Pathology-Renal & Urinary Flashcards
When performing a FAST exam on your fellow med student you are having difficulty finding his kidneys. Eventually you find them more centrally located in the abdomen. What congenital malformation would cause the kidneys to be located in this position?
Horseshoe kidneys stop ascending during fetal development because they get snagged on the inferior mesenteric artery.
A mother brings her 2 year old boy in to see you complaining of constipation over the last week. Radiographs reveal an enlarged right kidney that is obstructing bowel and causing the child to be constipated. What congenital malformation may cause this radiographic finding?
Unilateral agenesis, in this case of the left kidney. The right kidney hypertrophies due to hyper filtration from trying to do the work of two kidneys.
A pregnant mother comes to see you because she has not felt her baby kick for the past 3 days. She is 30 weeks along and very concerned. Physical exam reveals minimal amniotic fluid. You determine that the fetus is dead and help her in delivery. The child is seen below. Autopsy reveals underdeveloped lungs. Why did this child not survive?

This child has bilateral renal agenesis that causes oligohydramnios. The child’s symptoms are in line with the classic Potter sequence (flattened face, lowered ears, pulmonary hypoplasia and malformations of the extremities).
A mother comes to your office for her 20 week pregnancy ultrasound. Visualization of the child reveals abnormal facies, shortened extremities and pulmonary hypoplasia. Both kidneys are there, however, cysts are observed bilaterally. There is no family history of cystic kidney disease on either side of the family. What would you expect to find in this neonate if you biopsied one of the cysts?
Dysplastic kidney disease characterized by abnormal tissue (cartilage as seen below) in the renal parenchyma. Dysplastic kidney disease is not inheritable.

A mother brings her 14 year old girl in to see. She complains of bilateral flank pain and a headache. Physical exam reveals hypertension, a mid-systolic click on the cardiac exam and hematuria. Several family members have similar symptoms. What is most likely causing her symptoms?
Autosomal dominal PKD. This is a mutation in APKD1 or APKD2 that causes polycystin to build up and create cysts in the kidney. AD PKD is also associated with berry aneurisms (headache), hepatic cysts and mitral valve prolapse (murmur).

A newborn baby is brought to your office due to jaundice, flattened facies, pulmonary hypoplasia and shortening of the extremities. Physical exam reveals a blood pressure of 120/80. what is your diagnosis?
Autosomal recessive PKD. This child is in renal failure. Bilateral cysts development in the kidneys makes them non-functional and causes newborns to present with oligohydramnios. Cysts also develop on the liver in this disease, causing hepatic fibrosis and jaundice.
A mother brings her 8 year old boy in to see you complaining of hematuria. Urinalysis reveals proteinuria and physical exam reveals hypertension. The father had a similar condition when he was a child and needed double kidney transplantation. Ultrasonography reveals shrunken kidneys. Where are you most likely to find the pathology when getting a CT of this patient?
This is medullary cystic kidney disease. It presents with renal failure, parenchymal fibrosis and shrunken kidneys. You would find cysts in the medullary collecting ducts on CT.
What are the hallmark presentations of acute renal failure?
Azotemia (increased nitrogenous waste like BUN) and oliguria (decreased urine production)
In what ways can people develop acute renal failure?
Decreasing blood flow (pre-renal azotemia), decreasing outflow of urine (post-renal azotemia) and decreased function within the kidney (intrarenal azotemia)
A 77 year old male comes to the ED due to increasing dyspnea over the past few days. He has a history of heart failure. He also complains of recent oliguria, confusion and dry mouth. Blood analysis reveals a BUN:Cr ratio of 25. What is your diagnosis and what is causing this patients blood work to manifest this way?
This patient has pre-renal azotemia from decreased blood flow to the glomerulus due to heart failure. The BUN:Cr ratio is elevated because the glomerulus senses decreased flow and sends out renin, which in turn causes secretion of aldosterone. Aldosterone acts on the nephron to resorb more water and Na+. Additional BUN gets resorbed in the process. This causes the BUN:Cr ratio in the blood to go up because Cr is still being filtered at a constant rate and cannot be resorbed.
A 44 year old male presents to the ED in septic shock. Once he is stabilized you run some blood work to see how everything is going. You note the patient has an elevated BUN:Cr ratio in the blood. He also complains of oliguria. Further analysis reveals a decreased eGFR. What would you expect to see in analysis of renal tubular function in this patient?
This patient is presenting with acute pre renal azotemia (decreased eGFR, azotemia, oliguria and increased BUN:Cr). Since its pre-renal, you know his tubular function remains intact and his FENa (Fractional Excretion of Na+ indicates how well the tubules are able to resorb Na+) < 1% and urine osmolality > 500 (tubules have ability to concentrate the urine)
A patient presents to the ED with excruciating flank pain. He also complains of oliguria and confusion. Renal ultrasound reveals a renal calculus in the right ureter. What lab values would you expect to see if you analyzed this patient’s BUN:Cr ratio in the blood, FENa and urine osmolality?
This is an acute post-renal azotemia. This presents with a BUN:Cr blood ratio > 15, a normal FENa < 1% and a normal urine osmolality > 500.
A patient presents to the ED with excruciating flank pain. He also complains of oliguria and confusion. Renal ultrasound reveals a renal calculus in the right ureter. The doctor says the calculus should pass on its own and sends the patient home. What lab values would you expect to see if you analyzed this patient’s BUN:Cr ratio in the blood, FENa and urine osmolality a week later and the calculus was still blocking the ureter?
Long-standing post-renal obstruction leads to tubular epithelium damage. This results in decreased resorption of BUN and Na+. Lab values would reveal a decreased BUN:Cr blood ratio and an FENa > 2%. Additionally, renal tubular damage limits the kidney’s ability to concentrate urine and osmolality < 500.
What is the most common cause of acute renal failure?
Acute Tubular Necrosis
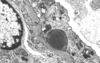
What change would you expect to see in the eGFR of the patient whose renal biopsy is shown below. What would you expect to see in his UA?

This is acute tubular necrosis. Note the anucleate epithelial cells that have sloughed from their basement membrane into the tubular lumen. This causes blockade of the tubule and decreases GFR due to back pressure. Clumping of the necrotic cells will manifest as brown granular casts excreted in the urine.

What portions of the nephron are particularly susceptible to ischemic acute tubular necrosis?
The proximal tubule and medullary segment of the thick ascending limb do a lot of reabsorption and need a lot of energy. In the case of decreased pre-renal blood supply, these are typically the first cells to go.
A patient presents to your clinic with a blood pressure of 100/60, when he is normally hypertensive. If further examination of this patient reveals nephrotoxic acute tubular necrosis, where is the most likely site of damage and what are the most likely agents?
The proximal tubule does most of the resorption and is most susceptible to nephrotoxic agents. These agents include aminoglycosides, heavy metals, myoglobinuria, ethylene glycol (antifreeze), radiocontrast dye and urate.
A panicked parent brings his 2 year old son to the ED because he was stumbling around the house and lost consciousness for a couple of minutes. This has never happened before and happened suddenly. Urine analysis reveals oxalate crystals. What is the most likely cause of this child’s symptoms? What else would you expect to see in the child’s urine analysis and blood work?
Antifreeze (ethylene glycol) has a sweet taste and kids may mistake it for juice. It is nephrotoxic and causes acute tubular necrosis. Acute tubular necrosis presents with elevated BUN and creatinine levels (due to inability to create a GFR due to blockade). Patients also become hyperkalemic (due to decreased K+ excretion) and acidotic (due to increased anion gap from decreased excretion of organic anions).
Why would you give a patient allopurinol prior to chemotherapy?
Chemotherapy causes rapid lysis of cancer cells. This results in a large release of uric acid that can damage the kidneys, causing acute tubular necrosis.
Why do you need to put a patient on dialysis if they have acute tubular necrosis? How long might they be on dialysis for?
Electrolyte imbalances created by tubular necrosis can be fatal. The tubular cells are stable cells. This means they can re-enter the cell cycle and regenerate, but it takes 2-3 weeks. Oliguria may persist that long and continue the need for dialysis.
A 67 year old man is admitted to the hospital for pneumonia. He has a history of heart failure and arthritis. He is given penicillin for the pneumonia and takes furosemide and ibuprofen regularly. He recovers within 2 days and is sent home and told to continue his antibiotics. A week later he develops a fever, rash and oliguria. Renal biopsy is shown below. What would you expect to see in this patient’s urine?

Note the tubules in the kidney look fine, but there is an inflammatory infiltrate in the interstitium. NSAIDs, penicillin and diuretics are the most common causes of acute interstitial nephritis. They induce a hypersensitivity reaction that causes inflammation of the renal interstitium and tubules. The common finding in the patient’s urine would be eosinophils.

A 19 year old female comes to the ED complaining of hematuria and flank pain. History only reveals a broken vertebra for which she has been taking aspirin for the past month or so. What is likely causing her symptoms?
A drug-induced hypersensitivity reaction that causes acute interstitial nephritis. Continued damage can result in renal papillary necrosis, which is seen in this patient.
What are the common causes of renal papillary necrosis?
Chronic analgesic abuse (aspirin/phenacetin), diabetes, sickle cell and severe acute pyelonephritis.
What is the definition of nephrotic syndrome?
A glomerular disorder resulting in proteinuria > 3.5g/day
Why do patients with nephrotic syndrome present with edema, increased infection, increased DVT and increased CAD?
Edema = hypoalbuminemia, Increased infection = hypogammaglobulinemia, DVT = excretion of anti-thrombin III, CAD = hyperlipidemia & hypercholesterolemia
You are doing rounds in the oncology wards and see a 12 year old boy with Hodgkin lymphoma. Physical examination reveals edema and hypertension for his age. What is likely causing the symptoms in this child? How would you treat him?
MCD (Minimal Change Disease) is the most common cause of nephrotic syndrome in children. It is normally idiopathic but can also be associated with Hodgkin lymphoma due to Reed-Sternberg cells. These B cells secrete tons of cytokines that damage the podocytes in the glomerulus. These patients have an excellent response to steroids due to decreased production of cytokines.
What are you likely to see on histological analysis of a patient’s renal tissue who has MCD?
Normal H&E stain. Negative immunofluorescence. Effacement of podocyte foot processes on EM.

Why do patients with MCD usually present with edema, but no increase in infections?
Selective proteinuria: loss of albumin but not of immunoglobulin.
What is the most common type of nephrotic syndrome in Hispanics and African Americans? What conditions is this condition associated with?
Focal Segmental Glomerular Sclerosis (FSGS). Normally it is idiopathic, but can be associated with HIV, heroin use and sickle cell disease.
A 32 year old African American male comes to see you. He has a history of HIV and heroin use. He also has sickle cell disease. He complains of recent edema in his face, arms and lower legs. He also says his blood pressure keeps going up. What would you expect to see on histological examination of this patient’s kidney?
FSGS. H&E would reveal focal (only a few glomeruli) and segmental (only part of the glomeruli) sclerosis. EM would reveal effacement of the podocyte pedicels. Immunofluorescence would be negative.

You suspect a patient has nephrotic syndrome due to minimal change disease. He has Hodgkin’s lymphoma so your attending physician gives you the go-ahead to try steroid therapy. How will this patient’s condition progress if he is not responsive to steroid therapy?
This means that he does not have MCD and will progress to FSGS and eventually to chronic renal failure.
What is the most common cause of nephrotic syndrome in caucasian adults? What other conditions is this condition associated with?
Membranous nephropathy. It is usually idiopathic, but can be associated with Hep B, Hep C, solid tumors, SLE or drugs (NSAIDs & penicillamine)
What is the most common disorder that presents in the kidneys of patients with lupus?
Diffuse proliferative glomerulonephritis
A patient comes to see you complaining of high blood pressure, a couple of DVTs in the past year, peripheral edema and increased pulmonary infections. Physical exam only reveals a malar rash and history reveals UV sensitivity. What is most likely causing this patient’s condition? What would you expect to see on histological examination of the patient’s kidney?
When patients with lupus present with nephrotic syndrome it is usually membranous nephropathy. On H&E you would see thickening of the glomerular basement membrane, granular immune complex deposition on immunofluorescence and subepithelial deposits with a “spike and dome” appearance on EM (from collagen deposition on top of immune complex on basement membrane).

A 45 year old male comes to see you complaining of increased peripheral edema, respiratory infections and DVTs in the past year. Physical exam reveals high blood pressure. PMH reveals hepatitis C. What may be causing this patient’s nephrotic syndrome and what would you expect to see on histological examination of his kidneys?
Membranoproliferative glomerulonephritis. H&E will show thick capillary membranes with a “tram-track” appearance (from mesangial cell plasma membrane proliferation splitting the immune complex deposit in half). Granular immune complex deposition in the endothelium and basement membrane will be seen on immunofluorescence.
What are the two different types of membranoproliferative glomerulonephritis? What conditions are they commonly associated with?
Type I = subendothelial immune complex deposits (associated with Hep B & Hep C). Type II = basement membrane immune complex deposits (C3 nephritic factor stabilizing C3 convertase)
Which type of membranoproliferative glomerulonephritis is more often associated with the “tram-track” appearance?
Type I (subendothelial deposits).
How do patients with C3 nephritic factor develop membranoproliferative glomerulonephritis?
C3 nephritic factor (an antibody) stabilizes C3 convertase. This is the enzyme that converts C3 to C3a & C3b. Stabilizing this enzyme results in over activation of complement, inflammation and damage to the glomerulus.