous mid grey echo texture
Interrupted by vessels and ligaments
Echogenic thin capsule around the liver
Similar or slightly increased echogenicity when compared to the cortex of the right kidney
Ligaments appear as echogenic linear structures
US: What is the portal triad and how does it appear?
Portal vein
Hepatic artery
Bile duct
Double barrelled/ parallel doube channel only seen when dilated
US: Why does the diaphragm appear bright?
It is curved
It focuses the US and therefore it appears bright
US: What are the 3 veins visible on a transverse section entering the IVC?
Right, left and middle hepatic vein
US: What direction should the blood travel in the portan vein and what colour would appear in Doppler?
It should travel towards the liver
It should appear red
US: What are the consequences of portal hypertension?
Increased diameter of vessels
Collaterals develop
Reversed flow in the portal system
Can get splenic varices or collaterals
US: In a longitudinal view of the kidney, where is the upper pole?
It is located at the bottom
US: How do you distinguish between the aorta and IVC?
Aorta walls are brighter than the IVC
Normal views of the IVC do not have branches
US: What are the liver pathologies that can be seen using US?
Haemangioma
Cirrhosis
Hepatocellular carcinoma (HCC)
Metastases
US: How does a haemangioma appear?
Extremely echogenic
well circumscribed lesions
Appear very bright
US: How does cirrhosis appear?
May appear normal
Fat and fibrosis is hyperechoic
There are textural changes - coarse and nodular
Has a lobulated outline
Asymmetrical hypertrophy/atrophy
Haemodynamic changes e.g. portal hypertension and splenomegaly
Ascites and HCC
Image gets increasingly brighter over time and will see less of the liver
Caudate lobe often spared so can look larger
US: How does a liver metastasis appear and where does it most likely come from?
May be solitary or multiple, appearance depends on primary
Likely to be from the bowel or breast
US: How does the common bile duct appear?
Intrahepatic portion is demonstrated anteriorly and to the right of the portal vein
Extraheptaic is harder to view and is often overshadowed by bowel
Normal calibre = 6mm
More ectactic in elderly = 8-9mm due to degeneration of the elastic fibre wall
What colour does the portal vein appear on Doppler?
Red
US: How would you see a stone in the common bile duct?
Often hard to see
Use long oblique view to see the neck of the gall bladder
Can sometimes just see the anterior surface as it is a strong reflector
US: What is the normal appearance of the gall bladder?
Variable positions, size and shape
Distended
anechoic
pear shaped sac
echogenic thin walls
Can sometimes be absent or previous cholecystectomy
US: What are the potential gall bladder pathologies that can be visualised?
Choleithiasis (gall stones)
Cholecystitis (inflammation)
Polyps
Adenomyomatosis
Carcinoma
US: How do gallstones appear?
Calculi appears echogenic with posterior acoustic shadowing
Postcystic enhancement due to decreased attenuation as it passes through fluid
Usually mobile - move patient to clarify
US: What is the normal gall bladder wall thickness? How is measured?
Less than 3mm when fasting
Measure the anterior wall in the transverse or longitudinal section
Use the anterior wall as it is difficult to delineate the posterior wall from the stomach
US: What are the signs of acute cholecystitis?
Thickening of the gall bladder wall
Gallbladder tenderness
Gall bladder enlargement
Pericholecystic fluid
Gas in GB
Acalculus in 5-10% of patients
US: What are the signs of chronic cholecystitis?
Can’t distinguish between acute and chronic with US
Recurrent RUQ pain
Almost always in associations with gallstones
Thickened gall bladder with narrow lumen
US: How do gall bladder polyps appear?
Small intraluminal echogenic structure
Fixed to the gall bladder wall
does not cast an acoustic shadow
Common
Can be: inflammatory, cholesterol or adenomyomas
Cholesterol most common wth no malignant potential
US: How does adenomyomatosis appear?
gall bladder mucosa becomes hyperplastic and invaginates forming hypoechoic areaas called Rokitansky-Aschoff sinuses
These sinuses have tiny cholesterol deposits
Causes comet tail artefact
Lumen commonly narrowed from wall thickening
US: What are the appearances of gall bladder carcinoma?
Variable ultrasound appearances
- Solid mass occupying lumen
- Irregular polypoid mass with lumen
- Irregular thickening gall bladder wall, can be focal or diffuse
US: What is the normal pancreas appearance?
Homogeneous texture
Echogenicity is age related
Younger = bulky and hypoechoic
Adult = hyperechoic
Older = hyperechoic and tending to atrophy
Margin should be smooth
US: What is the scanning technique for visualising the pancreas?
Transverse plane in the epigastrium
Different angulations required for different views of the pancreas
Left lobe of the liver can act as an acoustic window
Align the transducer along the long axis of the pancreas to identify the anatomy
A fluid filled stomach can be used to see the tail of the pancreas
Need to see: uncinate process, head, body and tail
US: What are the pathologies of the pancreas that can be seen?
Pancreatitis +/- pseudocyst
Calculi
Pancreatic carcinoma
US: What is the appearance of pancreatitis?
Acute with bowel gas
May appear normal at the onset or quickly resolve
Assess for pseudocyst formation
Necrotising pancreatitis may have focal complex lesions
Enlarged oedematous gland +/- focal/lobular lesions
Free fluid in the lesser sac or peritoneal spread of fluid
Reduced echogeniciy
US: What is the pancreatic pseduocycst appearance?
Echo free mass
New has thin walls, old has thicker walls
Complex internal contents
Irregular borders
May have multiple sites
US: What is the normal appearance of the kidneys?
Size 10-12cm
Smooth contour with bright line around
Cortex slightly brighter than medually pyramids
Collecting system appears bright and echogenic
Capsule is thin and highly reflective
Relectivity slightly less echogenic than the liver
Pyramids are echo poor areas in the cortex
US: What are the renal pathologies that are visible?
Renal cysts
Renal calculi
Hydronephrosis
Renal carcinoma
US: What are the renal cysts?
Echo poor circular area wiht posterior acoustic enhancement
US: What is the appearance of renal calculi?
Echogenic focus with posterior acoustic shadowing
US: What is the appearance of hydronephrosis?
Initially appears echogenic then echopoor
US: What is the appearance of renal dilation?
Echopoor area seen expanding the collecting system
US: What is the appearance of renal failure?
Maybe normal, increased or decreased in size
Increased echogenicity
US: Why are renal stones harder to distinguish?
the brightness of the collecting system can make it difficult
US: What is the spleen scanning technique?
Examined from the left lateral aspect
Coronal and transverse sectons are obtained with the patient supine/ left anterior oblique using an intercostal approach
Gental respiration so as not to obscure the image with lung tissue
US: What is the normal spleen appearance?
Homogenous echo texture
Smooth and mid-grey in echogenicity
Smooth margins and pointed inferior border
US: What are spenunculi and how do they appear?
Accessory spleen
Normal variant
Near splenic hilum
Usually 1-1.5cm in diameter
Can enlarge and function as a normal spleen
US: What are the splenic pathologies that can be seen?
Splenomegaly >13cm
Cysts - echopoor with PCE
Haemangiomas - well defined and echogenic
Calcifications
Abscesses
Trauma
Malignancy
What may be the cause of splenomegaly?
Non-specific sign
May be due to:
Trauma
Portal venous congestion
Systemic infection
Neoplastic conditions
Haematological disorders
US: What is the appearance of a spleen abscess?
Varies
From echo free to mixed with solid and cystic components
May contain septae and / or debris
What are the consequences of splenic trauma and what are their appearances?
Subcapsular haematoma
Extra-capsular haematoma
Splenic rupture - irregular area of reduced reflectivity
Acute haematomas - well or poorly defined cresent shaped areas of increased reflectivity
US: What are the appearances of the spleen in leukaemia?
Acute - may be slightly enlarged with reduced echogenicity
Chronic - grossly enlarged with reduced reflectivity
US: What is the appearance of lymphoma in the spleen?
Usually diffuse
Enlarged
Homogenous with decreased reflectivity
Appearances vary
US: How is a patient prepared for a gynae exam?
Full bladder
1-1.5 pints of water 1-1.5 hours before the exam
This moves bowel gas to enable the ovaries to be seen (uses the bladder as a window_
US: What transducer is used in a gynae US?
Curvilinear transabdominal 3-7MHz
OR
Curvilinear transvaginal 5-8MHz
US: What is the normal vagina appearance?
Thin walled muscular H structure
Can be used as a landmark during scanning
3 thin reflective echoes inferior to the urinary bladder
US: What are the 3 layers of the uterus and how do they appear on US?
Parametrium = outer serous layer. Highly reflective linear echo
Myometrium - low level homogenous echoes of muscular tissue
Endometrium = innter layer. Cavity lining. Changes throughout the menstrual cycle and in pregnancy
What are the 3 uterus positions?
Anteverted - most common. Cervix and vagina form a 90 degree angle
Anteflexed = the angle between cervix and vagina is less than 90 degrees. Visualisation is increased with bladder filling
Retroverted/retroflexed - uterine fundus is placed caudally and is a normal variant. Can result poor visualisation of endometrium TA (use TV)
What are the difference uterine variants?
Uterus develops from the fusion of the inferior aspec of the 2 Mullerian ducts at 4 weeks. Variants occur if this is disrupted
Didelphic - complete failure of fusion. 2 uteri each with separate cervical opening +/- double vagina
Bicornuate - partial fusion, double uterine cavities separated by a septum
Unicornuate - only one duct due to the abscence of paramesonephric duct
US: What is the normal appearance of the ovaries?
Low reflectivity of outline
Thin fibrous layer of tunica albuginea
Cortex contains follicles
Inner layer: medulla of connective tissue, contains vessels, strong reflectivity
Must label R and L
Often they are on different planes so can’t be seen together
US: Why use a TV probe?
Allows further evaluation of uterus and ovaries
Higher frequency transducer which increases resolution
Decreases the distance to the area of interest means reduction in penetration is not a problem
More detail
US: What are the uterus pathologies that are visible?
Myometrium - fibroids
Endometrium = endometrial carcinoma and polyps
US: What is the appearance of fibroids?
Well defined mass of altered echogenicity
May contain calcification
Necrosis would causes a decrease in echogenicity
US: What is the appearance of endometrial carcinoma?
TV scan
Increasingly common in postmenopausal women
Thickened or irregular endometrium
Loss of myo/endometrium differentiation
US: What is the normal thickness of the endometrium?
Less than 4mm
US: What is the appearance of polyps?
Echogenic area seen within the endometrial cavity
May be surrounded by fluid (makes it easier to see)
May see a feeder vessel with colour doppler
US: What are the ovarian pathologies?
Masses e.g. carcinoma
Cyst e.g. simple/haemorrhagic/dermoid
Functional - polycystic ovarian syndrome
US: How does a simple ovarian cyst appear?
Well defined
Echo free
Unilocular
Thin smooth walls
US: What components of a cyst need to be considered?
Uni/multi-locular?
Solid?
Cystic?
Papillary proliferations?
Septae?
US: How does a haemorrhagic ovarian cyst appear?
Appearance varies with time
Diffuse homogenous low level echoes, septated, clot retraction
US: What are the features of a benign mass?
Unilocular cyst
Presence of a solid component less than 7mm
Presence of acoustic shadowing
Smooth multilocular tumour <100mm
No blood flow
US: what are the features of a malignant ovarian tumour?
Irregular
Solid
Ascites
At least 4 papillary structures
Irregular multilocular solid tumour>100mm
very strong blood flow
US: What is the appearance of endometriotic cyst?
Filled with homogenous low level echoes
No loculations or solid elements
Same internal echogenicity throughout
Maybe depositsof endometrium in the pelvis
US: What are the features of polycystic ovaries?
Increased ovarian volume > 10ml
Follicle number >12
Follicle diamete 2-9mm
What are the features of a dermoid ovarian cyst?
Cystic teratoma
Tumour composed of a number of tissue e.g. skin, hair follicles and sweat glands
Complex mass of different echogenicity and appearance
US: What are the reasons for thyroid ultrasound referral?
Palpable mass
abnormal thyroid function test
Biopsy of fine needle aspiration
US: What is the technique for imaging the thyroid?
Patient supine with neck extended
TS and LS of entire gland from carotid to trachea
If it extends retrosternally, scan during swallowing to lift above the thoracic inlet
Should include vessels and nodes in the neck
US: What probe should you use to image the thyroid?
Linear probe 7-17MHz
If patient is large use a lower frequency curvilinear
US: What is the normal appearance of the thyroid?
Homogeneous echotexture
Greater reflectivity than adjoining musculature
Thin reflective capsule
Vascular structures may be visible
In LS - lobes appear oval with a slender elongated upper pole and rounded inferior pole
Can have normal colloid cysts
What is the role of US in the thyroid?
Identify signs associated with malignancy
Visualisation of infiltration/spread to lympth nodes
Small lesion detection
Locating nodules for FNA and biopsy
Enables histological evaluation
US: What are the thyroid pathologies that are visible?
Masses - cyst/carcinoma
Thyroiditis
Multi-nodular goitre
US: What are the appearances of a benign nodule of the thyroid?
Isoechoic or hypoechoic
Well defined borders
Echo poor halo
May have cystic components - can be colloid or haemorrhage
May be heterogeneous
Comet tail artefact may be present
Perinodular blood flow pattern
Smooth walls, well defined
US: What is the appearance of thyroiditis?
Enlarged gland
Heterogeneous
Mixed echogenicity
Increased blood flow
US: What is the appearance of thyroid malignancy?
Predominantly hypoechoic
70% solid 30% cystic component
Microcalcifications
Intranodular blood flow pattern
US: What are the indications for referral for aorta US?
pulsatile mass
acute abdomen +/- back pain, collapse or trauma
Screening
Monitoring of AAA
Post-op complications
US: What is the scanning technique for the aorta?
Easiest to find in TS 30-40mm above the umbilicus
Assess whole length from diaphragm to bifurcation
Look for origin or renal arteries
Ensure TS image is as round as possible
US: How do you locate the renal arteries?
SMA may be used as a landmark
Adapt technique to improve visualisation
Use the right lobe of the liver or the right kidney as an acoustic window
Right anterior oblique view
Sometimes called a rose-thorn view
US: What is the scanning technique for a LS of aorta?
Turn transducer 90 degrees
Assess from diaphragm to bifurcation
Identify SMA and coeliac axis
US: What is the normal appearance of the aorta?
In TS - posterior to IVC, superior to renal arterie.
Circular in shape
Coeliac axis and branches appear like gull’s wings
Anechoic vessel with highly reflective border
Follows the spine and tapers inferiorly
On LS coeliac axis arises from aterio-superior aspect with SMA seen below that following the course of the aorta
US: What measurements of the aorta should be taken?
Measure just inferior to the renal arteries unless worried about AAA then measure at widest point
TS - must be a 90 degrees (no salami slice)
Measure antero-posteior inner edge to the inner edge in LS and TS
Normal <3cm in diameter
US: What is the appearance of AAA?
In LS aorta > 3cm
Loss of smooth tapering shape
Usually seen central, anehoic true lumen surrounded by more echogenic thrombus
Thrombus may calcify
In TS large, roundish mass with anechoic true lumen
Thrombus may be irregular / thickened
If >5.5cm consider for surgery
How do the different tissues appear on abdominal x ray?
Gas = black Fat = dark grey
Soft tissue = light grey
Bone = white
Metal artefacts = white
AXR: What can the location of organs depend on?
Anatomical location
Affect on anatomical postion of body habitus
Affect on anatomical position due to patient position and motility of organs
AXR: What fat stripes are visible?
Properitoneal fat stripe - outlines ascending and descending colon
Can also see the fat stripes of abdominal wall separating muscles
What are the 9 areas of the abdomen?
R and L hypochondriac
Epigastric
R and L lumbar
Umbilical
R and L iliac
Hypogastric
AXR: What are the 4 different types of body habitus? How common are they?
Hypersthenic 5%
Sthenic 50%
Hyposthenic 35%
Asthenic 10%
Describe the hypersthenic body habitus?
Heart is nearly transverse
Lungs are short
Apices at or near the clavicles
Diaphragm is high
Stomach is high, transverse and central
Colon is high around the periphery
Describe the sthenic body habitus
Heart moderately transverse
lungs are moderate length
diaphragm is moderately high
stomach is high upper left
colon spread evenly
Describe the asthenic body habitus
heart nearly vertical at the midline
lungs are long
apices are above the clavicles
diaphragm is low
stomach is low and medially (in pelvis on standing)
colon is low and folds on itself
What are the differences between supine and erect abdominal radiographs?
Supine are easier to review, abdo contents more evenly spread and is of more uniform thickness
Erect - abdo wall sags and is no longer of uniform thickness
AXR: Describe the appearance of barium and air in the stomach in erect, prone, supine and lateral images
Erect and prone - air rises to the top, barium sinks to the bottom
In supine, the air is squashed down at the bottom
In lateral the air is concentrated to the centre of the stomach with barium at the top and bottom
AXR: What is the distribution of air and barium in the large intestine when supine and prone
SUPINE - air in the transverse colon and sigmoid as well as base of stomach
PRONE - air in the ascending and descending colon
AXR: WHat should be considered to determine the patient position and direction of x-ray beam?
Position of contrast agent
Bony appearances
Action of gravity
Anatomical differences between right and left
AXR: What additional factors determine position of abdominal contents?
Phase of respiration
Loss of muscle tone
presence of pathology
Age
Quantity of contents in hollow viscera
AXR: What should an initial inspection check?
Correct patient and date of examination
Correct markers
Correct area
Optimum contrast
Optimum density
Resolution
Artefacts
Collimation
Are repeats required?
Pathology
AXR: What are the 5 areas of interest to check?
Abdominal gas pattern
Biliary tree and right urinary tract
Left urinary tract and bladder
Bones
Soft tissues
AXR: What are the 3 types of abnormality?
Opacity - area of decreased image density
Radiolucency - area of increased image density
Distortion and displacement
AXR: What is the standard projection for GI X-ray?
AP with patient supine
AXR: What are the upper limits of the normal diameter of:
Small bowel
Colon
Caecum
Small bowel = 3cm
Colon = 6cm
Caecum = 9cm
AXR: What are the defining features of the small bowel?
NO haustra
Valvulae conniventes
Many loops
Small radius of curvature
Loops are CENTRAL
3-5cm dimeter
No solid faeces
AXR: What are valvulae conniventes?
Mucosal folds that cross the full width of the bowel
Only found in the small intestine
AXR: What are the defining features of the large bowel?
Haustra (but not in sigmoid)
NO valvulae conniventes
Few loops
Large radius of curvature
Loops are peripheral
5cm diameter loops
Solid faeces
Have Taenia coli
AXR: What are the pathologies that can be found in the biliary tree and urinary tracts?
Increased opacity in = gall stones, renal calculi and ureteric calculus
Increased radiolucency = gas in the biliary tree
Distortion = size and the shape of the kidney
AXR: Where are the possible areas that calcification can occur?
Adrenal
Renal
Gall bladder
Pancreas
Aortic aneurysm
Fibroid
Bladder
Prostatic
US: What are the relations of the ovary that can be seen?
Ovary, dominant follicle, follicles, bladder.
anteriorly: broad ligament, mesovarium, ovarian vessels, obliterated umbilical vein
posteriorly: ureter, internal iliac vessels, pelvic wall
superiorly: external iliac vessels
inferiorly: levator ani
medially: ovarian ligament
laterally: obturator vessels and nerves
US: What is the appearance of the ovaries?
homogenous echotexture with a central echogenic medulla
volume on ultrasound can be calculated with following formula 5:
0.523 x length (cm) x width (cm) x depth (cm)
What are the relations of the vagina that can be seen?
anteriorly - cervix, bladder, urethra
posteriorly - pouch of Douglas, Denonvillier’s fascia, perineal body
laterally - levator ani, pelvic fascia, ureters
What are the relations of the uterus?
anteriorly - bladder; uterovesical pouch
posteriorly - rectum; pouch of Douglas
laterally - broad ligament; uterine vessels
uterine tubes open into its upper part
inferiorly - uterine cavity communicates with that of the vagina


